Abstract
Objective
To evaluate the environmental and economic impact of teleophthalmological services provided by a primary (rural) and tertiary (urban) eyecare network in India.
Methods
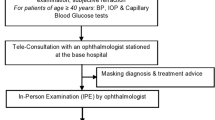
This prospective study utilised a random sampling method, and administered an environmental and economic impact assessment questionnaire. The study included 324 (primary: 173; tertiary: 151) patients who received teleconsultations from July to September 2022. The primary network (rural) used a colour-coded triage system (Green: eye conditions managed by teleconsult alone; yellow: semi-urgent referral within 1 week to a month, red: urgent referral within a day to a week). The tertiary network (urban) included new and follow-up patients. The environmental impact was assessed by estimating the potential CO2 emissions saved by avoiding travel for various transport modes. Economic impact measured by the potential cost savings from direct (travel) and indirect (food and wages lost) expenses spent by yellow and red referrals (primary) and the first-visit expenses of follow-up (tertiary) patients.
Results
The primary rural network saved 2.89 kg CO2/person and 80 km/person. The tertiary urban network saved 176.6 kg CO2/person and 1666 km/person. The potential cost savings on travel expenses were INR 19,970 (USD 250) for the primary (average: INR 370 (USD 4.6) per patient) and INR 758,870 (USD 9486) for the tertiary network (average: INR 8339 (USD 104) per patient). Indirect cost savings (food and wages) were of INR 29,100 (USD 364) for the primary and INR 347,800 (USD 4347) for the tertiary network.
Conclusion
Teleophthalmology offers substantial environmental and economic benefits in rural and urban eyecare systems.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article and its Supplementary Information files.
References
Dasgupta A, Deb S. Telemedicine: a new horizon in public health in India. Indian J Community Med. 2008;33:3–8.
Dolar-Szczasny J, Baranska A, Rejdak R. Evaluating the efficacy of teleophthalmology in delivering ophthalmic care to underserved populations: a literature review. J Clin Med. 2023;12:3161.
Ullah W, Pathan SK, Panchal A, Anandan S, Saleem K, Sattar Y, et al. Cost-effectiveness and diagnostic accuracy of telemedicine in macular disease and diabetic retinopathy: a systematic review and meta-analysis. Medicine. 2020;99:e20306.
Kumari Rani P, Raman R, Manikandan M, Mahajan S, Paul PG, Sharma T. Patient satisfaction with tele-ophthalmology versus ophthalmologist-based screening in diabetic retinopathy. J Telemed Telecare. 2006;12:159–60.
Sim DA, Mitry D, Alexander P, Mapani A, Goverdhan S, Aslam T, et al. The evolution of teleophthalmology programs in the United Kingdom: beyond diabetic retinopathy screening. J Diabetes Sci Technol. 2016;10:308–17.
Veeramani P, Pilar Martin-Gutierrez M, Agorogiannis E, Hamilton R, Griggs T, Nicholson L, et al. Efficacy and safety outcomes of a novel model to assess new medical retina referrals in a high-volume medical retina virtual clinic. Eye (Lond). 2024;38:168–72.
Christy B, Mahalakshmi M, Aishwarya TV, Jayaraman D, Das AV, Rani PK. Tele-rehabilitation for persons with vision impairment during COVID-19: experiences and lessons learned. Indian J Ophthalmol. 2022;70:1026–9.
Dullet NW, Geraghty EM, Kaufman T, Kissee JL, King J, Dharmar M, et al. Impact of a university-based outpatient telemedicine program on time savings, travel costs, and environmental pollutants. Value Health. 2017;20:542–6.
Roan VD, Sun KJ, Valentim CCS, Bheemidi AR, Iyer A, Singh RP, et al. Patient satisfaction in the era of COVID-19: virtual visit versus in-person visit satisfaction. Optom Vis Sci. 2022;99:190–4.
Purohit A, Smith J, Hibble A. Does telemedicine reduce the carbon footprint of healthcare? A systematic review. Future Health J. 2021;8:e85–91.
Ravindrane R, Patel J. The environmental impacts of telemedicine in place of face-to-face patient care: a systematic review. Future Health J. 2022;9:28–33.
Komal S, Radhakrishnan N, Vardhan SA, Prajna NV. Effectiveness of a tele-ophthalmology vision center in treating corneal disorders and its associated economic benefits. Cornea. 2022;41:688–91.
Rao GN, Khanna RC, Athota SM, Rajshekar V, Rani PK. Integrated model of primary and secondary eye care for underserved rural areas: the L V Prasad Eye Institute experience. Indian J Ophthalmol. 2012;60:396–400.
Kammari P, Ambadker MC, Loomba A, Deepthi N, Shravani M, Vadapalli R, et al. A novel technology tool to capture the clinical information of patients across rural vision centers in a three-tier eye care network in India using the eyeSmart EMR App. Rural Remote Health. 2019;19:5255.
Das AV, Rani PK, Vaddavalli PK. Tele-consultations and electronic medical records driven remote patient care: responding to the COVID-19 lockdown in India. Indian J Ophthalmol. 2020;68:1007–12.
Rani PK, Das AV. Setting up a primary eye care teleconsultation service. Community Eye Health. 2022;35:6–7.
Lange O, Plath J, Dziggel TF, Karpa DF, Keil M, Becker T, et al. A transparency checklist for carbon footprint calculations applied within a systematic review of virtual care interventions. Int J Environ Res Public Health. 2022;19:7474.
Tennison I, Roschnik S, Ashby B, Boyd R, Hamilton I, Oreszczyn T, et al. Health care’s response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. 2021;5:e84–92.
Wong YL, Noor M, James KL, Aslam TM. Ophthalmology going greener: a narrative review. Ophthalmol Ther. 2021;10:845–57.
Das AV, Khanna RC, Kumar N, Rani PK. Impact of implementing teleophthalmology referral guidelines using the eyeSmart EMR App in 63,703 patients from India. Int J Telemed Appl. 2022;2022:8523131.
Andrews E, Pearson D, Kelly C, Stroud L, Rivas Perez M. Carbon footprint of patient journeys through primary care: a mixed methods approach. Br J Gen Pr. 2013;63:e595–603.
Nicolet J, Mueller Y, Paruta P, Boucher J, Senn N. What is the carbon footprint of primary care practices? A retrospective life-cycle analysis in Switzerland. Environ Health. 2022;21:3.
Nikolaidou A, Tsaousis KT. Teleophthalmology and artificial intelligence as game changers in ophthalmic care after the COVID-19 pandemic. Cureus. 2021;13:e16392.
Paquette S, Lin JC. Outpatient telemedicine program in vascular surgery reduces patient travel time, cost, and environmental pollutant emissions. Ann Vasc Surg. 2019;59:167–72.
Muschol J, Heinrich M, Heiss C, Knapp G, Repp H, Schneider H, et al. Assessing telemedicine efficiency in follow-up care with video consultations for patients in orthopedic and trauma surgery in Germany: randomized controlled trial. J Med Internet Res. 2022;24:e36996.
Funding
Hyderabad Eye Research Foundation, Hyderabad, India.
Author information
Authors and Affiliations
Contributions
Study concept and design: PKR, RCK, RR, VMR, and PKV; Study conduct and data acquisition: PKR, SC, AKP, VST, VS, and VI; Data analysis: PKR and RR; Manuscript writing, editing, and review: PKR, RCK, RR, VMR, and PKV.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rani, P.K., Khanna, R.C., Ravindrane, R. et al. Teleophthalmology at a primary and tertiary eye care network from India: environmental and economic impact. Eye (2024). https://doi.org/10.1038/s41433-024-02934-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41433-024-02934-4