Abstract
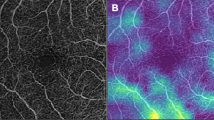
Cardiovascular disease (CVD) remains the leading cause of death worldwide. Assessing of CVD risk plays an essential role in identifying individuals at higher risk and enables the implementation of targeted intervention strategies, leading to improved CVD prevalence reduction and patient survival rates. The ocular vasculature, particularly the retinal vasculature, has emerged as a potential means for CVD risk stratification due to its anatomical similarities and physiological characteristics shared with other vital organs, such as the brain and heart. The integration of artificial intelligence (AI) into ocular imaging has the potential to overcome limitations associated with traditional semi-automated image analysis, including inefficiency and manual measurement errors. Furthermore, AI techniques may uncover novel and subtle features that contribute to the identification of ocular biomarkers associated with CVD. This review provides a comprehensive overview of advancements made in AI-based ocular image analysis for predicting CVD, including the prediction of CVD risk factors, the replacement of traditional CVD biomarkers (e.g., CT-scan measured coronary artery calcium score), and the prediction of symptomatic CVD events. The review covers a range of ocular imaging modalities, including colour fundus photography, optical coherence tomography, and optical coherence tomography angiography, and other types of images like external eye images. Additionally, the review addresses the current limitations of AI research in this field and discusses the challenges associated with translating AI algorithms into clinical practice.
摘要
心血管疾病(CVD)仍然是全球死亡的主要原因。评估CVD的风险在识别高风险个体方面发挥着重要作用, 并能够实施有针对性的干预策略, 从而降低CVD患病率并提高患者生存率。眼部血管, 特别是视网膜血管, 由于其与大脑和心脏等重要器官的解剖学和生理特征的相似性, 已成为CVD风险分层的潜在手段。将人工智能(AI)应用于眼科成像有可能克服传统半自动图像分析的局限性, 包括低效率和人工测量误差。此外, 人工智能技术有助于识别与CVD相关的眼部生物标志物的细微特征。本综述全面概述了基于AI的眼部图像分析在预测CVD方面取得的进展, 包括预测CVD 危险因素、代替传统CVD生物标志物(例如CT扫描测量的冠状动脉钙指标)以及预测症状性CVD疾病。本综述涵盖了一系列的眼部成像方式, 包括彩色眼底照相、光学相干断层扫描和光学相干断层扫描血管造影, 以及其他类型的图像, 如眼外部照相。此外, 综述提出了目前在该领域人工智能研究的局限性, 并讨论了将人工智能算法转化为临床实践的相关挑战。
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Cardiovascular diseases (CVDs)- World Health Organization. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed Aug 2023.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–934.
SCORE2 working group and ESC Cardiovascular risk collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42:2439–54.
Pylypchuk R, Wells S, Kerr A, Poppe K, Riddell T, Harwood M, et al. Cardiovascular disease risk prediction equations in 400 000 primary care patients in New Zealand: a derivation and validation study. Lancet. 2018;391:1897–907.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74:e177–e232.
Yadlowsky S, Hayward RA, Sussman JB, McClelland RL, Min Y-I, Basu S. Clinical implications of revised pooled cohort equations for estimating atherosclerotic cardiovascular disease risk. Ann Intern Med. 2018;169:20.
Ma Y, Xiong J, Zhu Y, Ge Z, Hua R, Fu M, et al. Deep learning algorithm using fundus photographs for 10-year risk assessment of ischemic cardiovascular diseases in China. Sci Bull. 2022;67:17–20.
Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013;382:1762–5.
Gariano RF, Gardner TW. Retinal angiogenesis in development and disease. Nature. 2005;438:960–6.
Patton N, Aslam T, MacGillivray T, Pattie A, Deary IJ, Dhillon B. Retinal vascular image analysis as a potential screening tool for cerebrovascular disease: a rationale based on homology between cerebral and retinal microvasculatures. J Anat. 2005;206:319–48.
Flammer J, Konieczka K, Bruno RM, Virdis A, Flammer AJ, Taddei S. The eye and the heart. Eur Heart J. 2013;34:1270–8.
Liew G, Wang JJ. Retinal vascular signs: a window to the heart? Rev Española de Cardiolía (Engl Ed). 2011;64:515–21.
Chua J, Chin CWL, Hong J, Chee ML, Le T-T, Ting DSW, et al. Impact of hypertension on retinal capillary microvasculature using optical coherence tomographic angiography. J Hypertens. 2019;37:572–80.
Zekavat SM, Raghu VK, Trinder M, Ye Y, Koyama S, Honigberg MC, et al. Deep learning of the retina enables phenome- and genome-wide analyses of the microvasculature. Circulation. 2022;145:134–50.
Wong TY, Klein R, Klein BE, Tielsch JM, Hubbard L, Nieto FJ. Retinal microvascular abnormalities and their relationship with hypertension, cardiovascular disease, and mortality. Surv Ophthalmol. 2001;46:59–80.
Wong TY, Mitchell P. Hypertensive retinopathy. N Engl J Med. 2004;351:2310–7.
McClintic BR, McClintic JI, Bisognano JD, Block RC. The relationship between retinal microvascular abnormalities and coronary heart disease: a review. Am J Med. 2010;123:374.e1–7.
Wang L, Wong TY, Sharrett AR, Klein R, Folsom AR, Jerosch-Herold M. Relationship between retinal arteriolar narrowing and myocardial perfusion: multi-ethnic study of atherosclerosis. Hypertension. 2008;51:119–26.
Tedeschi-Reiner E, Strozzi M, Skoric B, Reiner Z. Relation of atherosclerotic changes in retinal arteries to the extent of coronary artery disease. Am J Cardiol. 2005;96:1107–9.
Karanam VC, Tamariz L, Batawi H, Wang J, Galor A. Functional slit lamp biomicroscopy metrics correlate with cardiovascular risk. Ocul Surf. 2019;17:64–9.
Um J-Y, An N-H, Yang G-B, Lee G-M, Cho J-J, Cho J-W, et al. Novel approach of molecular genetic understanding of iridology: relationship between iris constitution and angiotensin converting enzyme gene polymorphism. Am J Chin Med. 2005;33:501–5.
Noorbakhsh-Sabet N, Zand R, Zhang Y, Abedi V. Artificial intelligence transforms the future of health care. Am J Med. 2019;132:795–801.
Çetinkaya MB, Duran H. A detailed and comparative work for retinal vessel segmentation based on the most effective heuristic approaches. Biomed Eng/Biomedizinische Tech. 2021;66:181–200.
Schmidt-Erfurth U, Sadeghipour A, Gerendas BS, Waldstein SM, Bogunović H. Artificial intelligence in retina. Prog Retin Eye Res. 2018;67:1–29.
LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521:436–44.
Abramoff MD, Lou Y, Erginay A, Clarida W, Amelon R, Folk JC, et al. Improved automated detection of diabetic retinopathy on a publicly available dataset through integration of deep learning. Invest Ophthalmol Vis Sci. 2016;57:5200–6.
Ting DSW, Cheung CY, Lim G, Tan GSW, Quang ND, Gan A, et al. Development and validation of a deep learning system for diabetic retinopathy and related eye diseases using retinal images from multiethnic populations with diabetes. JAMA. 2017;318:2211–23.
Gulshan V, Peng L, Coram M, Stumpe MC, Wu D, Narayanaswamy A, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA. 2016;316:2402–10.
Zhou Y, Wagner SK, Chia MA, Zhao A, Woodward-Court P, Xu M, et al. AutoMorph: automated retinal vascular morphology quantification via a deep learning pipeline. Transl Vis Sci Technol. 2022;11:12.
Welikala RA, Fraz MM, Habib MM, Daniel-Tong S, Yates M, Foster PJ, et al. editors. Automated quantification of retinal vessel morphometry in the UK biobank cohort. In: 2017 Seventh International Conference on Image Processing Theory, Tools and Applications (IPTA). Montreal, QC, Canada: IEEE; 2017. p. 1–6. Available from: https://ieeexplore.ieee.org/abstract/document/8310108.
Korot E, Wagner SK, Faes L, Liu X, Huemer J, Ferraz D, et al. Will AI replace ophthalmologists? Transl Vis Sci Technol. 2020;9:2.
Rim TH, Lee CJ, Tham YC, Cheung N, Yu M, Lee G, et al. Deep-learning-based cardiovascular risk stratification using coronary artery calcium scores predicted from retinal photographs. Lancet Digit Health. 2021;3:e306–e16.
Mordi IR, Trucco E, Syed MG, MacGillivray T, Nar A, Huang Y, et al. Prediction of major adverse cardiovascular events from retinal, clinical, and genomic data in individuals with type 2 diabetes: a population cohort study. Diabetes Care. 2022;45:710–6.
Poplin R, Varadarajan AV, Blumer K, Liu Y, McConnell MV, Corrado GS, et al. Prediction of cardiovascular risk factors from retinal fundus photographs via deep learning. Nat Biomed Eng. 2018;2:158–64.
Vaghefi E, Yang S, Hill S, Humphrey G, Walker N, Squirrell D. Detection of smoking status from retinal images; a Convolutional Neural Network study. Sci Rep. 2019;9:7180.
Zhang L, Yuan M, An Z, Zhao X, Wu H, Li H, et al. Prediction of hypertension, hyperglycemia and dyslipidemia from retinal fundus photographs via deep learning: a cross-sectional study of chronic diseases in central China. PLoS ONE. 2020;15:e0233166.
Zhu Z, Shi D, Guankai P, Tan Z, Shang X, Hu W, et al. Retinal age gap as a predictive biomarker for mortality risk. Br J Ophthalmol. 2023;107:547–54.
Zhu Z, Chen Y, Wang W, Wang Y, Hu W, Shang X, et al. Association of retinal age gap with arterial stiffness and incident cardiovascular disease. Stroke. 2022;53:3320–8.
Nusinovici S, Rim TH, Yu M, Lee G, Tham YC, Cheung N, et al. Retinal photograph-based deep learning predicts biological age, and stratifies morbidity and mortality risk. Age Ageing. 2022;51:afac065.
Rim TH, Lee G, Kim Y, Tham YC, Lee CJ, Baik SJ, et al. Prediction of systemic biomarkers from retinal photographs: development and validation of deep-learning algorithms. Lancet Digit Health. 2020;2:e526–e36.
Gerrits N, Elen B, Craenendonck TV, Triantafyllidou D, Petropoulos IN, Malik RA, et al. Age and sex affect deep learning prediction of cardiometabolic risk factors from retinal images. Sci Rep. 2020;10:9432.
Nagasato D, Tabuchi H, Masumoto H, Kusuyama T, Kawai Y, Ishitobi N, et al. Prediction of age and brachial-ankle pulse-wave velocity using ultra-wide-field pseudo-color images by deep learning. Sci Rep. 2020;10:19369.
Kooman JP, Kotanko P, Schols AM, Shiels PG, Stenvinkel P. Chronic kidney disease and premature ageing. Nat Rev Nephrol. 2014;10:732–42.
Balakumar P, Maung UK, Jagadeesh G. Prevalence and prevention of cardiovascular disease and diabetes mellitus. Pharmacol Res. 2016;113:600–9.
Sabanayagam C, Xu D, Ting DSW, Nusinovici S, Banu R, Hamzah H, et al. A deep learning algorithm to detect chronic kidney disease from retinal photographs in community-based populations. Lancet Digit Health. 2020;2:e295–e302.
Zhang K, Liu X, Xu J, Yuan J, Cai W, Chen T, et al. Deep-learning models for the detection and incidence prediction of chronic kidney disease and type 2 diabetes from retinal fundus images. Nat Biomed Eng. 2021;5:533–45.
Chang J, Ko A, Park SM, Choi S, Kim K, Kim SM, et al. Association of cardiovascular mortality and deep learning-funduscopic atherosclerosis score derived from retinal fundus images. Am J Ophthalmol. 2020;217:121–30.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73:e285–e350.
Goff DC Jr., Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S49–73.
Son J, Shin JY, Chun EJ, Jung KH, Park KH, Park SJ. Predicting high coronary artery calcium score from retinal fundus images with deep learning algorithms. Transl Vis Sci Technol. 2020;9:28.
Diaz-Pinto A, Ravikumar N, Attar R, Suinesiaputra A, Zhao Y, Levelt E, et al. Predicting myocardial infarction through retinal scans and minimal personal information. Nat Mach Intell. 2022;4:55–61.
Mok VC, Lam BY, Wong A, Ko H, Markus HS, Wong LK. Early-onset and delayed-onset poststroke dementia - revisiting the mechanisms. Nat Rev Neurol. 2017;13:148–59.
Lau AY, Mok V, Lee J, Fan Y, Zeng J, Lam B, et al. Retinal image analytics detects white matter hyperintensities in healthy adults. Ann Clin Transl Neurol. 2019;6:98–105.
Zee B, Wong Y, Lee J, Fan Y, Zeng J, Lam B, et al. Machine-learning method for localization of cerebral white matter hyperintensities in healthy adults based on retinal images. Brain Commun. 2021;3:fcab124.
Khan A, De Boever P, Gerrits N, Akhtar N, Saqqur M, Ponirakis G, et al. Retinal vessel multifractals predict pial collateral status in patients with acute ischemic stroke. PLoS ONE. 2022;17:e0267837.
Al-Absi HRH, Islam MT, Refaee MA, Chowdhury MEH, Alam T. Cardiovascular disease diagnosis from dxa scan and retinal images using deep learning. Sensors. 2022;22:4310.
Ma Y, Xiong J, Zhu Y, Ge Z, Hua R, Fu M, et al. Deep learning algorithm using fundus photographs for 10-year risk assessment of ischemic cardiovascular diseases in China. Sci Bull (Beijing). 2022;67:17–20.
Rudnicka AR, Welikala R, Barman S, Foster PJ, Luben R, Hayat S, et al. Artificial intelligence-enabled retinal vasculometry for prediction of circulatory mortality, myocardial infarction and stroke. Br J Ophthalmol. 2022;106:1722–9.
Dai G, He W, Xu L, Pazo EE, Lin T, Liu S, et al. Exploring the effect of hypertension on retinal microvasculature using deep learning on East Asian population. PLoS ONE. 2020;15:e0230111.
Mueller S, Wintergerst MWM, Falahat P, Holz FG, Schaefer C, Schahab N, et al. Multiple instance learning detects peripheral arterial disease from high-resolution color fundus photography. Sci Rep. 2022;12:1389.
Qu Y, Zhuo Y, Lee J, Huang X, Yang Z, Yu H, et al. Ischemic and haemorrhagic stroke risk estimation using a machine-learning-based retinal image analysis. Front Neurol. 2022;13:916966.
D’Agostino RB Sr., Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–53.
Gupta A. StrokeSave: a novel, high-performance mobile application for stroke diagnosis using deep learning and computer vision. Teknos Science Journal 2019.
Hassan ON, Menten MJ, Bogunovic H, Schmidt-Erfurth U, Lotery A, Rueckert D, editors. Deep learning prediction of age and sex from optical coherence tomography. In: 2021 IEEE 18th International Symposium on Biomedical Imaging (ISBI). Nice, France: IEEE; 2021. p. 238–42. Available from: https://ieeexplore.ieee.org/abstract/document/9434107.
Chueh KM, Hsieh YT, Chen HH, Ma IH, Huang SL. Identification of sex and age from macular optical coherence tomography and feature analysis using deep learning. Am J Ophthalmol. 2022;235:221–8.
Munk MR, Kurmann T, Márquez-Neila P, Zinkernagel MS, Wolf S, Sznitman R. Assessment of patient specific information in the wild on fundus photography and optical coherence tomography. Sci Rep. 2021;11:8621.
Nawaf Y, Leon F, Bruce CVC. Brain frailty and small vessel disease for stroke outcome prediction. Neurology. 2020;94:191.
Tschirret O, Moreno Legast G, Mansuy A, Mewton N, Buisson M, Hannoun S, et al. Impact of brain atrophy on early neurological deterioration and outcome in severe ischemic stroke treated by intravenous thrombolysis. Eur Neurol. 2018;79:240–6.
Appleton JP, Woodhouse LJ, Adami A, Becker JL, Berge E, Cala LA, et al. Imaging markers of small vessel disease and brain frailty, and outcomes in acute stroke. Neurology. 2020;94:e439–e52.
Tao W, Kwapong WR, Xie J, Wang Z, Guo X, Liu J, et al. Retinal microvasculature and imaging markers of brain frailty in normal aging adults. Front Aging Neurosci. 2022;14:945964.
Gandhi MM, Lampe FC, Wood DA. Incidence, clinical characteristics, and short-term prognosis of angina pectoris. Br Heart J. 1995;73:193–8.
Zhong P, Qin J, Li Z, Jiang L, Peng Q, Huang M, et al. Development and validation of retinal vasculature nomogram in suspected angina due to coronary artery disease. J Atheroscler Thromb. 2022;29:579–96.
Hwang J, Karanam V, Wang J, Feuer WJ, Garg RK, Tamariz L, et al. Conjunctival vessels in diabetes using functional slit lamp biomicroscopy. Cornea. 2021;40:950–7.
Bansal A, Agarwal R, Sharma RK. Determining diabetes using iris recognition system. Int J Diabetes Dev Ctries. 2015;35:432–8.
Wang TJ, Keller JJ, Sheu JJ, Lin HC. A 3-year follow-up study on the risk of stroke among patients with conjunctival haemorrhage. Acta Ophthalmol. 2013;91:226–30.
Brennan PF, McNeil AJ, Jing M, Awuah A, Moore JS, Mailey J, et al. Assessment of the conjunctival microcirculation for patients presenting with acute myocardial infarction compared to healthy controls. Sci Rep. 2021;11:7660.
Khalifa NE, Taha M, Hassanien AE, Mohamed H. Deep Iris: deep learning for gender classification through iris patterns. Acta Inform Med. 2019;27:96.
Samant P, Agarwal R. Machine learning techniques for medical diagnosis of diabetes using iris images. Comput Methods Prog Biomed. 2018;157:121–8.
Awuah A, Moore JS, Nesbit MA, Ruddock MW, Brennan PF, Mailey JA, et al. A novel algorithm for cardiovascular screening using conjunctival microcirculatory parameters and blood biomarkers. Sci Rep. 2022;12:6545.
Babenko B, Mitani A, Traynis I, Kitade N, Singh P, Maa AY, et al. Detection of signs of disease in external photographs of the eyes via deep learning. Nat Biomed Eng. 2022;6:1370–83.
Babenko B, Traynis I, Chen C, Singh P, Uddin A, Cuadros J, et al. A deep learning model for novel systemic biomarkers in photographs of the external eye: a retrospective study. Lancet Digit Health. 2023;5:e257–e64.
Hubbard LD, Brothers RJ, King WN, Clegg LX, Klein R, Cooper LS, et al. Methods for evaluation of retinal microvascular abnormalities associated with hypertension/sclerosis in the Atherosclerosis Risk in Communities Study. Ophthalmology. 1999;106:2269–80.
Wong TY, Knudtson MD, Klein R, Klein BE, Meuer SM, Hubbard LD. Computer-assisted measurement of retinal vessel diameters in the Beaver Dam Eye Study: methodology, correlation between eyes, and effect of refractive errors. Ophthalmology. 2004;111:1183–90.
Cheung CY, Hsu W, Lee ML, Wang JJ, Mitchell P, Lau QP, et al. A new method to measure peripheral retinal vascular caliber over an extended area. Microcirculation. 2010;17:495–503.
McGrory S, Taylor AM, Pellegrini E, Ballerini L, Kirin M, Doubal FN, et al. Towards standardization of quantitative retinal vascular parameters: comparison of SIVA and VAMPIRE measurements in the Lothian Birth Cohort 1936. Transl Vis Sci Technol. 2018;7:12.
Tapp RJ, Owen CG, Barman SA, Welikala RA, Foster PJ, Whincup PH, et al. Associations of retinal microvascular diameters and tortuosity with blood pressure and arterial stiffness: United Kingdom Biobank. Hypertension. 2019;74:1383–90.
Cheung CY, Xu D, Cheng CY, Sabanayagam C, Tham YC, Yu M, et al. A deep-learning system for the assessment of cardiovascular disease risk via the measurement of retinal-vessel calibre. Nat Biomed Eng. 2021;5:498–508.
Maurovich-Horvat P. Current trends in the use of machine learning for diagnostics and/or risk stratification in cardiovascular disease. Cardiovasc Res. 2021;117:e67–e9.
Xu J, Xue K, Zhang K. Current status and future trends of clinical diagnoses via image-based deep learning. Theranostics. 2019;9:7556–65.
Ruamviboonsuk P, Chantra S, Seresirikachorn K, Ruamviboonsuk V, Sangroongruangsri S. Economic evaluations of artificial intelligence in ophthalmology. Asia Pac J Ophthalmol. 2021;10:307–16.
Gao S, He L, Chen Y, Li D, Lai K. Public perception of artificial intelligence in medical care: content analysis of social media. J Med Internet Res. 2020;22:e16649.
Funding
The work was supported by National Key Research and Development Program of China (No. 2022YFC2502800).
Author information
Authors and Affiliations
Contributions
YH: manuscript writing; CYC (Carol Y Cheung): Concept and paper revision; DWL: Literature review and paper revision; YCT: Literature review and paper revision; BS: Literature review and paper revision; CYC (Ching Yu Cheng): Literature review and paper revision; YXW: Writing and paper revision; TYW: Concept, original presentation and revision. The corresponding authors have listed all authors who met the authorship criteria into the manuscript.
Corresponding author
Ethics declarations
Competing interests
TYW is a consultant for Aldropika Therapeutics, Bayer, Boehringer-Ingelheim, Genentech, Iveric Bio, Novartis, Oxurion, Plano, Roche, Sanofi, Shanghai Henlius. He is an inventor, holds patents and is a co-founder of start-up companies EyRiS and Visre, which have interests in, and develop digital solutions for eye diseases.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, Y., Cheung, C.Y., Li, D. et al. AI-integrated ocular imaging for predicting cardiovascular disease: advancements and future outlook. Eye 38, 464–472 (2024). https://doi.org/10.1038/s41433-023-02724-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02724-4