Abstract
Objective
To describe the clinical characteristics, outcomes, and management of a large cohort of patients with concomitant malignant arterial hypertension and intracranial hypertension.
Methods
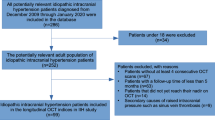
Design: Retrospective case series. Subjects: Patients aged ≥ 18 years with bilateral optic disc oedema (ODE), malignant arterial hypertension and intracranial hypertension at five academic institutions. Patient demographics, clinical characteristics, diagnostic studies, and management were collected.
Results
Nineteen patients (58% female, 63% Black) were included. Median age was 35 years; body mass index (BMI) was 30 kg/m2. Fourteen (74%) patients had pre-existing hypertension. The most common presenting symptom was blurred vision (89%). Median blood pressure (BP) was 220 mmHg systolic (IQR 199–231.5 mmHg) and 130 mmHg diastolic (IQR 116–136 mmHg) mmHg), and median lumbar puncture opening pressure was 36.5 cmH2O. All patients received treatment for arterial hypertension. Seventeen (89%) patients received medical treatment for raised intracranial pressure, while six (30%) patients underwent a surgical intervention. There was significant improvement in ODE, peripapillary retinal nerve fibre layer thickness, and visual field in the worst eye (p < 0.05). Considering the worst eye, 9 (47%) presented with acuity ≥ 20/25, while 5 (26%) presented with ≤ 20/200. Overall, 7 patients maintained ≥ 20/25 acuity or better, 6 demonstrated improvement, and 5 demonstrated worsening.
Conclusions
Papilloedema and malignant arterial hypertension can occur simultaneously with potentially greater risk for severe visual loss. Clinicians should consider a workup for papilloedema among patients with significantly elevated blood pressure and bilateral optic disc oedema.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
We agree to the data availability policy of the journal.
References
Chobanian AV, Bakris G, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. JAMA 2003;289:2560–72.
Shenchu Xie J, Donaldson L, Margolin E. Papilledema: a review of etiology, pathophysiology, diagnosis, and management. Surv Ophthalmol. 2022;67:1135–59.
Hammond S, Razor Wells J, Marcus DM, Prisant M. Ophthalmoscopic findings in malignant hypertension. J Clin Hypertens. 2005;8:221–3.
Mishra P, Dash N, Sahu S, Kanaujia V, Sharma K. Malignant hypertension and the role of ophthalmologists: a review article. Cureus 2022;14:e27140.
Hayreh SS, Servais GE, Virdi PS. Fundus lesions in malignant hypertension. Ophthalmology 1986;93:74–87.
Cheung CY, Biousse V, Keane PA, Schiffrin EL, Wong TY. Hypertensive eye disease. Nat Rev Dis Prim. 2022;8:14.
Shah BM, Sadaka A, Berry S, Malik A, Lee AG. Bilateral disc edema in hypertensive emergency. Can J Ophthalmol 2018;53:e113–5.
Abbasi HN, Brady AJ, Cooper SA. Fulminant idiopathic intracranial hypertension with malignant systemic hypertension-a case report. Neuro-Ophthalmol. 2013;37:120–3.
de Carlo TE, Zahid S, MacIntosh PW. Optic nerve head edema in a healthy man in his 20s. JAMA Ophthalmol. 2019;137:455–6.
Lip PL, Burdon MA, Clarke CE, Beevers DG, Lip GYH. Lone papilloedema. Lancet. 2001;357:1924.
Sinclair AJ, Burdon MA, Nightingale PG, Matthews TD, Jacks A, Lawden M, et al. Rating papilloedema: an evaluation of the Frisen classification in idiopathic intracranial hypertension. J Neurol. 2012;259:1406–12.
Wall M, George D. Idiopathic intracranial hypertension. Brain 1991;114:155–80.
Ahn SJ, Woo SJ, Park KH. Retinal and choroidal changes with severe hypertension and their association with visual outcome. Investigative Ophthalmol Vis Neurosci. 2014;55:7775–85.
Thambisetty M, Lavin PJ, Newman NJ, Biousse V. Fulminant idiopathic intracranial hypertension. Neurology 2007;68:229–32.
Fodstad H, Kelly PJ, Buchfelder M. History of the cushing reflex. Neurosurgery. 2006;59:1132–7.
Taylor RD, Corcoran AC, Page IH. Increased cerebrospinal fluid pressure and papilledema in malignant hypertension. AMA Arch Intern Med. 1954;93:818–24.
Pickering GW. The cerebrospinal fluid pressure in arterial hypertension. Clin Sci. 1934;1:397–413.
Shelburne SA, Blain D, O’Hare JP. The spinal fluid in hypertension. J Clin Investig. 1932;11:489–96.
Lee AG, Beaver HA. Acute bilateral optic disk edema with a macular star figure in a 12-year-old girl. Surv Ophthalmol. 2002;47:42–9.
Author information
Authors and Affiliations
Contributions
MSL was responsible for designing the protocol, analysing data, interpreting results, and writing the draft of the manuscript. VS was responsible for designing the protocol, analysing data, interpreting results, and writing the draft of the manuscript. JJC, SG, MTB, AF, CMC, SK, VB, LS, and MD were responsible for collecting data, analysing data, interpreting results, and editing the manuscript.
Corresponding author
Ethics declarations
Competing interests
None of the authors have any disclosures relevant to this submission. Michael S Lee, MD receives royalties from Uptodate and Springer, receives research support from Invex, owns stock in Horizon, and serves as a consultant for Panbela. John Chen, MD, PhD serves as a consultant to Roche, UCB, and Horizon. Sidney Gospe MD has received support from the NIH. M. Tariq Bhatti, MD has served as a consultant for Bristol Meyers Squbb and Sanofi Genzyme. Valerie Biousse has served as a consultant for Gensight and Neurophoenix. Leanne Stunkel MD has no disclosures. Michael Dattilo, MD, PhD has no disclosures. Alexis Flowers, MD has no disclosures. Collin McClelland, MD has no disclosures. Victoria Sattarova, MD has no disclosures. Sachin Kedar, MD has not disclosures.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sattarova, V., Flowers, A., Gospe, S.M. et al. A multi-centre case series of patients with coexistent intracranial hypertension and malignant arterial hypertension. Eye 38, 274–278 (2024). https://doi.org/10.1038/s41433-023-02672-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02672-z