Abstract
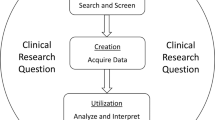
In the current literature, clinical registry cohorts related to ocular inflammation are few and far between, and there are none involving multi-continental international data. Many existing registries comprise administrative databases, data related to specific uveitic diseases, or are designed to address a particular clinical problem. The existing data, although useful and serving their intended purposes, are segmented and may not be sufficiently robust to design prognostication tools or draw epidemiological conclusions in the field of uveitis and ocular inflammation. To solve this, we have developed the Ocular Autoimmune Systemic Inflammatory Infectious Study (OASIS) Clinical Registry. OASIS collects prospective and retrospective data on patients with all types of ocular inflammatory conditions from centers all around the world. It is a primarily web-based platform with alternative offline modes of access. A comprehensive set of clinical data ranging from demographics, past medical history, clinical presentation, working diagnosis to visual outcomes are collected over a range of time points. Additionally, clinical images such as optical coherence tomography, fundus fluorescein angiography and indocyanine green angiography studies may be uploaded. Through the capturing of diverse, well-structured, and clinically meaningful data in a simplified and consistent fashion, OASIS will deliver a comprehensive and well organized data set ripe for data analysis. The applications of the registry are numerous, and include performing epidemiological analysis, monitoring drug side effects, and studying treatment safety efficacy. Furthermore, the data compiled in OASIS will be used to develop new classification and diagnostic systems, as well as treatment and prognostication guidelines for uveitis.
摘要
现有文献中, 与眼部炎症相关的临床注册队列很少, 而且没有涉及多中心的国际数据。许多现有的数据库, 包括行政数据库、与特定葡萄球菌疾病有关的数据, 是为了解决特定的临床问题。现有数据库虽然有用且服务于其预期目的, 但数据是不连续的, 可能不足以设计预测工具或得出葡萄膜炎和眼部炎症领域的流行病学结论。为了解决这个问题, 我们开发了眼部自身免疫性全身炎症感染研究 (OASIS) 临床注册数据库。OASIS从世界各地的中心收集所有类型的眼部炎症患者的前瞻性和回顾性数据。它是主要基于Web的平台, 也具有备选的离线访问模式。OASIS在一系列时间点收集了一组全面的临床数据, 从人口统计学、既往病史、临床表现、工作诊断到视觉结局。此外, OASIS可以上传临床图像, 例如相干光断层扫描, 荧光素血管造影和吲哚菁绿血管造影研究。OASIS通过以简化和固定的方式捕获多样化、结构良好且具有临床意义的数据, 提供全面且整理完善的数据集, 适合数据的分析。该数据集的应用很多, 包括进行流行病学分析、监测药物的副作用和研究治疗的安全性。此外, OASIS汇编的数据将用于开发新的分类和诊断系统, 以及葡萄膜炎的治疗和预后指南。
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Kempen JH, Daniel E, Gangaputra S, Dreger K, Jabs DA, Kaçmaz RO, et al. Methods for identifying long-term adverse effects of treatment in patients with eye diseases: the Systemic Immunosuppressive Therapy for Eye Diseases (SITE) Cohort Study. Ophthalmic Epidemiol. 2008;15:47–55.
Multicenter Uveitis Steroid Treatment Trial Research Group, Kempen JH, Altaweel MM, Holbrook JT, Jabs DA, Sugar EA. The multicenter uveitis steroid treatment trial: rationale, design, and baseline characteristics. Am J Ophthalmol. 2010;149:550–561.e10.
Rathinam SR, Gonzales JA, Thundikandy R, Kanakath A, Murugan SB, Vedhanayaki R, et al. Effect of corticosteroid-sparing treatment with mycophenolate mofetil vs methotrexate on inflammation in patients with uveitis: a randomized clinical trial. JAMA. 2019;322:936–45.
Jaffe GJ, Dick AD, Brézin AP, Nguyen QD, Thorne JE, Kestelyn P, et al. Adalimumab in patients with active noninfectious uveitis. N. Engl J Med. 2016;375:932–43.
Nguyen QD, Merrill PT, Jaffe GJ, Dick AD, Kurup SK, Sheppard J, et al. Adalimumab for prevention of uveitic flare in patients with inactive non-infectious uveitis controlled by corticosteroids (VISUAL II): a multicentre, double-masked, randomised, placebo-controlled phase 3 trial. Lancet. 2016;388:1183–92.
Ramanan AV, Dick AD, Jones AP, McKay A, Williamson PR, Compeyrot-Lacassagne S, et al. Adalimumab plus Methotrexate for Uveitis in Juvenile Idiopathic Arthritis. N. Engl J Med. 2017;376:1637–46.
Detels R, Muñoz A, McFarlane G, Kingsley LA, Margolick JB, Giorgi J, et al. Effectiveness of potent antiretroviral therapy on time to AIDS and death in men with known HIV infection duration. JAMA. 1998;280:1497–503.
Thio CL, Seaberg EC, Skolasky R Jr, Phair J, Visscher B, Muñoz A, et al. HIV-1, hepatitis B virus, and risk of liver-related mortality in the Multicenter Cohort Study (MACS). Lancet. 2002;360:1921–6.
Tan JCK, Ferdi AC, Gillies MC, Watson SL. Clinical registries in ophthalmology. Ophthalmology. 2019;126:655–62.
Li JQ, Heinz C, Dell J, Schmid M, Finger RP. Treatment exit options for non-infectious uveitis (TOFU): study protocol for a prospective clinical registry. Ophthalmic Epidemiol. 2021;21:1–8.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for acute posterior multifocal placoid pigment epitheliopathy. Am J Ophthalmol. 2021;228:174–81.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for acute retinal necrosis syndrome. Am J Ophthalmol. 2021;228:237–44.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for birdshot chorioretinitis. Am J Ophthalmol. 2021;228:65–71.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for behçet disease uveitis. Am J Ophthalmol. 2021;228:80–8.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for cytomegalovirus anterior uveitis. Am J Ophthalmol. 2021;228:89–95.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for cytomegalovirus retinitis. Am J Ophthalmol. 2021;228:245–54.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for fuchs uveitis syndrome. Am J Ophthalmol. 2021;228:262–7.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for herpes simplex virus anterior uveitis. Am J Ophthalmol. 2021;228:231–6.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for intermediate uveitis, non-pars planitis type. Am J Ophthalmol. 2021;228:159–64.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for juvenile idiopathic arthritis–associated chronic anterior uveitis. Am J Ophthalmol. 2021;228:192–7.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for multifocal choroiditis with panuveitis. Am J Ophthalmol. 2021;228:152–8.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for multiple evanescent white dot syndrome. Am J Ophthalmol. 2021;228:198–204.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for multiple sclerosis-associated intermediate uveitis. Am J Ophthalmol. 2021;228:72–9.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for pars planitis. Am J Ophthalmol. 2021;228:268–74.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for punctate inner choroiditis. Am J Ophthalmol. 2021;228:275–80.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for sarcoidosis-associated uveitis. Am J Ophthalmol. 2021;228:220–30.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for serpiginous choroiditis. Am J Ophthalmol. 2021;228:126–33.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for spondyloarthritis/HLA-B27-associated anterior uveitis. Am J Ophthalmol. 2021;228:117–25.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for sympathetic ophthalmia. Am J Ophthalmol. 2021;228:212–9.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for syphilitic uveitis. Am J Ophthalmol. 2021;228:182–91. Aug
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for toxoplasmic retinitis. Am J Ophthalmol. 2021;228:134–41.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for tubercular uveitis. Am J Ophthalmol. 2021;228:142–51.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for tubulointerstitial nephritis with uveitis syndrome. Am J Ophthalmol. 2021;228:255–61.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for varicella zoster virus anterior uveitis. Am J Ophthalmol. 2021;228:165–73.
Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for vogt-koyanagi-harada disease. Am J Ophthalmol. 2021;228:205–11.
Murray P. The standardization of Uveitis Nomenclature (SUN) working group. Standardization of uveitis nomenclature for reporting clinical data. Results of the first international workshop. Am J Ophthalmol. 2005;3:509–16.
Agrawal R, Testi I, Mahajan S, Yuen YS, Agarwal A, Kon OM, et al. Collaborative Ocular Tuberculosis Study consensus guidelines on the management of tubercular uveitis-report 1: guidelines for initiating antitubercular therapy in tubercular choroiditis. Ophthalmology. 2021;128:266–76.
Krizhevsky A, Sutskever I, Hinton GE. ImageNet classification with deep convolutional neural networks. Commun ACM. 2017;60:84–90.
Iandola FN, Han S, Moskewicz MW, Ashraf K, Dally WJ, Keutzer K SqueezeNet: AlexNet-level accuracy with 50x fewer parameters and <0.5MB model size [Internet]. arXiv [cs.CV]. 2016. Available from: http://arxiv.org/abs/1602.07360
Simonyan K, Zisserman A. Very Deep Convolutional Networks for Large-Scale Image Recognition [Internet]. arXiv [cs.CV]. 2014. Available from: http://arxiv.org/abs/1409.1556
Szegedy C, Liu W, Jia Y, Sermanet P, Reed S, Anguelov D, et al. Going deeper with convolutions. In: 2015 IEEE Conference on Computer Vision and Pattern Recognition (CVPR). 2015. p. 1–9.
He K, Zhang X, Ren S, Sun J. Deep Residual Learning for Image Recognition [Internet]. arXiv [cs.CV]. 2015. Available from: http://arxiv.org/abs/1512.03385
Huang G, Liu Z, van der Maaten L, Weinberger KQ. Densely Connected Convolutional Networks [Internet]. arXiv [cs.CV]. 2016. Available from: http://arxiv.org/abs/1608.06993
Chollet F Xception: Deep Learning with Depthwise Separable Convolutions. In: 2017 IEEE Conference on Computer Vision and Pattern Recognition (CVPR). 2017. p. 1800–7.
Ren S, He K, Girshick R, Sun J. Faster R-CNN: Towards real-time object detection with region proposal networks. IEEE Trans Pattern Anal Mach Intell. 2017;39:1137–49.
Hyvärinen A, Oja E. Independent component analysis: algorithms and applications. Neural Netw. 2000;13:411–30.
Tenenbaum JB, de Silva V, Langford JC. A global geometric framework for nonlinear dimensionality reduction. Science. 2000;290:2319–23.
Zimmer VA, Lekadir K, Hoogendoorn C, Frangi AF, Piella G. A framework for optimal kernel-based manifold embedding of medical image data. Comput Med Imaging Graph. 2015;41:93–107.
Zheng H-T, Borchert C, Jiang Y. A knowledge-driven approach to biomedical document conceptualization. Artif Intell Med. 2010;49:67–78.
Rosipal R, Krämer N. Overview and recent advances in partial least squares. In: Subspace, Latent Structure and Feature Selection. Springer Berlin Heidelberg; 2006. p. 34–51.
Jolliffe IT, Cadima J. Principal component analysis: a review and recent developments. Philos Trans A Math Phys Eng Sci. 2016;374:20150202.
Gola D, Mahachie John JM, van Steen K, König IR. A roadmap to multifactor dimensionality reduction methods. Brief Bioinform. 2016;17:293–308.
Pratihar DK. Non-Linear Dimensionality Reduction Techniques [Internet]. Encyclopedia of Data Warehousing and Mining, Second Edition. 2009. p. 1416–24. Available from: https://doi.org/10.4018/978-1-60566-010-3.ch219
Han L, Wu Z, Zeng K, Yang X. Online multilinear principal component analysis. Neurocomputing. 2018;275:888–96.
Lu H, Plataniotis KN, Venetsanopoulos AN. A survey of multilinear subspace learning for tensor data. Pattern Recognit. 2011;44:1540–51.
Learning the Kernel Matrix with Semi-definite Programming. Computer Science Division, University of California; 2002. 84.
Bank D, Koenigstein N, Giryes R. Autoencoders [Internet]. arXiv [cs.LG]. 2020. Available from: http://arxiv.org/abs/2003.05991
The 1000 Genomes Project Consortium, Auton A, Abecasis GR, Altshuler DM, Durbin RM, Abecasis GR, et al. A global reference for human genetic variation. Nature. 2015;526:68–74.
ENCODE Project Consortium. The ENCODE (ENCyclopedia Of DNA elements) project. Science. 2004;306:636–40.
Tomczak K, Czerwińska P, Wiznerowicz M. The Cancer Genome Atlas (TCGA): an immeasurable source of knowledge. Contemp Oncol (Pozn). 2015;19:A68–77.
Chen EJ, Bin Ismail MA, Mi H, Ho SL, Lim WK, Teoh SC, et al. Ocular autoimmune systemic inflammatory infectious study (OASIS) - report 1: epidemiology and classification. Ocul Immunol Inflamm. 2018;26:732–46.
M A, El-Asrar A, Abouammoh M, Al-Mezaine HS. Tuberculous uveitis. Middle East Afr J Ophthalmol. 2009;16:188–201.
Rao NA, Rajendram R, See RF Vogt-Koyanagi-Harada Disease. In: Retinal Imaging. Elsevier; 2006. p. 343–8.
Sazzini M, Garagnani P, Sarno S, De Fanti S, Lazzano T, Yang Yao D, et al. Tracing Behçet’s disease origins along the Silk Road: an anthropological evolutionary genetics perspective. Clin Exp Rheumatol. 2015;33:S60–6.
Jabs DA, Nussenblatt RB, Rosenbaum JT, Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–16.
Standardization of Uveitis Nomenclature (SUN) Working Group. Development of classification criteria for the uveitides. Am J Ophthalmol. 2021;228:96–105.
Ting DSW, Cheung CY-L, Lim G, Tan GSW, Quang ND, Gan A, et al. Development and validation of a deep learning system for diabetic retinopathy and related eye diseases using retinal images from multiethnic populations with diabetes. JAMA. 2017;318:2211–23.
Low R, Chen EJ, Bin Ismail MA, Mi H, Ling HS, Lim WK, et al. Ocular autoimmune systemic inflammatory infectious study (OASIS) - report 2: pattern of uveitis investigations in Singapore. Ocul Immunol Inflamm. 2020;28:92–9.
Agrawal R, Testi I, Bodaghi B, Barisani-Asenbauer T, McCluskey P, Agarwal A, et al. Collaborative ocular tuberculosis study consensus guidelines on the management of tubercular uveitis-report 2: guidelines for initiating antitubercular therapy in anterior uveitis, intermediate uveitis, panuveitis, and retinal vasculitis. Ophthalmology. 2021;128:277–87.
Kamath PS, Kim WR, Advanced Liver Disease Study Group. The model for end-stage liver disease (MELD). Hepatology. 2007;45:797–805.
Casey BM, McIntire DD, Leveno KJ. The continuing value of the Apgar score for the assessment of newborn infants. N. Engl J Med. 2001;344:467–71.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002;15:163–5.
Cecchin V, Zannin ME, Ferrari D, Pontikaki I, Miserocchi E, Paroli MP, et al. Longterm safety and efficacy of adalimumab and infliximab for uveitis associated with juvenile idiopathic arthritis. J Rheumatol. 2018;45:1167–72.
Funding
RA received funding from National Medical Research Council, Ministry of Health, Singapore for his project entitled “To establish a predictive artificial intelligence (AI) based model using immune-phenotype correlation for disease stratification and prognosis in patients with ocular tuberculosis (OTB)”, Grant: MOH/NMRC/CSAINV/19nov-007.
Author information
Authors and Affiliations
Consortia
Contributions
The authors confirm their contribution to the paper as follows: study conception and design: RA, VG, JHK; data collection: all authors; analysis and interpretation of results: RA, BL, SMSN, RL, JHK; draft manuscript preparation: all authors. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ng, S.M.S., Low, R., Pak, C. et al. The role of a multicentre data repository in ocular inflammation: The Ocular Autoimmune Systemic Inflammatory Infectious Study (OASIS). Eye 37, 3084–3096 (2023). https://doi.org/10.1038/s41433-023-02472-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02472-5
This article is cited by
-
Knowledge and Current Practices in Monogenic Uveitis: An International Survey by IUSG and AIDA Network
Ophthalmology and Therapy (2024)