Abstract
Objectives
To evaluate the effect of miosis and laser peripheral iridotomy (LPI) on intraocular lens (IOL) power prediction and ocular biometry in eyes with primary angle closure disease (PACD).
Methods
In this prospective observational study, primary angle closure suspects (PACS), and subjects classified with primary angle closure (PAC)/primary angle-closure glaucoma (PACG) undergoing LPI were enrolled. Ocular biometric parameters were measured with IOLMaster700 at baseline (T0), one week after pilocarpine instillation (T1), and another week post LPI (T2). Biometric changes and the IOL power predicted for emmetropia using Barrett Universal II, Haigis, Holladay2, Hoffer Q and SRK/T formulae were analysed and compared among different time points.
Results
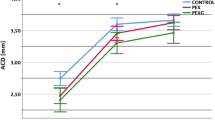
100 eyes of 50 PACS and 50 PAC/PACG patients were enrolled. Following pilocarpine-induced miosis, lens thickness (LT) increased and anterior chamber depth (ACD) decreased (all groups p < 0.01), while white-to-white diameter decreased and central corneal thickness increased significantly only in the PACS cohort (both p < 0.01). Compared to baseline, LPI induced an increase of ACD and a slight decrease of LT in PACS (both p < 0.01), whereas only axial length changed significantly (p = 0.012) in the PAC/PACG cohort. Regardless of the formula used, no significant difference to the predicted IOL power for emmetropia existed among the three time points in each group (all p > 0.1).
Conclusion
We report the changes of anterior segment parameters induced by miosis and LPI in PACD. These interventions do not significantly affect the IOL power calculation predicted for emmetropia in Chinese eyes when common third-, fourth-and new generation IOL formulae are used.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated and analysed during the current study are available from the corresponding author, YHC, on reasonable request. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
References
Prum BE Jr, Herndon LW Jr, Moroi SE, Mansberger SL, Stein JD, Lim MC, et al. Primary angle closure preferred practice pattern((R)) guidelines. Ophthalmology. 2016;123:40.
Lee HS, Park JW, Park SW. Factors affecting refractive outcome after cataract surgery in patients with a history of acute primary angle closure. Jpn J Ophthalmol. 2014;58:33–9.
Manoharan N, Patnaik JL, Bonnell LN, SooHoo JR, Pantcheva MB, Kahook MY, et al. Refractive outcomes of phacoemulsification cataract surgery in glaucoma patients. J Cataract Refract Surg. 2018;44:348–54.
Croft MA, McDonald JP, Katz A, Lin TL, Lütjen-Drecoll E, Kaufman PL. Extralenticular and lenticular aspects of accommodation and presbyopia in human versus monkey eyes. Invest Ophthalmol Vis Sci. 2013;54:5035–48.
Langenbucher A, Haigis W, Seitz B. Difficult lens power calculations. Curr Opin Ophthalmol. 2004;15:1–9.
Chen X, Wang X, Tang Y, Sun X, Chen Y. Optical coherence tomography analysis of anterior segment parameters before and after laser peripheral iridotomy in primary angle-closure suspects by using CASIA2. BMC Ophthalmol. 2022;22:144.
Talajic JC, Lesk MR, Nantel-Battista M, Harasymowycz PJ. Anterior segment changes after pilocarpine and laser iridotomy for primary angle-closure suspects with Scheimpflug photography. J Glaucoma. 2013;22:776–9.
Mogil RS, Khezri N, Ren R, Adleyba O, Abumasmah R, Ghassibi MP, et al. Changes in iridocorneal angle and anterior chamber structure in eyes with anatomically narrow angles: laser iridotomy versus pilocarpine. J Glaucoma. 2018;27:1073–8.
Muzyka-Woźniak M, Ogar A. Anterior chamber depth and iris and lens position before and after phacoemulsification in eyes with a short or long axial length. J Cataract Refract Surg. 2016;42:563–8.
Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86:238–42.
European Glaucoma Society Terminology and Guidelines for Glaucoma. 5th edn. Br J Ophthalmol. 2021;105(Suppl 1):1–169.
Gupta R, Kumar R, Chauhan L. Anterior chamber morphology changes in eyes with narrow angles by Scheimpflug imaging: Pilocarpine versus laser peripheral iridotomy. Int Ophthalmol. 2021;41:2099–108.
Saitoh K, Yoshida K, Hamatsu Y, Tazawa Y. Changes in the shape of the anterior and posterior corneal surfaces caused by mydriasis and miosis: detailed analysis. J Cataract Refract Surg. 2004;30:1024–30.
Kashiwagi K, Abe K, Tsukahara S. Quantitative evaluation of changes in anterior segment biometry by peripheral laser iridotomy using newly developed scanning peripheral anterior chamber depth analyser. Br J Ophthalmol. 2004;88:1036–41.
He M, Friedman DS, Ge J, Huang W, Jin C, Lee PS, et al. Laser peripheral iridotomy in primary angle-closure suspects: biometric and gonioscopic outcomes: the Liwan Eye Study. Ophthalmology. 2007;114:494–500.
Liu YM, Hu D, Zhou LF, Lan J, Feng CC, Wang XY, et al. Associations of lens thickness and axial length with outcomes of laser peripheral iridotomy. Int J Ophthalmol. 2021;14:714–8.
Shrivastava AK, Behera P, Kumar B, Nanda S. Precision of intraocular lens power prediction in eyes shorter than 22 mm: an analysis of 6 formulas. J Cataract Refract Surg. 2018;44:1317–20.
Gokce SE, Montes De Oca I, Cooke DL, Wang L, Koch DD, Al-Mohtaseb Z. Accuracy of 8 intraocular lens calculation formulas in relation to anterior chamber depth in patients with normal axial lengths. J Cataract Refract Surg. 2018;44:362–8.
Lane S, Collins S, Das KK, Maass S, Thatthamla I, Schatz H, et al. Evaluation of intraocular lens mechanical stability. J Cataract Refract Surg. 2019;45:501–6.
Mencucci R, Cennamo M, Venturi D, Vignapiano R, Favuzza E. Visual outcome, optical quality, and patient satisfaction with a new monofocal IOL, enhanced for intermediate vision: preliminary results. J Cataract Refract Surg. 2020;46:378–87.
Auffarth GU, Gerl M, Tsai L, Janakiraman DP, Jackson B, Alarcon A, et al. Clinical evaluation of a new monofocal IOL with enhanced intermediate function in patients with cataract. J Cataract Refract Surg. 2021;47:184–91.
Olsen T. Calculation of intraocular lens power: a review. Acta Ophthalmol Scand. 2007;85:472–85.
Read SA, Collins MJ, Iskander DR. Diurnal variation of axial length, intraocular pressure, and anterior eye biometrics. Invest Ophthalmol Vis Sci. 2008;49:2911–8.
Yamagishi-Kimura R, Honjo M, Komizo T, Ono T, Yagi A, Lee J, et al. Interaction between pilocarpine and ripasudil on intraocular pressure, pupil diameter, and the aqueous-outflow pathway. Invest Ophthalmol Vis Sci. 2018;59:1844–54.
Hirasawa K, Shoji N, Kobashi C, Yamanashi A. Effects of mydriasis and miosis on kinetic perimetry findings in normal participants. Graefes Arch Clin Exp Ophthalmol. 2015;253:1341–6.
Yunard A, Oktariana VD, Artini W, Prihartono J. Comparison of intraocular pressure and anterior chamber angle changes between pilocarpine and laser peripheral iridotomy. J Curr Glaucoma Pract. 2019;13:32–6.
Niemczyk M, Danielewska ME, Kostyszak MA, Lewandowski D, Iskander DR. The effect of intraocular pressure elevation and related ocular biometry changes on corneal OCT speckle distribution in porcine eyes. PLoS One. 2021;16:e0249213.
Tekcan H, Mangan MS, Imamoglu S, Alpogan O. Refractive outcomes of uneventful cataract surgery in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Korean J Ophthalmol. 2022;36:226–35.
Altan C, Bayraktar S, Altan T, Eren H, Yilmaz OF. Anterior chamber depth, iridocorneal angle width, and intraocular pressure changes after uneventful phacoemulsification in eyes without glaucoma and with open iridocorneal angles. J Cataract Refract Surg. 2004;30:832–8.
Radhakrishnan S, Chen PP, Junk AK, Nouri-Mahdavi K, Chen TC. Laser peripheral iridotomy in primary angle closure: a report by the American Academy of Ophthalmology. Ophthalmology. 2018;125:1110–20.
Guzman CP, Gong T, Nongpiur ME, Perera SA, How AC, Lee HK, et al. Anterior segment optical coherence tomography parameters in subtypes of primary angle closure. Invest Ophthalmol Vis Sci. 2013;54:5281–6.
Funding
This research project was supported directly by Shanghai Municipal Health Commission (20214Y0073), Clinical Research Plan of SHDC (Grant No. SHDC2020CR6029). The authors were also supported by grants from the State Program of National Natural Science Foundation of China (81870692), Shanghai Committee of Science and Technology (Grant no. 20S31905800), National Key Research and Development Program of China (2020YFA0112700), the State Key Program of National Natural Science Foundation of China (82030027), the subject of major projects of National Natural Science Foundation of China (81790641), and National Natural Science Foundation of China (82101123).
Author information
Authors and Affiliations
Contributions
XS and YC conceived and designed the work. HY and DQ majorly carried out this clinic trial and acquired data. JW, GC and HY played an important role in data analysis and results interpretation. HY, GC and YC drafted and revised the manuscript. All the authors approved the final version to be published.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, H., Qian, D., Chan, G. et al. Influence of miosis and laser peripheral iridotomy on intraocular lens power calculation in patients with primary angle closure disease. Eye 37, 2744–2752 (2023). https://doi.org/10.1038/s41433-023-02408-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02408-z