Abstract
Purpose
To compare the efficacy of macular buckling (MB) alone against a combined internal limiting membrane (ILM) inversion flap for full-thickness macular hole (FTMH)-associated macular detachment (MD) in patients with high myopia.
Methods
This was a prospective interventional case series of patients with high myopia surgically treated with MB alone or combined with an inverted ILM flap for FTMH- associated MD. Best-corrected visual acuity (BCVA) at the 24-month postoperative follow-up, rate of initial retinal reattachment and macular hole closure were measured.
Results
A total of 62 eyes from 62 participants (33 in the MB group, 29 in the combination group) were studied. Postoperative BCVA improved significantly in both the combination group (P < 0.001) and the MB group (P = 0.027). The postoperative BCVA at 12 months (P = 0.021) and 24 months (P = 0.041) was significantly better in the combination group than in the MB group. The postoperative BCVA was not significantly different between the eyes with closed and unclosed MH at each follow-up time point (P > 0.05). In the combination group, we observed earlier retinal reattachment and closure of the MH as well as a higher rate of MH closure (82.8% vs. 66.7%) than in the MB group, although this difference was insignificant (P = 0.248).
Conclusion
MB combined with the ILM flap inversion technique achieved better postoperative BCVA and a higher success rate of MH closure than MB alone. We believe that combination surgery should be preferentially recommended.
Similar content being viewed by others
Introduction
Macular detachment (MD) associated with a full-thickness macular hole (FTMH) is a severe vision-threatening complication of high myopia [1]. High myopia patients with FTMH require urgent surgical intervention because they can easily develop to retinal and choroidal detachment. Several surgical methods have been attempted to treat high myopia patients with FTMH, including pars plana vitrectomy (PPV) with internal limiting membrane (ILM) peeling [2] or ILM flap inversion [3,4,5,6,7], lens capsular flap transplantation [8], autologous serum injection [9], autologous neurosensory retinal flap transplantation [10], human amniotic membrane grafting [11], and gas or silicone oil tamponade. Previous studies demonstrated that the inverted ILM flap technique can provide a bridge that helps the edges of the macular hole to migrate centripetally, thus achieving a better functional and anatomical prognosis, especially in large macular holes (MHs) [12], in high myopia MHs, and in refractory MHs [13, 14]. However, the MH is often accompanied by posterior staphyloma and expanded eyeball in eyes with high myopia, PPV alone often caused more severe macular atrophy progression after surgery than MB [11, 15], and primary anatomical success was significantly lower when compared to emmetropic patients [16].
Macular buckling (MB) has shown success in the treatment of MH-associated MD in patients with high myopia, as MB corrects posterior staphyloma, thus releasing anteroposterior traction forces and aiding reattachment [17, 18]. Our previous study showed that the retinal reattachment success rate was significantly higher with MB than with PPV, although there was no significant difference in the MH closure rate [15]. Due to the complexity of the macular hole in high myopia, combined surgery is recommended.
Thus, our study aims to evaluate and compare the long-term effects of MB alone to combined ILM flap inversion for high myopia patients with MH-associated MD. Our results can provide evidence to improve surgical design and obtain more satisfactory results in the surgical management of high myopia patients with MH-associated MD.
Methods
Trial design
This prospective study was designed to explore the prognosis of high myopia patients with full-thickness macular hole (FTMH)-associated macular detachment (MD) undergoing the macular buckling (MB) surgery alone (the MB group) or combined with an internal limiting membrane (ILM) inversion flap (the combination group). High myopia patients with FTMH-associated MD due to axial length elongation were recruited between January 2017 and November 2019 at Zhongshan Ophthalmic Center in Guangzhou, China. Randomized grouping was conducted after participants were informed about the purpose of this study and informed consent was signed. This study was approved by the Ethical Review Committee of Zhongshan Ophthalmic Center and adhered to the tenets of the Declaration of Helsinki.
It was assumed that MH closure rate would be 64% after receiving MB and 90% after receiving combined surgery, with 80% statistical power and a two-sided test. Thus, to allow for a 3% loss during follow-up, a total of 70 participants were required to participate in this study, with 35 patients in each arm (calculated using G-Power V.3.1.9.2 software).
Inclusion and exclusion criteria
High myopia patients between the age of 18 and 70 years old, with an axial length (AL) longer than 26.5 mm or a refractive error (spherical equivalent) less than −8.0 dioptres, and presence of FTMH-associated MD on optical coherence tomography (OCT) were included. Our exclusion criteria were patients with a history of ocular trauma or glaucoma, an active intraocular haemorrhage or inflammation, any media opacity that precluded imaging or clinical evaluation of the macula, a history of intraocular surgery except cataract surgery, and retinal detachment extending beyond the vascular arcades.
Participants
A total of 80 high myopia patients with FTMH-associated MD on OCT images were initially recruited, of which 7 patients were excluded according to the exclusion criteria that had extended retinal detachment beyond the vascular arcades while awaiting surgery, 3 patients declined participation. A total of 70 patients were finally included, with randomized grouping of 35 eyes in the MB group and 35 eyes in the combination group (Fig. 1).
Randomization
The 70 participants included were randomized according to a 1:1 ratio using a random number generator and assigned to undergo either MB alone surgery or MB combined with ILM flap inversion. The patients were given a detailed explanation of their assigned surgical procedures and understood the risks of potential complications before giving consent.
Surgical technique
One experienced vitreoretinal surgeon (LL) performed all the surgeries under retrobulbar or general anaesthesia. The MB surgery was performed using a silicone sponge-titanium exoplant, as described in our previous studies [15, 19]. Under general or retrobulbar anaesthesia, the surgery began with a 360o limbal periotomy. The superior rectus, lateral rectus, inferior rectus and the inferior oblique muscle were separated from the surrounding tendons. The rectus muscles were then looped using silk ties to allow for rotation of eye position. One of the distal ends of the silicone band was passed under the inferior oblique muscle, lateral rectus and inferior rectus, then it was sutured to the sclera on the nasal side of the inferior rectus muscle using a spatulated needle with 5-0 non-absorbable thread (Ethicon, Johnson & Johnson Medical Ltd, China) approximately 12 mm posterior to the limbus. The other end of the band crossed the superior rectus muscle, and it was sutured to the sclera on the nasal side of the superior rectus muscle. Release part of the aqueous humour by anterior chamber puncture. The sponge-enveloped titanium plate was sutured in the superior temporal quadrant. The length of the upper and lower bands and the location of the temporal titanium plate sutures were calculated from preoperative 3D MRI of patients. Intraoperative adjustments were made under indirect fundoscopy to ensure that the surgical ridge was located in the centre of the macula.
The participants in the combined group underwent MB, followed by 25-gauge PPV. A 25-gauge PPV was performed according to a regular procedure. The core and posterior hyaloid were removed, followed by a first air-fluid exchange drained subretinal fluid (SRF), which temporarily reattached the retina. Indocyanine green was used to stain the ILM, which was then peeled using microforceps. The ILM flap was gently inverted to cover the MH, and perfluorocarbon liquid (PFCL) was injected to stabilize the ILM flap. Air-fluid exchange and air-PFCL exchange were then conducted, eventually filling the vitreous cavity with filtered air. At the end of the surgery, viscoelastic agents were dropped upon the ILM flap to avoid flap displacement. Patients were instructed to maintain a prone position for 3 days after surgery.
Outcome measurements
All participants returned for follow-up at 6 months, 12 months and 24 months postsurgery for evaluation. The outcome parameters assessed were best corrected visual acuity (BCVA), intraocular pressure (IOP) measurements (TX-200 tonometer; Canon, Japan), AL measurements (IOL Master; Carl Zeiss, Germany), OCT (Heidelberg Engineering, Heidelberg, Germany; DRI-OCT, Topcon Corp, Tokyo, Japan), retinal reattachment, MH closure and complications. The absence of a foveal defect and absence of bare RPE exposure to the vitreous were regarded as MH closure. The technician who performed the examination was blind to the patients’ group.
Statistical analysis
Data processing and analysis were performed with SPSS software for Windows (V23.0). Data are presented as the mean ± SD. For variables with a normal distribution, 2 independent t tests were used for comparison. For variables with a nonnormal distribution, Mann-Whitney U tests were performed for analysis. Chi-square tests were used to assess qualitative data. One-way analysis of variance was conducted to analyse presurgery and postsurgery BCVA and AL. The results were considered statistically significant when the P value was less than 0.05.
Results
A randomized grouping of 70 eyes from 70 participants included had 35 participants in the MB surgery group and 35 participants in the combined surgery group. One participant in the MB group and two participants in the combination group did not receive their allocated intervention. Due to incomplete postsurgical follow-up, 1 participant in the MB group and 4 participants in the combined group were excluded from the final analysis. Patient demographics and ocular characteristics between the two groups were well matched (Table 1).
Comparison of BCVA between the two groups
After surgery, there was significant improvement in BCVA for both groups (P < 0.05). The BCVA was significantly better in the combination group at 12 months (P = 0.021) and 24 months (P = 0.041) than in the MB group, but not at 6 months (P = 0.132) (Table 1). For eyes with MH closure, there was significant improvement in BCVA in the combination group (P < 0.001); however, this improvement was not significant in the MB group (P = 0.058). For eyes without MH closure, there was no significant improvement in BCVA for either group (P > 0.05). Comparing eyes with and without MH closure, BCVA was not significantly different at every follow-up time point within both groups (P > 0.05) (Table 2).
Comparison of retinal reattachment and MH closure rates between the two groups
Retinal reattachment was achieved in 32 (32/33, 97.0%) eyes in the MB group and 29 (29/29 = 100%) eyes in the combination group at 24 months postoperatively. There was 1 eye in the MB group in which neither retinal reattachment nor MH closure was achieved during the follow-up period. MH closure was reached in 22 (22/33, 66.7%) eyes in the MB group and in 24 (24/29, 82.8%) eyes in the combination group at 24 months postoperatively.
A higher rate of retinal reattachment was found in the combination group at one month after surgery (P = 0.018), but no difference was found between the two groups at 3 months, 6 months, 12 months and 24 months after surgery. The rate of MH closure was higher in the combination group at one month (P < 0.001) and 3 months (P = 0.04), but the difference in rate was not significant at 6 months, 12 months, and 24 months postsurgery (Supplementary Table 1) (Fig. 2).
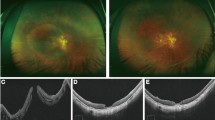
Ai Presurgical image of MH-associated macular detachment (MD) from a patient in the MB group. Aii Closed MH and residual subretinal fluid (SRF) outside the fovea 3 months after MB surgery. Aiii–iv Retinal reattachment with MH closure at 1 year and 2 years after MB. Bi A presurgical image of MH and MD of a patient from the combination group. Bii MH closure with MD at 1 month after combined surgery. Biii Image showing most of the SRF absorbed at 6 months after surgery. Biv Retinal reattachment with MH closure at 18 months after surgery. Ci Presurgical image of MH and macular detachment (MD) from a patient in the MB group. Cii–iv Images of retinal reattachment with remaining unclosed MHs at 1 month, 6 months and 2 years after surgery. Di A presurgical image of a patient in the combination group with MH and MD. Dii–iv Images of retinal reattachment without MH closure at the 3-month, 12-month and 24-month follow-ups after combined surgery.
In all the eyes of the combination group, ILM flap inversion was attempted. However, successful inversion was achieved in only 20 (20/29 = 69.0%) eyes. For these 20 eyes with successful ILM flap inversion, the MH closure rate was 100%. However, the MH failed to close in five of the nine eyes where ILM flap inversion was unsuccessful (Fig. 2).
Comparison of axial length between the two groups
There was no significant difference in AL between the two groups at any time point (P > 0.05). After surgery, AL was significantly shortened for both groups (P < 0.001). There was also a trend of gradual regression of AL in both groups up to 12 months postsurgery (Supplementary Table 2).
Complications after surgery
Diplopia and metamorphopsia were the most common postoperative complications (65/67, 97.01%) in the early postoperative period, and these symptoms tended to recover or decrease over time. Within the 24-month follow-up period, cataract surgery was performed for 5 patients in the MB group and 9 patients in the combination group. There were 2 eyes in the MB group that developed retinoschisis after retinal reattachment and MH closure with disappearance of the surgical ridge. Intraretinal cysts were observed in three cases from the MB group and in two cases from the combination group. Choroidal neovascularization (CNV) was observed in one eye from the MB group after surgery (Fig. 3).
Ai The image at 6 months after MB group shows the retinal reattachment with MH closure. Aii The image at postoperative year 1 shows the retinoschisis with an obvious decrease in the surgical ridge. Bi The image at 1 year after combination surgery shows retinal reattachment with MH closure. Bii Image of intraretinal cysts at 23 months after surgery. Ci The image at 1 month after MB surgery showing MH unclosure without CNV. Cii The image at 1 year after surgery showing MH closure with choroidal neovascularization.
Discussion
MH with retinal detachment in patients with high myopia has been difficult to manage and poses great challenges for vitreoretinal surgeons. This study compared the effect of MB and combined surgery with ILM flap inversion on FTMH- associated MD. All patients in the combined group were treated with MB, PPV, ILM flap inversion and filtered air as tamponade. Overall, the combined surgery achieved a higher and earlier MH closure, and BCVA improved for both groups, although MH closure did not account for a significant difference in postsurgical BCVA.
Several techniques have been proposed to treat high myopia MH. The autologous retinal transplantation technique to repair high myopia MH was studied by Moysidis et al. [20] and a high rate of hyperreflective foci was found in the graft early after surgery. On the other hand, Chen et al. [21] reported that excessive gliosis was observed with an inverted ILM flap. Gliosis is necessary for MH closure, a process during which neurotrophic factors and basic fibroblast growth factors are produced by activated Müller cells, and the ILM helps in cocultured Müller cell proliferation [22]. Eyes with high myopia have a much thinner ILM [23, 24], and as a response to the elongated globe in the eye with high myopia, Müller cells enter the ILM, causing Müller cell debris to accumulate, thus providing a damage-repairing microenvironment that promotes glial proliferation [23]. However, excessive gliosis can be toxic to neurons. The resulting irregular surface of the retina caused by excessive gliosis could lead to metamorphopsia.
In our study, the MH closure rate was 82.8% in the combination group and only 66.7% in the MB group. The BCVA was better in the combined group at 12 months and 24 months postoperatively than that in the MB group. However, the BCVA between closed MH and unclosed MH was not significantly different, which was in line with other studies. [13, 21, 25]
Previous studies have shown that ELM and EZ restoration was associated with improvement of postsurgical BCVA [26]. However, the outer retinal layer was difficult to identify in our study due to chorioretinal atrophy, indicating that irreversible damage had occurred in the photoreceptor layer. In a regular macular hole, closure was facilitated by concentric contraction of the outer plexiform layer and the centripetal displacement of photoreceptors [27]. Although the fovea was filled with glial tissue [28], atrophy of the photoreceptor layer caused irreversible damage such that the fovea lost its original stratified structure. Hence, it is explicable that the postsurgical BCVA between closed and unclosed MHs was not significantly different.
In the combined group, the recovery of retinal reattachment and MH closure was earlier than that in the MB group. There might be two recovery patterns for the different surgical methods. In the MB group, retinal reattachment occurred due to scleral imbrications that attached the eyeball to the retina, and MH closure was caused by the migration of activated glial cells over time. In combined surgery, the mechanism of MH closure was different, as the inverted ILM flap formed a bridge that provided a scaffold for cells to encroach and enclose the hole. Then, the subretinal fluid was absorbed gradually, and the retina was reattached. Even so, the combined surgery resulted in earlier retinal reattachment and MH closure than MB alone.
In our study, only 69% of patients with combined surgery underwent a successful ILM flap inversion procedure, while the other 31% were unable to complete this procedure because the surgeon could not peel a relatively complete ILM to cover the MH. Due to the unique anatomy of an eye with high myopia and considering its long axial length, thin neurosensory layers, thin ILM and poor contrast, performing procedures in eyes with high myopia are challenging even for an experienced surgeon. Meta-analysis [7] showed that the inverted ILM flap technique could reach a high MH closure ranging from 91.8% to 97.1% and could be an alternative to the treatment of MH in high myopia with or without retinal detachment. In our study, in cases of successful ILM reversal, all the macular holes were closed. Inversion of the ILM flap might have served as a bridge, thus providing scaffolding for tissue proliferation which aids in the healing process of MH. Even though there was no difference in BCVA after surgery between the MH closure and nonclosure groups, MH closure reduced the risk of retinal detachment later in life [29].
Choroidal neovascularization was found to have developed in one case. This might be due to intraoperative and postoperative inflammation that induced the expression of vascular endothelial growth factor. Another reason might be the compression force of the buckle implant disturbing the microcirculatory drainage of the choroid [30], leading to local ischaemia and hypoxia.
Intraretinal cysts were seen in five eyes, which has never been reported in the eyes treated by PPV alone. The presence of cysts was seen as cystoid changes without subretinal fluid. This was likely due to atrophy or loss of tissue. Poor RPE function due to extremely high myopia might be the cause of retinal degeneration and failure of retinal outflow mechanisms, explaining the presence of postsurgery intraretinal cysts.
Our study had an adequate follow-up period of 24 months after surgery, which was a strength of our investigation. However, there were some limitations. First, this was a single-site study, the sample size was relatively small and the loss to follow up was relatively high. Second, such manoeuvres may be technically challenging even for experienced surgeons, as only 69% of patients in the combined group had a successful ILM flap inversion due to an excessively long axis and thin ILM. Third, the mechanisms behind the lack of a significant difference in BCVA between closed and unclosed MHs as well as the development of postsurgical CNV and intraretinal cysts remain unclear, and further research is needed.
In conclusion, MB combined with ILM flap inversion achieved significant BCVA improvement and a higher MH closure rate in high myopia patients with FTMH- associated macular detachment. MH closure could prevent future retinal detachments. Therefore, it is a recommended method of surgical management for MH-associated MD in high myopia patients.
Summary table
What was known before
-
The macular hole closure rate was relatively low with macular buckling alone, whereas PPV alone often caused more severe macular atrophy progression after surgery which impair the postoperative BCVA.
What this study adds
-
MB combined with PPV and the ILM flap inversion technique achieved better postoperative BCVA and a higher success rate of MH closure than MB alone.
Data availability
The data was available from the corresponding author on the reasonable request.
References
Ruiz-Medrano J, Montero JA, Flores-Moreno I, Arias L, Garcia-Layana A, Ruiz-Moreno JM. Myopic maculopathy: Current status and proposal for a new classification and grading system (ATN). Prog Retin Eye Res. 2019;69:80–115.
Uemoto R, Yamamoto S, Tsukahara I, Takeuchi S. Efficacy of internal limiting membrane removal for retinal detachments resulting from a myopic macular hole. Retina. 2004;24:560–6.
Chen SN, Yang CM. Inverted internal limiting membrane insertion for macular hole-associated retinal detachment in high myopia. Am J Ophthalmol. 2016;162:99–106.e101.
Kuriyama S, Hayashi H, Jingami Y, Kuramoto N, Akita J, Matsumoto M. Efficacy of inverted internal limiting membrane flap technique for the treatment of macular hole in high myopia. Am J Ophthalmol. 2013;156:125–31.e121.
Michalewska Z, Michalewski J, Dulczewska-Cichecka K, Nawrocki J. Inverted internal limiting membrane flap technique for surgical repair of myopic macular holes. Retina. 2014;34:664–9.
Olenik A, Rios J, Mateo C. Inverted internal limiting membrane flap technique for macular holes in high myopia with axial length >/=30 mm. Retina. 2016;36:1688–93.
Chatziralli I, Machairoudia G, Kazantzis D, Theodossiadis G, Theodossiadis P. Inverted internal limiting membrane flap technique for myopic macular hole: A meta-analysis. Surv Ophthalmol. 2021;66:771–80.
Chen SN, Yang CM. Lens capsular flap transplantation in the management of refractory macular hole from multiple etiologies. Retina. 2016;36:163–70.
Ezra E, Gregor ZJ, Morfields Macular Hole Study Ggroup Report N. Surgery for idiopathic full-thickness macular hole: two-year results of a randomized clinical trial comparing natural history, vitrectomy, and vitrectomy plus autologous serum: Morfields Macular Hole Study Group RAeport no. 1. Arch Ophthalmol. 2004;122:224–36.
Takeuchi J, Kataoka K, Shimizu H, Tomita R, Kominami T, Ushida H, et al. Intraoperative and Postoperative Monitoring of Autologous Neurosensory Retinal Flap Transplantation for a Refractory Macular Hole Associated with High Myopia. Retina. 2021;41:921–30.
Tsai DC, Huang YH, Chen SJ. Parafoveal atrophy after human amniotic membrane graft for macular hole in patients with high myopia. Br J Ophthalmol. 2021;105:1002–10.
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018–25.
Gu X, Hu Z, Qian H, Fransisca S, Mugisha A, Wang J, et al. Perfluorocarbon liquid-assisted inverted internal limiting membrane flap technique versus internal limiting membrane peeling for highly myopic macular hole retinal detachment. Retina. 2021;41:317–23.
Hu Z, Gu X, Qian H, Liang K, Zhang W, Ji J, et al. Perfluorocarbon Liquid-Assisted Inverted Limiting Membrane Flap Technique Combined With Subretinal Fluid Drainage for Macular Hole Retinal Detachment in Highly Myopic Eyes. Retina. 2019.
Zhao X, Li Y, Ma W, Lian P, Yu X, Chen S, et al. Macular buckling versus vitrectomy on macular hole associated macular detachment in eyes with high myopia: a randomised trial. Br J Ophthalmol. 2021;0:1–5.
Ikuno Y. Overview of the Complications of High Myopia. Retina. 2017;37:2347–51.
Ripandelli G, Coppe AM, Fedeli R, Parisi V, D’Amico DJ, Stirpe M. Evaluation of primary surgical procedures for retinal detachment with macular hole in highly myopic eyes: a comparison [corrected] of vitrectomy versus posterior episcleral buckling surgery. Ophthalmology. 2001;108:2258–64.
Theodossiadis GP, Theodossiadis PG. The macular buckling procedure in the treatment of retinal detachment in highly myopic eyes with macular hole and posterior staphyloma: mean follow-up of 15 years. Retina. 2005;25:285–89.
Zhao X, Ma W, Lian P, Tanumiharjo S, Lin Y, Ding X, et al. Three-year outcomes of macular buckling for macular holes and foveoschisis in highly myopic eyes. Acta Ophthalmol. 2020;98:e470–e78.
Moysidis SN, Koulisis N, Adrean SD, Charles S, Chetty N, Chhablani JK, et al. Autologous Retinal Transplantation for Primary and Refractory Macular Holes and Macular Hole Retinal Detachments: The Global Consortium. Ophthalmology. 2021;128:672–85.
Chen Y, Wang J, Ye X, Yu J, Tao J, Lin L, et al. The Role of Internal Limiting Membrane Flap for Highly Myopic Macular Hole Retinal Detachment: Improving the Closure Rate but Leading to Excessive Gliosis. Front Med (Lausanne). 2021;8:812693.
Zhang L, Li X, Lin X, Wu M. Nerve growth factor promotes the proliferation of Muller cells co-cultured with internal limiting membrane by regulating cell cycle via Trk-A/PI3K/Akt pathway. BMC Ophthalmol. 2019;19:130.
Chen L, Wei Y, Zhou X, Zhang Z, Chi W, Gong L, et al. Morphologic, Biomechanical, and Compositional Features of the Internal Limiting Membrane in Pathologic Myopic Foveoschisis. Invest Ophthalmol Vis Sci. 2018;59:5569–78.
Vogt D, Stefanov S, Guenther SR, Hagenau F, Wolf A, Priglinger SG, et al. Comparison of Vitreomacular Interface Changes in Myopic Foveoschisis and Idiopathic Epiretinal Membrane Foveoschisis. Am J Ophthalmol. 2020;217:152–1.
Baba R, Wakabayashi Y, Umazume K, Ishikawa T, Yagi H, Muramatsu D, et al. Efficacy of the Inverted Internal Limiting Membrane Flap Technique with Vitrectomy for Retinal Detachment Associated with Myopic Macular Holes. Retina. 2017;37:466–71.
Tan Y, Chan W, Gilhotra J. Outer retina restoration is not a prerequisite for visual improvement following the inverted internal limiting membrane flap technique. Clin Exp Ophthalmol. 2020;48:851–53.
Bringmann A, Duncker T, Jochmann C, Barth T, Duncker GIW, Wiedemann P. Spontaneous closure of small full-thickness macular holes: Presumed role of Muller cells. Acta Ophthalmol. 2020;98:e447–e456.
Bringmann A, Jochmann C, Unterlauft JD, Wiedemann R, Rehak M, Wiedemann P. Different modes of foveal regeneration after closure of full-thickness macular holes by (re)vitrectomy and autologous platelet concentrate. Int J Ophthalmol. 2020;13:36–48.
Ghoraba HH, Mansour HO, Elsayed MAA, Zaky AG, Heikal MA, Abdelfattah HM, et al. Risk Factors for Recurrent Myopic Macular Hole Retinal Detachment after Silicone Oil Removal in Patients with Open Flat Macular Hole. Ophthalmologica. 2021;244:118–26.
Tang N, Zhao X, Chen J, Liu B, Lu L. Changes in the Choroidal Thickness after Macular Buckling in Highly Myopic Eyes. Retina. 2021;41:1858–66.
Author contributios
LL was responsible for conducting the research, designing the study and doing the surgery; PL contributed in editing and critical revision of the manuscript; XJZ was responsible for following up the patients, analysing the data, editing and revision of the manuscript; HYS contributed to analyse and interpret the data; ST contributed in critical revision of the manuscript; YBW contributed in interpreting the data; YQC contributed in interpreting the data; SDC was responsible for extracting the data; XH was responsible for extracting the data; BQL was responsible for critical revision of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhao, X., Song, H., Tanumiharjo, S. et al. Macular buckling alone versus combined inverted ILM flap on macular hole-associated macular detachment in patients with high myopia. Eye 37, 2730–2735 (2023). https://doi.org/10.1038/s41433-023-02406-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02406-1