Abstract
Objective
To evaluate the surgical results and the variables affecting the outcomes in conjunctival-limbal allograft transplantation (CLAL).
Methods
Patients who underwent CLAL for limbal stem cell deficiency (LSCD) between 2007 and 2019 were included in the study. LSCD staging was performed according to the staging system developed by the ‘Limbal Stem Cell Working Group’. Stage 1C and higher stage LSCD patients were included in the study. ‘Successful surgical outcome’ was defined as improvement in LSCD stage at 1 year postoperatively.
Results
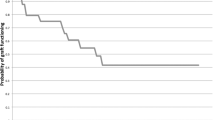
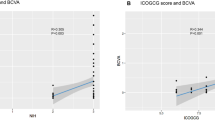
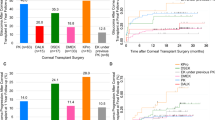
A total of 19 eyes of 19 LSCD patients were included. The mean age of the patients was 40.21 ± 14.65 (6–65) years, and the male/female ratio was 12/7. CLAL was performed in 9 (47.3%) patients with Stage 2B, 9 (47.3%) patients with Stage 3 and 1 (5.4%) with Stage 1C. LSCD aetiology; chemical injury (12), vernal keratoconjunctivitis (2), aniridia (1), corneal degeneration (1), and unknown (3). Surgery was successful in 52.6% of cases. Surgical success was associated with lower LSCD stage (p = 0.04). Lower grades of chemical injury at presentation and a longer time interval between injury and CLAL were associated with higher surgical success (p = 0.001; p = 0.001). The mean postoperative follow-up time was 50.77 ± 29.46 (6–98) months.
Conclusions
Despite graft rejection and long-term use of immunosuppressants, CLAL is still one of the most preferred techniques in the treatment of bilateral LSCD. Preoperative LSCD stage and degree of chemical burn are important factors affecting the surgical outcome. Also, CLAL surgery should not be rushed and should be performed when inflammation has subsided.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Dziasko MA, Daniels JT. Anatomical features and cell-cell interactions in the human limbal epithelial stem cell niche. Ocul Surf. 2016;14:322–30.
Biber JM. Classification of ocular surface disease. In: Holland EJ, Mannis MJ, Lee WB, eds. Ocular surface disease: cornea, conjunctiva and tear film. New York, NY: Elsevier; 2013:35–44.
Lindquist TD. Conjunctivitis: an overview and classification. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. Philadelphia, PA: Mosby Elsevier; 2005:509–20.
Liang L, Sheha H, Tseng SC. Long-term outcomes of keratolimbal allograft for total limbal stem cell deficiency using combined immunosuppressive agents and correction of ocular surface deficits. Arch Ophthalmol. 2009;127:1428–34.
Javadi MA, Jafarinasab MR, Feizi S, Negahban K. Management of mustard gas induced limbal stem cell deficiency and keratitis. Ophthalmology. 2011;118:1272–81.
Movahedan A, Cheung AY, Eslani M, Mogilishetty G, Govil A, Holland EJ. Long-term outcomes of ocular surface stem cell allograft transplantation. Am J Ophthalmol. 2017;184:97–107.
Holland EJ. Epithelial transplantation for the management of severe ocular surface disease. Trans Am Ophthalmol Soc. 1996;94:677–743.
Tsai RJ, Tseng SC. Human allograft limbal transplantation for corneal surface reconstruction. Cornea. 1994;13:389–400.
Tsubota K, Toda I, Saito H, Shinozaki N, Shimazaki J. Reconstruction of the corneal epithelium by limbal allograft transplantation for severe ocular surface disorders. Ophthalmology. 1995;102:1486–95.
Titiyal JS, Sharma N, Agarwal AK, Prakash G, Tandon R, Vajpayee R. Live related versus cadaveric limbal allograft in limbal stem cell deficiency. Ocul Immunol Inflamm. 2015;23:232–9.
Holland EJ, Mogilishetty G, Skeens HM, Hair DB, Neff KD, Biber JM, et al. Systemic immunosuppression in ocular surface stem cell transplantation: results of a 10-year experience. Cornea. 2012;31:655–61.
Solomon A, Ellies P, Anderson DF, Touhami A, Grueterich M, Espana EM, et al. Long-term outcome of keratolimbal allograft with or without penetrating keratoplasty for total limbal stem cell deficiency. Ophthalmology. 2002;109:1159–66.
Dua HS, King AJ, Joseph A. A new classification of ocular surface burns. Br J Ophthalmol. 2001;85:1379–83.
Deng SX, Borderie V, Chan CC, Dana R, Figueiredo FC, Gomes JAP, et al. Global consensus on definition, classification, diagnosis, and staging of limbal stem cell deficiency. Cornea. 2019;38:364–75.
Figueiredo GS, Salvador-Culla B, Baylis OJ, Mudhar HS, Lako M, Figueiredo FC. Outcomes of penetrating keratoplasty following autologous cultivated limbal epithelial stem cell transplantation. Stem Cells. 2018;36:925–31.
Shanbhag SS, Nikpoor N, Rao Donthineni P, Singh V, Chodosh J, Basu S. Autologous limbal stem cell transplantation: a systematic review of clinical outcomes with different surgical techniques. Br J Ophthalmol. 2020;104:247–53.
Lal I, Gupta N, Purushotham J, Sangwan V. Limbal stem cell deficiency: current management. J Clin Ophthalmol Res. 2016;4:3–12.
Sacchetti M, Rama P, Bruscolini A, Lambiase A. limbal stem cell transplantation: clinical results, limits, and perspectives. Stem Cells Int. 2018; 2018:8086269. https://doi.org/10.1155/2018/8086269.
Holland EJ. Management of limbal stem cell deficiency: a historical perspective, past, present, and future. Cornea. 2015;34:S9–15.
Haagdorens M, Van Acker SI, Van Gerwen V, Ni Dhubhghaill S, Koppen C, Tassignon MJ, et al. Limbal stem cell deficiency: current treatment options and emerging therapies. Stem Cells Int. 2016;2016:9798374. https://doi.org/10.1155/2016/9798374
Le Q, Chauhan T, Yung M, Tseng CH, Deng SX. Outcomes of limbal stem cell transplant: a meta-analysis. JAMA Ophthalmol. 2020;138:660–70.
Cheng J, Zhai H, Wang J, Duan H, Zhou Q. Long-term outcome of allogeneic cultivated limbal epithelial transplantation for symblepharon caused by severe ocular burns. BMC Ophthalmol. 2017;17:8.
Deng SX, Kruse F, Gomes JAP, Chan CC, Daya S, Dana R, et al. Global consensus on the management of limbal stem cell deficiency. J Cornea Extern Dis. 2020;39:1291–302.
Bizrah M, Yusuf A, Ahmad S. An update on chemical eye burns. Eye. 2019;33:1362–77.
Ghosh S, Salvador-Culla B, Kotagiri A, Pushpoth S, Tey A, Johnson ZK, et al. Acute chemical eye injury and limbal stem cell deficiency—a prospective study in the United Kingdom. Cornea. 2019;38:8–12.
Korkmaz I, Palamar M, Egrilmez S, Gurdal M, Yagci A, Barut Selver O. Evaluation of limbal stem cell transplant success in ocular chemical injury. Exp Clin Transplant. 2022;10. 6002/ect.2021.0393. https://doi.org/10.6002/ect.2021.0393.
Unlu BH, Utine CA, Durak I. Simple limbal epithelial transplantation in limbal stem cell deficiency after chemical eye injury. Eur Eye Res. 2021;1:47–52. https://doi.org/10.14744/eer.2021.81300
Ozek D, Karaca EE, Kemer OE. Simple limbal epithelial transplantation method in the treatment of unilateral limbal stem cell deficiency due to chemical burn. Eur Eye Res. 2021;1:31–36. https://doi.org/10.14744/eer.2021.32032
Cheung AY, Sarnicola E, Govil A, Holland EJ. Combined conjunctival limbal autografts and living-related conjunctival limbal allografts for severe unilateral ocular surface failure, 2017;36:1570–5.
Baradaran-Rafii A, Eslani M, Djalillian AR. Complications of keratolimbal allograft surgery. Cornea. 2013;32:561–6.
Shimazaki J, Shimmura S, Tsubota K. Donor source affects the outcome of ocular surface reconstruction in chemical or thermal burns of the cornea. Ophthalmology. 2004;111:38–44.
Daya SM, Ilari FA. Living related conjunctival limbal allograft for the treatment of stem cell deficiency. Ophthalmology. 2001;108:126–33. discussion 133-134
Nassiri N, Pandya HK, Djalilian AR. Limbal allograft transplantation using fibrin glue. Arch Ophthalmol. 2011;129:218–22.
Behaegel J, Koppen C, Gerwen V, Tassignon MJ, Dhubhghaill SN. Corneal epithelial restoration after penetrating keratoplasty in repeated failed cultivated limbal stem cell grafts. J EuCornea. 2019;2:6–9.
Ozer MD, Altinkurt E, Alparslan N. The long-term surgical outcomes of conjunctival-limbal autograft procedure with or without penetrating keratoplasty in eyes with unilateral limbal stem cell deficiency. Taiwan J Ophthalmol. 2020;10:22–28.
Author information
Authors and Affiliations
Contributions
MK, IK and OBS were responsible for the conception or design of the work. MK and IK were responsible for the data collection. MK, IK and MPO were responsible for the data analysis, MPO, SE, and AY for interpretation. MK, IK and MPO were responsible for drafting the article. MPO, SE, AY and OBS were responsible for the critical revision of the article. All authors were responsible for the final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kasikci, M., Korkmaz, I., Palamar, M. et al. Evaluation of the factors that influence surgical outcome in conjunctival-limbal allograft transplantation. Eye 37, 2192–2196 (2023). https://doi.org/10.1038/s41433-022-02314-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02314-w