Abstract
Backgrounds/Objectives
The threshold of hypertension was lowered from systolic blood pressure (SBP)/diastolic blood pressure (DBP) 140/90 mmHg to 130/80 mmHg by the 2017 American College of Cardiology/American Heart Association blood pressure (BP) guideline. Thus, we investigated the association between retinal vein occlusion (RVO) occurrence and early-stage hypertension.
Subjects/Methods
This retrospective cohort study used the JMDC Claims Database (JMDC Inc., Tokyo, Japan) between 2005 and 2020. Individuals undergoing health checkups who had data on BP and did not take antihypertensive medications were included. They were classified into four BP groups: normal BP (SBP < 120 mmHg and DBP < 80 mmHg), elevated BP (SBP 120–129 mmHg and DBP < 80 mmHg), stage 1 hypertension (SBP 130–139 mmHg or DBP 80–89 mmHg), and stage 2 hypertension (SBP ≥ 140 mmHg or DBP ≥ 90 mmHg). Date of RVO occurrence was defined as the first date of diagnosis. We estimated adjusted hazard ratios for RVO and central RVO using weighted Cox regression to adjust for potential confounders.
Results
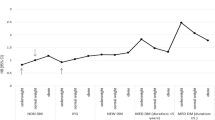
A total of 2,703,264 individuals were eligible. During a mean follow-up of 1,091 days, 3,526 RVO and 828 central RVO events occurred. The adjusted hazard ratios (95% confidence intervals) were 1.37 (1.19–1.57), 1.95 (1.75–2.18), and 3.33 (2.95–3.76) for RVO and 1.44 (1.07–1.93), 2.17 (1.72–2.73), and 3.76 (2.91–4.86) for central RVO in the elevated BP, stage 1 hypertension, and stage 2 hypertension groups, respectively, compared with the normal BP group.
Conclusions
Even individuals with early-stage hypertension showed higher risks for RVO and central RVO than individuals with normal BP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
We used de-identified, individual-level data obtained from the JMDC Claims Database (Tokyo, Japan). The address of their HP is https://www.jmdc.co.jp/en/index. Data are not publicly available.
References
Cugati S, Wang JJ, Rochtchina E, Mitchell P. Ten-year incidence of retinal vein occlusion in an older population: The Blue Mountains Eye Study. Arch Ophthalmol. 2006;124:726–32.
Rogers S, McIntosh RL, Cheung N, Lim L, Wang JJ, Mitchell P, et al. The Prevalence of Retinal Vein Occlusion: Pooled Data from Population Studies from the United States, Europe, Asia, and Australia. Ophthalmology 2010;117:313–319.e1.
United Nations Population Fund. World Population Dashboard. Available at: https://www.unfpa.org/data/world-population-dashboard.
Korobelnik J-F, Larsen M, Eter N, Bailey C, Wolf S, Schmelter T, et al. Efficacy and safety of intravitreal aflibercept treat-and-extend for macular edema in central retinal vein occlusion: the centera study. Am J Ophthalmol. 2021;227:106–15.
Clark WL, Boyer DS, Heier JS, Brown DM, Haller JA, Vitti R, et al. Intravitreal aflibercept for macular edema following branch retinal vein occlusion 52-week results of the vibrant study. Ophthalmology 2016;123:330–6.
Heier JS, Campochiaro PA, Yau L, Li Z, Saroj N, Rubio RG, et al. Ranibizumab for macular edema due to retinal vein occlusions: Long-term follow-up in the HORIZON trial. Ophthalmology 2012;119:802–9.
Brown DM, Campochiaro PA, Singh RP, Li Z, Gray S, Saroj N, et al. Ranibizumab for Macular Edema following Central Retinal Vein Occlusion. Six-Month Primary End Point Results of a Phase III Study. Ophthalmology 2010;117:1124–1133.e1.
Hykin P, Prevost AT, Vasconcelos JC, Murphy C, Kelly J, Ramu J, et al. Clinical Effectiveness of Intravitreal Therapy With Ranibizumab vs Aflibercept vs Bevacizumab for Macular Edema Secondary to Central Retinal Vein Occlusion: A Randomized Clinical Trial. JAMA Ophthalmol. 2019;137:1256–64.
Kymes SM, Vollman D. Recognizing the true cost of medical spending—an assessment of ranibizumab for retinal disorders. JAMA Ophthalmol. 2019;137:1432–3.
Kolar P. Risk factors for central and branch retinal vein occlusion: a meta-analysis of published clinical data. J Ophthalmol. 2014;2014:1–5.
Arakawa S, Yasuda M, Nagata M, Ninomiya T, Hirakawa Y, Doi Y, et al. Nine-year incidence and risk factors for retinal vein occlusion in a general japanese population: the hisayama study. Investig Opthalmology Vis Sci. 2011;52:5905–9.
Zhou JQ, Xu L, Wang S, Wang YX, You QS, Tu Y, et al. The 10-year incidence and risk factors of retinal vein occlusion. Ophthalmology 2013;120:803–8.
Stem MS, Talwar N, Comer GM, Stein JD. A longitudinal analysis of risk factors associated with central retinal vein occlusion. Ophthalmology 2013;120:362–70.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:1269–324.
Mansournia MA, Altman DG. Population attributable fraction. BMJ. 2018;360:k757. https://doi.org/10.1136/bmj.k757.
Nagai K, Tanaka T, Kodaira N, Kimura S, Takahashi Y, Nakayama T. Data resource profile: JMDC claims database sourced from health insurance societies. J Gen Fam Med. 2021;22:118–27.
JMDC Inc. Available at: https://www.jmdc.co.jp/en/jmdc-claims-database/ [Accessed July 26, 2021].
Anon. Risk factors for central retinal vein occlusion. The Eye Disease Case-Control Study Group. Arch Ophthalmol 1996;114:545–54.
Mitchell P, Smith W, Chang A. Prevalence and Associations of Retinal Vein Occlusion in Australia: The Blue Mountains Eye Study. Arch Ophthalmol. 1996;114:1243–7.
Lee KS, Nam KH, Kim DW, Kang EC, Koh HJ. Risk of Retinal Vein Occlusion in Patients With End-Stage Renal Disease: A 12-Year, Retrospective, Nationwide Cohort Study in South Korea. Investig Opthalmology Vis Sci. 2018;59:39–44.
Rehak M, Rehak J, Müller M, Faude S, Faude F, Siegemund A, et al. The prevalence of activated protein C (APC) resistance and factor V Leiden is significantly higher in patients with retinal vein occlusion without general risk factors: Case-control study and meta-analysis. Thromb Haemost. 2008;99:925–9.
Ministry of Health, Labour and Welfare. Standard Medical Examination / Health Guidance Program. Available at: https://www.mhlw.go.jp/bunya/shakaihosho/iryouseido01/info03a.html [Accessed August 7, 2021].
Paik DW, Han K, Kang SW, Ham D-I, Kim SJ, Chung T-Y, et al. Differential effect of obesity on the incidence of retinal vein occlusion with and without diabetes: a Korean nationwide cohort study. Sci Rep. 2020;10:10512.
Newman-Casey PA, Stem M, Talwar N, Musch DC, Besirli CG, Stein JD. Risk factors associated with developing branch retinal vein occlusion among enrollees in a united states managed care plan. Ophthalmology 2014;121:1939–48.
Klein R, Klein BE, Moss SE, Meuer SM. The epidemiology of retinal vein occlusion: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc. 2000;98:133–43.
Sperduto RD, Hiller R, Chew E, Seigel D, Blair N, Burton TC, et al. Risk factors for hemiretinal vein occlusion: comparison with risk factors for central and branch retinal vein occlusion: the eye disease case-control study. Ophthalmology 1998;105:765–71.
Shahsuvaryan ML, Melkonyan AK. Central retinal vein occlusion risk profile: a case-control study. Eur J Ophthalmol. 2003;13:445–52.
Kaneko H, Yano Y, Itoh H, Morita K, Kiriyama H, Kamon T, et al. Association of Blood Pressure Classification Using the 2017 American College of Cardiology/American Heart Association Blood Pressure Guideline With Risk of Heart Failure and Atrial Fibrillation. Circulation 2021;143:2244–53.
Austin PC. Using the Standardized Difference to Compare the Prevalence of a Binary Variable Between Two Groups in Observational Research. Commun Stat - Simul Comput. 2009;38:1228–34.
Pocock SJ, Clayton TC, Altman DG. Survival plots of time-to-event outcomes in clinical trials: good practice and pitfalls. Lancet. 2002;359:1686–9.
Patino CM, Ferreira JC. Test for trend: evaluating dose-response effects in association studies. J Bras Pneumol. 2016;42:240–240.
Hess KR. Graphical methods for assessing violations of the proportional hazards assumption in cox regression. Stat Med. 1995;14:1707–23.
Therneau T, Crowson C, Atkinson E Using time dependent covariates and time dependent coefficients in the cox model. 2022. Available at: https://cran.r-project.org/web/packages/survival/vignettes/timedep.pdf.
Yoshida K, Hernández-Díaz S, Solomon DH, Jackson JW, Gagne JJ, Glynn RJ, et al. Matching weights to simultaneously compare three treatment groups: Comparison to three-way matching. Epidemiol Camb Mass. 2017;28:387–95.
Natarajan S, Lipsitz SR, Rimm E. A simple method of determining confidence intervals for population attributable risk from complex surveys. Stat Med. 2007;26:3229–39.
Yano Y, Reis JP, Colangelo LA, Shimbo D, Viera AJ, Allen NB, et al. Association of Blood Pressure Classification in Young Adults Using the 2017 American College of Cardiology/American Heart Association Blood Pressure Guideline With Cardiovascular Events Later in Life. JAMA 2018;320:1774–82.
Son JS, Choi S, Kim K, Kim SM, Choi D, Lee G, et al. Association of Blood Pressure Classification in Korean Young Adults According to the 2017 American College of Cardiology/American Heart Association Guidelines With Subsequent Cardiovascular Disease Events. JAMA. 2018;320:1783–92.
Matsuoka S, Kaneko H, Yano Y, Itoh H, Fukui A, Morita K, et al. Association Between Blood Pressure Classification Using the 2017 ACC/AHA Blood Pressure Guideline and Retinal Atherosclerosis. Am J Hypertens. 2021;34:1049–56.
Jones DW, Whelton PK, Allen N, Clark D, Gidding SS, Muntner P, et al. Management of Stage 1 Hypertension in Adults With a Low 10-Year Risk for Cardiovascular Disease: Filling a Guidance Gap: A Scientific Statement From the American Heart Association. Hypertension 2021;77:e58–e67.
Tamiya R, Miyake M, Kido A, Hiragi S, Tamura H, Kuroda T, et al. Validation study of the claims-based definition for age-related macular degeneration at a single university hospital in Japan. Jpn J Ophthalmol. 2021;65:388–94.
Gulmez M, Tekce A. Blood pressure variability in patients with branch retinal vein occlusion. Retina 2020;40:2045–9.
Funding
This work was supported by grants from the Ministry of Health, Labour and Welfare, Japan (21AA2007) and the Ministry of Education, Culture, Sports, Science and Technology, Japan (20H03907 and 21H03159). The sponsor or funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
YH had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: YH, HK, AO, HY, and RO. Acquisition, analysis, and interpretation of data: YH, HK, SA, AO, HM, HY, RO. Drafting of the manuscript: YH, HK, HY, and AO. Critical revision of the manuscript for important intellectual content: YH. Statistical analysis: YH, SA, AO, and HY. Obtained funding: HY. Administrative, technical, or material support: None. Study supervision: HY and AO.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41433_2022_2241_MOESM3_ESM.docx
Hazard ratios for any retinal vein occlusion and central retinal vein occlusion before and after weighting in the individuals aged <40 years
41433_2022_2241_MOESM4_ESM.docx
Hazard ratios for any retinal vein occlusion and central retinal vein occlusion before and after weighting in the individuals aged ≥40 years
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hashimoto, Y., Kaneko, H., Aso, S. et al. Association between retinal vein occlusion and early-stage hypertension: A propensity score analysis using a large claims database. Eye 37, 1741–1747 (2023). https://doi.org/10.1038/s41433-022-02241-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02241-w