Abstract
Objectives
To evaluate the association between serum retinol concentration and normal-tension glaucoma (NTG).
Methods
A total of 345 study subjects were recruited in a prospective cross-sectional study: 101 patients with NTG, 106 patients with high-pressure primary open-angle glaucoma (POAG) and 138 healthy control subjects. Serum retinol concentration in fasting blood samples was determined by ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS). All study subjects were given complete ophthalmic examinations and diagnosed by two glaucoma sub-specialists.
Results
Serum retinol concentrations in NTG, POAG, and controls were 338.90 ± 103.23 ng/mL, 405.22 ± 114.12 ng/mL, and 408.84 ± 122.36 ng/mL respectively. NTG patients had lower serum retinol concentrations than POAG (p < 0.001) or healthy controls (p < 0.001). There was no statistical difference between the POAG and healthy controls (p = 0.780). Higher proportion of NTG patients (37.6%) than POAG (17.9%) or controls (21.7%) had serum retinol concentrations lower than 300 ng/mL. Serum retinol was positively correlated with optic nerve sheath diameter (ONSD) (r = 0.349, p = 0.001) in glaucoma patients and not associated with any other demographic features or ophthalmic biometric parameters in the NTG patients. Multivariate logistic regression showed that serum retinol (OR = 0.898, 95CI%: 0.851–0.947) was associated with incident NTG.
Conclusions
NTG patients had lower serum retinol concentrations. Serum retinol uniquely associated with NTG makes it a new potential option for the diagnosis and treatment of the disease.
Similar content being viewed by others
Introduction
In East Asian populations, normal-tension glaucoma (NTG) is known to be more prevalent than the high-pressure form of primary open-angle glaucoma (POAG), accounting for about 70% of POAG in Chinese and 92% in Japanese [1, 2]. The mechanism of NTG is complex [3]. While intraocular pressure (IOP) should be consistently low in NTG patients, controlling IOP at a low level can inhibit glaucomatous progression in some patients but not the others. In one study 38% open-angle glaucoma (OAG) patients still had visual field damage after controlling IOP [4]. In addition to IOP, ocular blood flow, which affects blood flow to the optic nerve [5], and trans-laminar pressure gradient, which governs cerebrospinal fluid pressure across the lamina cribrosa [6], are known to be involved in the pathogenesis of NTG.
Vitamin A is a generic term for a group of related organic compounds that include retinol, retinal, retinoic acid and several provitamin A carotenoids. It is essential for vision, immunity, reproduction, cell growth, and cell differentiation [7]. The various biological activities of vitamin A that affect intracranial pressure (ICP) [8], anti-oxidation and anti-amyloid β [9, 10], makes it closely associated with NTG. Vitamin A intake was found to be associated with incidence of NTG in population-based studies as antioxidant nutrients. The Rotterdam study on European patients with OAG, in which NTG accounted for 84.6% of the glaucoma patients, found the association of low intake of vitamin A with an increased risk of glaucoma [11]. Consistent results were shown in two subsequent cross-sectional studies on Japanese Americans and South Koreans [12, 13].
However, studies about vitamin A dietary intake were affected by subjective rather than objective factors. To further investigate the association and eliminate bias from self-report intake, serum levels of retinol, the most used biomarkers of vitamin A status according to WHO suggestions have been adopted [14]. Retinol is the predominant circulating form of vitamin A in the blood. Serum retinol concentration is homeostatically controlled and does not fall until body stores are significantly compromised [14]. It reflects an individual’s vitamin A status even when the body’s reserve of vitamin A is low. A European study showed that the serum vitamin A of NTG was lower than that of POAG [15], while a Japanese study reported no difference in serum vitamin A level between NTG and healthy people [16].
There are uncertainties and inconsistencies in the association of serum retinol and NTG. In this study, we aimed to evaluate serum retinol concentrations, to be determined by an advanced information-rich chromatographic procedure, in a cohort of NTG, POAG and normal controls with strict inclusion and exclusion criteria.
Methods
This study is a prospective cross-sectional study conducted at the Beijing Tongren Hospital, Beijing, China. The Medical Ethics Committee of Beijing Tongren Hospital approved the study. The study was conducted according to the Declaration of Helsinki and was registered at http://www.chictr.org.cn (registration number: ChiCTR1900028122). All participants gave written informed consent.
Participants
The NTG group involved 101 patients with NTG, the POAG group 106 patients with high-pressure POAG, and the control group 138 healthy subjects (the sample size estimation is in the Supplementary File). All glaucoma subjects were recruited at the Glaucoma Clinic, Beijing Tongren Hospital from May 2017 to January 2020. Diagnosis of glaucoma was based on: (1) glaucomatous abnormalities of the disc and optic nerve head, including notches in the optic nerve rim and localized or segmental loss of the retinal nerve fiber layer, (2) visual field loss including a paracentral, arcuate, or Seidel’s scotoma or a nasal step consistent with the glaucomatous structural abnormalities, and (3) open or non-occludable anterior chambers with gonioscopy. All the above three criteria are necessary. In addition, two glaucoma sub-specialists with more than 20 years of clinical experiences in glaucoma (W.H. and W.N.) separately provided independent diagnosis for each study subject. They were blinded to the patients’ diagnoses when conducting their assessments. Both had to agree. If there was disagreement, the patient would be excluded from the study.
The NTG patients never had IOP higher than 21 mmHg since the time of diagnosis. Patients in the POAG group had high IOP (IOP > 21 mmHg). All glaucoma subjects had at least one 24 h IOP measurement by Goldmann tonometry without any ocular hypotensive medication. All glaucoma patients were followed regularly for 3–6 months after serum retinol measurement. During follow-up, those NTG patients found to have elevated IOP were excluded from further studies.
We enrolled healthy subjects aged 18–70 years who attended the Health Center of Beijing Tongren Hospital for routine health check from May 2017 to January 2020. All subjects had complete information including IOP and color fundus photography. We did not enroll patients with previous history of eye disease, IOP > 21 mmHg, or having suspected glaucoma changes in fundus photography.
Exclusion criteria of all study subjects who: (1) took multivitamin tablets or other retinoids within 1 week of testing; (2) had fever, diarrhea and infection within 2 weeks of testing; (3) were pregnant or had given birth or breastfeeding within prior 2 months; (4) had liver and kidney diseases that may affect retinol metabolism; (5) had myopic refractive error of more than eight diopters; (6) were diagnosed with neurological disease, congenital glaucoma, or secondary glaucoma.
Serum retinol measurements
We strictly controlled the collection of 5 mL overnight fasting blood samples between 7:00 am and 10:00 am by a vacuum blood collection tube. Serum was collected after centrifugation at 3000 rpm for 10 min. We stored 0.8 mL of serum samples at −80 °C for <3 months prior to retinol measurement. The samples were encoded with randomization of the NTG, POAG and control samples. The investigator who carried out the serum analysis could only see the sample number and was not informed of any clinical information.
Standard and sample preparation
Standards and samples were processed under red light to avoid photoisomerization and photodegradation of target compounds. Standard stock solution of retinol (1.061 mg/mL) was prepared in methanol. A series of calibration standards at eight concentrations (10, 20, 50, 100, 200, 500, 1000, and 2000 ng/mL) were prepared by dilution with methanol from the stock solution. The isotope internal standard (d8-retinol) was also prepared in methanol at the final concentration of 200 ng/mL. All solutions were stored at −80 °C until analysis.
100 ul serum sample in a clean centrifuge tube was added 100 ul internal standard solution (d8-retinol 200 ng/mL), vortexed for 3 min and added 600 ul hexane followed by further vortex mixing for 5 min and centrifugation at 4 °C at 15000 rpm for 10 min. 400 ul supernatant was transferred into another centrifuge tube and dried under nitrogen at room temperature. The sample residue was re-dissolved in 150 ul 80% acetonitrile and centrifuged at 15000 rpm for 3 min at 4 °C. Finally, 120 ul supernatant was transferred to a 96 well plate for analysis.
UPLC-MS/MS analysis
Analysis was conducted on an ultra-performance liquid chromatography-tandem electrospray-triple quadrupole mass spectrometry system (Xevo TQD, Waters, Milford, MA). A 10 μL aliquot of sample was injected into a Waters BEH C18 column (50 mm × 2.1 mm i.d., 1.7 μm particle size) for separation of sample molecules on a binary gradient of water (A) and 2 mmol ammonium formate methanol (B) both containing 0.1% formic acid at a flow rate of 0.4 mL min−1. The gradient: 0 min 70% B, 2 min 90% B, 2.5 min 100% B, 4 min 100% B, then immediately returned to 70% B and maintained for 1.5 min to re-equilibrate. The total chromatographic run time was 5.5 min at column temperature of 40 °C.
The mass spectrometry was operated in positive ionization mode (ESI+) with multiple reaction monitoring. Source temperature was 150 °C. The capillary voltage was 3.0 kV. Nitrogen served as de-solvation gas with a flow of 800 L h−1 at 400 °C.
Ophthalmic examinations
All study subjects undertook ophthalmic measurements for biometric parameters within 1 week before blood sample collection. We conducted best-corrected visual acuity, slit-lamp bio-microscopy, gonioscopy and non-contact tonometry. Photography of the optic disk and retinal nerve fibre layer were assessed using the fundus camera EOS D60 (Canon Co. Utsunomiyashi, Tochigiken, Japan). Visual field was assessed by automated perimetry on a Zeiss Humphrey Field Analyzer (Carl Zeiss Meditec Inc., Dublin, CA). Axial length was measured by optical biometry (Lenstar900, Haag-Streit, Switzerland) and central corneal thickness (CCT) by anterior segment Optical Coherence Tomography (Casia ss-1000, Tomey Corporation, Nagoya, Japan). 24 h IOP measurement was conducted in hospital ward with Goldmann applanation tonometry at 2 AM, 6 AM, 8 AM, 10 AM, 2 PM, 6 PM, and 10 PM. All study subjects were invited for the measurement of optic nerve sheath diameter (ONSD) at 3 mm behind the globe. Among them 55 NTG patients and 38 POAG patients accepted the invitation. ONSD was measured on B-mode ultrasound using a 12.5 MHz linear array probe (L15-7io; Philips, Bothell, WA) as previously described [17].
Statistical analysis
The Shapiro test was used to check the distribution of the quantitative data. Data at normal distribution were expressed as mean ± standard deviation, and data not normally distributed were described by median and quartile. Serum retinol was expressed as both mean ± standard deviation and median and quartile. We used One-way ANOVA to compare normally distributed parameters among the study groups. The Kruskal–Wallis test was used to compare the non-normally distributed parameters and Chi-square test to compare qualitative parameters. The Post Hoc test was conducted if there was statistical difference among the study groups. The significance level was set to be 0.05, and adjusted to 0.017 according to Bonferroni criteria when Post Hoc test was done. Spearman correlation analysis was performed to study associations between serum retinol and other variables. Logistic regression was done to explore the risk factors of NTG. All statistical analyses were performed using an open-source R program (Version 3.6.1).
Results
Demographic features and ophthalmic biometric parameters of the three groups of study subjects were shown in Table 1. Body mass index (BMI) in the healthy control group was significantly higher than those in NTG (t = −2.941, p = 0.004). Mean artery pressure (MAP) in the healthy control group were higher than those in NTG (Z = −4.783, p < 0.001) or POAG (Z = −3.770, p < 0.001). The peak IOP (Z = 140.892, p < 0.001) and ONSD (Z = 2.151, p = 0.032) were significantly lower in NTG than in POAG. There were no significant differences in the other parameters among the study groups.
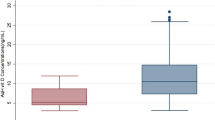
The mean serum retinol concentration in NTG patients at 338.90 ± 103.23 ng/mL was the lowest when compared with high-pressure POAG patients (405.22 ± 114.12 ng/mL) and healthy controls (408.84 ± 122.36 ng/mL). The median level of serum retinol concentrations in NTG, POAG and healthy groups were 321.24 (interquartile range, IQR: 263.81–395.50) ng/mL, 390.78 (319.10–469.10) ng/mL and 402.05 (316.39–475.52) ng/mL respectively (Fig. 1). The serum retinol concentration in the NTG group was statistically lower than that in POAG (Z = −4.379, p < 0.001) or control (Z = −4.543, p < 0.001). There was no statistical difference in serum retinol concentration between POAG and controls (Z = −2.79, p = 0.780). In the NTG group, 38 out of 101 (37.6%) patients had serum retinol concentrations lower than 300 ng/mL, in comparison with only 19 out of 106 (17.9%) POAG patients and 30 out of 138 (21.7%) controls (Fig. 2).
The associations of serum retinol in all three groups were shown in Table 2. In the controls, serum retinol was associated with gender (r = 0.224, p = 0.008), age (r = −0.239, p = 0.005), height (r = 0.234, p = 0.006), weight (r = 0.207, p = 0.016) and MAP (r = 0.181, p = 0.034), but not associated with BMI and IOP. In the POAG group, serum retinol was positively associated with gender (r = 0.338, p < 0.001), height (r = 0.260, p = 0.008) and weight (r = 0.229, p = 0.018), but not associated with age, BMI, MAP and IOP. Notably, in the NTG patients, serum retinol was not associated with any of these parameters. There was a positive correlation between serum retinol and ONSD (r = 0.349, p = 0.001) in all 93 subjects (55 with NTG and 38 with POAG) (Fig. 3).
BMI, MAP (Table 1), and serum retinol (Fig. 1) were statistically different between the NTG and the healthy control group. Multivariate logistic regression analysis showed a significant association of serum retinol with incident NTG after adjustment for BMI and MAP (OR = 0.898, 95CI%:0.851–0.947) (p < 0.001). After adjustment by multivariate logistic regression, MAP (OR = 0.959, 95CI%:0.935–0.983) (p < 0.001) was also significantly associated with incident NTG, BMI was not significantly associated with incident NTG (p = 0.337).
Discussion
Multiple studies have suggested there is an association between dietary intake of vitamin A and glaucoma [18]. For high-pressure glaucoma, two prospective cohorts, the Nurses Health Study and the Health Professional Follow-up Study, showed no significant correlation between vitamin A intake and OAG (75.6% had IOP higher than 21 mmHg) [19]. However, reported studies on NTG suggested that low vitamin A intake may be a risk factor. A European prospective cohort with 3502 subjects of OAG with 84.6% NTG showed low intake of retinol equivalents as risk [11]. Results in a cross-sectional study in Japanese Americans were consistent [12]. In the Korean National Health and Nutrition Examination Survey, vitamin A intake of NTG subjects was not associated with NTG after multivariate analysis [20]. However, for low BMI female subjects, NTG had significant association with lower vitamin A and β-carotene intake in a recent Korean study [13]. These reported results indicated association of vitamin A with glaucoma at normal IOP.
In our study, there were significantly lower serum retinol concentrations in patients with NTG than in high-pressure POAG patients or in healthy controls (Fig. 1). Serum retinol concentrations below 300 ng/mL were found among 37.6% of NTG, 21.74% of healthy subjects and 17.92% of POAG. NTG patients have almost a twofold risk of vitamin A deficiency compared with healthy subjects or POAG patients (Fig. 2). Notably, there was no significant difference between the healthy controls and high-pressure POAG patients in serum retinol concentration and in the proportion of study subjects with serum retinol concentrations below 300 ng/mL. There is a unique association between low serum retinol and NTG.
Whether serum retinol levels are lower in NTG patients than in healthy controls or POAG patients has been inconsistent in reported studies. Belmonte et al. reported lower serum retinol levels in NTG patients (n = 13) compared with POAG patients (n = 48) [15]. Similarly, vitamin A in NTG was lower than POAG or controls, although statistically insignificant, in another study: mean serum vitamin A concentration of 304 ± 158 ng/mL in NTG (n = 15), 397 ± 133 ng/mL in POAG (n = 48) and 379 ± 120 ng/mL in healthy controls (n = 75) [21]. In a study on multiple serum antioxidant levels in 47 NTG patients and 44 controls, there was no significant difference in serum vitamin A levels between them [16]. Reversed-phase high-performance liquid chromatography with electrochemical detection was used and the reported mean values of serum vitamin A were close to or exceeded the human serum vitamin A reference range (300–800 ng/mL) [22]. However, the study did not include patients with high-pressure POAG. Serum vitamin A concentrations of a group of Turkish glaucoma patients (n = 150), undifferentiated for sub-types with no IOP information, was higher than that of controls (n = 31) [23]. The sample sizes of these studies were small.
In a larger study, no association of glaucoma with serum vitamin A concentration was found in 2912 non-institutionalized glaucoma patients randomly recruited from the National Health and Nutrition Examination Survey in USA [24]. The glaucoma was self-reporting and undifferentiated for glaucoma types with no information of IOP. Also, the serum vitamin A levels were based on the National Health and Nutrition Examination Survey records. The results, therefore, were not conclusive. All these preliminary studies were useful and interesting but could not be interpreted conclusively.
In order to consolidate the association of serum retinol with NTG, we conduct this study in strict inclusive criteria of NTG, high-pressure POAG and control subjects. Fasting serum retinol was determined by ultra-performance liquid chromatography with information-rich tandem mass spectrometry. In this assay protocol, an isotope internal was added to overcome the matrix effect, thus ensuring the accuracy of the measurement. With over a hundred study subjects in each subject group, we have confirmed NTG patients have lower serum retinol than controls or the high-pressure POAG patients.
NTG patients also showed lower BMI and MAP (Table 1). Hypotension had been thought to impair perfusion of the optic nerve [25]. It was likely a risk factor in the development of NTG in patients with Flammer syndrome [26]. As for BMI, every unit increase was associated with a 6% reduced risk of NTG in a study involving 228 female NTG patients [27]. In our study, serum retinol of controls was positively associated with height and weight, but not with BMI (Table 2). While there was a positive correlation between blood pressure and serum retinol in the controls, there was no such correlation in the NTG patients. Low BMI and MAP may not be the cause of low serum retinol in NTG. In addition, multivariate logistic regression showed that serum retinol remained significantly associated with incident NTG after adjustment for BMI and MAP. These results indicate that low serum retinol in NTG patients may be a risk factor independent of BMI and blood pressure.
There was no difference in age and gender among the three groups (Table 1). Age and gender were also associated with serum retinol in controls, consistent with generally accepted conclusions [22]. NTG is more likely to occur in older, female [28], and hypotensive individuals [25]. Therefore, we conclude that although the low serum retinol level is not caused by low BMI and hypotension in NTG patients, lower serum retinol in older, female, and hypotensive people seem to be associated with NTG in these people.
In addition, a comparison of the ophthalmic biometric parameters of the two glaucoma groups showed that only peak IOP and ONSD were different between NTG and POAG (Table 1). Peak IOP has no correlation with serum retinol (Table 2). Intriguingly, as a parameter of noninvasive measurement of ICP [29], ONSD at 3 mm behind the globe using B-mode ultrasound was different between NTG and POAG, as well as significantly associated with serum retinol. The ONSD of the NTG patients was significantly lower than that of the POAG patients, which was related to the trans-laminar pressure gradient mechanism of NTG. ICP was reportedly lower in NTG than POAG and controls [30]. As a part of the central nervous system, the intraorbital subarachnoid space surrounding the optic nerve is subject to the same pressure changes as the intracranial compartment. Previous studies have shown that ONSD is strongly correlated with the ICP value [31]. A magnetic resonance imaging study and an ultrasonography imaging study independently showed that the lower ICP of NTG patients caused its ONSD to be lower than that of POAG and normal controls [17, 32]. In our study, ONSD in patients with glaucoma was positively correlated with serum retinol concentration (Fig. 3), which may be related to the effect of serum retinol on ICP.
Serum retinol has a specific ability to affect ICP. Some patients with intracranial hypertension without any secondary factors had been found to have higher serum retinol concentrations [33]. In another study, the serum and cerebrospinal fluid retinol concentrations in idiopathic intracranial hypertension patients were higher than those in the control group after other factors were corrected [34]. Libien et al. suggested that serum retinol levels changed the amount of retinol taken up by the choroid plexus epithelium and affected the conversion of retinol to all-trans retinoic acid in target cells, eventually affecting ICP [8].
There are limitations in this study. (1) The causal association between NTG and low retinol remains to be investigated through experimental and prospective studies. (2) We focused on the vitamin A levels in NTG patients and we found a correlation. However, there are other confounding nutrients, such as vitamins B1, B3, B12, C, D and E, which have also been shown to affect the pathogenesis of glaucoma [18]. The interrelationships of various nutrients in NTG have to be investigated. (3) Ideally, ICP should be measured directly through a lumbar puncture. However, it is not accepted by most ophthalmic patients due to its invasiveness. We measured ONSD as an alternative. Although ONSD has a high correlation with ICP, it still has some controversies and cannot fully represent ICP. The relationship between low retinol and abnormal ICP in NTG still has to be explored.
In conclusion, serum retinol concentration was significantly lower in patients with NTG compared with patients with high-pressure POAG and healthy controls. For NTG patients, risk factors including old age, females, hypotension, and low BMI are not responsible for the low serum retinol level, which may be related to low ICP and abnormal trans-laminar pressure gradient. Although the role of serum retinol in the pathogenesis of NTG remains to be further studied, its unique association with NTG provides a potential option for the diagnosis and treatment.
Supplementary information is available at Eye’s website
Summary
What was known before
-
There are uncertainties and inconsistencies in the association of serum retinol and glaucoma.
What this study adds
-
Patients with NTG have lower serum retinol than healthy people or high-pressure glaucoma controls.
-
There is a unique association between retinol and NTG after adjustment for other risk factors.
-
The association between retinol and NTG seems to be related to changes in trans-laminar pressure gradient.
References
Zhao J, Solano MM, Oldenburg CE, Liu T, Wang Y, Wang N, et al. Prevalence of normal-tension glaucoma in the Chinese population: a systematic review and meta-analysis. Am J Ophthalmol. 2019;199:101–10.
Iwase A, Suzuki Y, Araie M, Yamamoto T, Abe H, Shirato S, et al. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology. 2004;111:1641–8.
Killer HE, Pircher A. Normal tension glaucoma: review of current understanding and mechanisms of the pathogenesis. Eye (Lond). 2018;32:924–30.
Cockburn DM. Does reduction of intraocular pressure (IOP) prevent visual field loss in glaucoma? Am J Optom Physiol Opt. 1983;60:705–11.
Flammer J, Orgül S, Costa VP, Orzalesi N, Krieglstein GK, Serra LM, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002;21:359–93.
Jonas JB, Wang N, Yang D, Ritch R, Panda-Jonas S. Facts and myths of cerebrospinal fluid pressure for the physiology of the eye. Prog Retin Eye Res. 2015;46:67–83.
Higdon J, Drake VJ. Evidence-based approach to vitamins and minerals: health benefits and intake recommendations. 2nd ed. New York: Thieme Medical Publishers; 2003.
Libien J, Blaner WS. Retinol and retinol-binding protein in cerebrospinal fluid: can vitamin A take the “Idiopathic” out of idiopathic intracranial hypertension? J Neuroophthalmol. 2007;27:253–7.
Raman R, Vaghefi E, Braakhuis AJ. Food components and ocular pathophysiology: a critical appraisal of the role of oxidative mechanisms. Asia Pac J Clin Nutr. 2017;26:572–85.
Takasaki J, Ono K, Yoshiike Y, Hirohata M, Ikeda T, Morinaga A, et al. Vitamin A has anti-oligomerization effects on amyloid-β in vitro. J Alzheimers Dis. 2011;27:271–80.
Ramdas WD, Wolfs RCW, Kiefte-de Jong JC, Hofman A, de Jong PTVM, Vingerling JR, et al. Nutrient intake and risk of open-angle glaucoma: the Rotterdam Study. Eur J Epidemiol. 2012;27:385–93.
Yoserizal M, Hirooka K, Yoneda M, Ohno H, Kobuke K, Kawano R, et al. Associations of nutrient intakes with glaucoma among Japanese Americans. Med (Baltim). 2019;98:e18314.
Lee JY, Kim JM, Lee KY, Kim B, Lee MY, Park KH. Relationships between Obesity, Nutrient Supply and Primary Open Angle Glaucoma in Koreans. Nutrients. 2020;12:878.
World Health Organization. Serum retinol concentrations for determining the prevalence of vitamin A deficiency in populations. Geneva: World Health Organization; 2011.
Belmonte A, Tormo C, Lopez N, Villalba C, Fernandez C, Hernandez F. Vitamins A, E, B12 and folate levels in different types of glaucoma. Clin Chem Lab Med. 2011;49:S816.
Yuki K, Murat D, Kimura I, Ohtake Y, Tsubota K. Reduced-serum vitamin C and increased uric acid levels in normal-tension glaucoma. Graefes Arch Clin Exp Ophthalmol. 2010;248:243–8.
Liu H, Yang D, Ma T, Shi W, Zhu Q, Kang J, et al. Measurement and associations of the optic nerve subarachnoid space in normal tension and primary open-angle glaucoma. Am J Ophthalmol. 2018;186:128–37.
Ramdas WD, Schouten JSAG, Webers CAB. The effect of vitamins on glaucoma: a systematic review and meta-analysis. Nutrients. 2018;10:359.
Kang JH, Pasquale LR, Willett W, Rosner B, Egan KM, Faberowski N, et al. Antioxidant intake and primary open-angle glaucoma: a prospective study. Am J Epidemiol. 2003;158:337–46.
Jung KI, Kim YC, Park CK. Dietary niacin and open-angle glaucoma: the Korean national health and nutrition examination survey. Nutrients. 2018;10:387.
López-Riquelme N, Villalba C, Tormo C, Belmonte A, Fernandez C, Torralba G, et al. Endothelin-1 levels and biomarkers of oxidative stress in glaucoma patients. Int Ophthalmol. 2015;35:527–32.
Sawyer BG. Tietz fundamentals of clinical chemistry and molecular diagnostics. 7th ed. St. Louis, MO: Elsevier; 2015.
Engin KN, Yemişci B, Yiğit U, Ağaçhan A, Coşkun C. Variability of serum oxidative stress biomarkers relative to biochemical data and clinical parameters of glaucoma patients. Mol Vis. 2010;16:1260–71.
Wang SY, Singh K, Lin SC. Glaucoma and vitamins A, C, and E supplement intake and serum levels in a population-based sample of the United States. Eye (Lond). 2013;27:487–94.
Leske MC, Wu S-Y, Nemesure B, Hennis A, Group BES. Incident open-angle glaucoma and blood pressure. Arch Ophthalmol. 2002;120:954–9.
Konieczka K, Ritch R, Traverso CE, Kim DM, Kook MS, Gallino A, et al. Flammer syndrome. EPMA J. 2014;5:11.
Pasquale LR, Willett WC, Rosner BA, Kang JH. Anthropometric measures and their relation to Incident primary open-angle glaucoma. Ophthalmology. 2010;117:1521–9.
Mallick J, Devi L, Malik P, Mallick J. Update on normal tension glaucoma. J Ophthalmic Vis Res. 2016;11:204–8.
Soldatos T, Chatzimichail K, Papathanasiou M, Gouliamos A. Optic nerve sonography: a new window for the non-invasive evaluation of intracranial pressure in brain injury. Emerg Med J. 2009;26:630–4.
Ren R, Jonas JB, Tian G, Zhen Y, Ma K, Li S, et al. Cerebrospinal fluid pressure in glaucoma: a prospective study. Ophthalmology. 2010;117:259–66.
Wang LJ, Chen LM, Chen Y, Bao LY, Zheng NN, Wang YZ, et al. Ultrasonography assessments of optic nerve sheath diameter as a noninvasive and dynamic method of detecting changes in intracranial pressure. JAMA Ophthalmol. 2018;136:250–6.
Wang N, Xie X, Yang D, Xian J, Li Y, Ren R, et al. Orbital cerebrospinal fluid space in glaucoma: the Beijing intracranial and intraocular pressure (iCOP) Study. Ophthalmology. 2012;119:2065–2073.e2061.
Jacobson DM, Berg R, Wall M, Digre KB, Corbett JJ, Ellefson RD. Serum vitamin A concentration is elevated in idiopathic intracranial hypertension. Neurology. 1999;53:1114.
Warner JEA, Larson AJ, Bhosale P, Digre KB, Henley C, Alder SC, et al. Retinol-binding protein and retinol analysis in cerebrospinal fluid and serum of patients with and without idiopathic intracranial hypertension. J Neuroophthalmol. 2007;27:258–62.
Author information
Authors and Affiliations
Contributions
RP, SF, YS, YG, YX, and NW designed the study. NW acquired funding and supervised the research team. RP, DM, YZ, YF, JL, YW, HH, and JC recruited and examined study subjects. HL, QZ, YS and HW conducted ophthalmic examinations. XL and JQ conducted biochemical tests. JP and CC conducted the chromatographic and mass spectrometric assays. RP, SF, YS, YG, YX and KC performed data analysis. RP, CPP and NW interpreted the data. RP, SAL, and CX drafted the paper. RP, CPP, SAL, and RNW revised the paper.
Funding
This study was funded by the National Natural Science Foundation of China (81730027), Beijing University-CMU, Advanced Innovation Centre for Big Data-Based Precision Medicine, Ophthalmic Subcenter (BHME2018-2019) and Sanming Project of Medicine in Shenzhen (SZSM201512045). The funding organization had no role in the design or conduct of this research.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the paper, or in the decision to publish the results.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Pang, R., Feng, S., Cao, K. et al. Association of serum retinol concentration with normal-tension glaucoma. Eye 36, 1820–1825 (2022). https://doi.org/10.1038/s41433-021-01740-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01740-6