Abstract
Background
Water exposure during contact lens wear has been associated with contact lens disease including microbial keratitis and sterile corneal infiltrates. Despite the documented risks, water exposure is common amongst lens wearers. This study aimed to determine the effect of water education in the form of “no-water” lens case stickers on water-contact behaviours and storage case contamination.
Methods
In a prospective, masked, randomised controlled trial, 200 daily lens wearers were randomised to either receive a storage case with a “no-water” sticker (test) or without a “no-water” sticker (control). Both groups received written compliance information. Participants completed a self-administered lens hygiene questionnaire at baseline and after 6 weeks. Microbial analysis of used storage cases, collected at both study visits, was conducted using ATP and limulus amebocyte lysate (LAL) assays for overall microbial contamination and endotoxin levels, respectively. A one-way ANCOVA and multiple logistic regression determined the change in water-contact behaviours and storage case contamination over time.
Results
A total of 188 lens wearers completed both study visits; 128 females and 60 males; average age 29 ± 13 (range 18–78 years); 95 test and 93 control participants. After 6 weeks, the overall water exposure score and endotoxin levels reduced significantly in the test group compared with the control group (p < 0.05). There were no significant changes in individual water-contact behaviours or overall storage case contamination.
Conclusion
A no-water infographic on the contact lens case improved overall water-contact behaviours and reduced storage case endotoxin. Refining the messaging may be beneficial in future to improve other aspects of compliance.
Similar content being viewed by others
Introduction
Inappropriate exposure of contact lens and/or storage case to non-sterile water is associated with sterile [1, 2] and infectious corneal disease [3,4,5]. Water exposure including storing and rinsing lenses and cases in tap water [6, 7] and showering or swimming while wearing contact lenses [8] can result in microbial contamination of the contact lens and/or storage case [7, 8]. The most prevalent microbes in lens-related corneal infection are waterborne Gram-negative microorganisms such as Pseudomonas aeruginosa [7, 9, 10] and free-living amoeba including Acanthamoeba [6, 11]. The contact lens and/or storage case may act as a vehicle for transferring pathogenic microorganisms to the eye, potentially increasing the risk of adverse events.
To increase awareness among contact lens wearers regarding risks associated with water exposure, international public health and contact lens-related professional organizations have delivered guidelines to avoid water exposure during contact lens wear [12,13,14,15]. However, handling instructions from contact lens manufacturers endorse the use of tap water for rinsing off cleaning solution from the surface of rigid gas permeable lenses [16, 17]. In addition, water imagery (splashes, pools of water and water droplets) in the marketing materials of contact lens and disinfection products may contribute to confusion about the use of water during contact lens wear amongst both wearers and eye care practitioners. Equivocal messaging may lead to inadvertent water exposure of the contact lens or storage case [16], exposing contact lens wearers to increased risk of adverse events. In an attempt to deliver unequivocal, practical and consistent safety information to contact lens wearers, a “no-water” graphic has been designed by a patient advocate who suffered from Acanthamoeba keratitis [18], to be used on contact lens packaging at the point of supply to contact lens wearers (Fig. 1).
This study aimed to investigate the impact of behavioural education in the form of a simple visual infographic, the “no-water” sticker, on water-contact behaviours of contact lens wearers. A secondary aim was to determine the impact of water education on overall level of overall microbial contamination and endotoxin level in contact lens storage cases.
Materials and methods
Participants
Two hundred established contact lens wearers using reusable soft daily wear reusable contact lenses participated in this randomised, interventional, double masked, 6 weeks clinical trial. Participants were enroled from the UNSW Sydney Optometry Clinic, the UNSW Sydney campus and from the general community. Participants were not included in the study if they were younger than 18 years, used daily disposable lenses or had active anterior segment disease. In addition, participants were excluded if they were enroled in another clinical trial during the study. The study was conducted between June 2017 and December 2018. This study was approved by the UNSW Human Research Ethics Committee (approval ref # HC16735) and all procedures were conducted in accordance with the tenets of the Declarations of Helsinki 1975 as amended in 2000. The clinical trial was registered with the Australian New Zealand Clinical Trial Registry (ACTRN#12618001404213). All subjects signed a statement of informed consent before enrolment.
Study design and intervention protocol
The study included two visits: before and 6 weeks after receiving the interventional education. Participants were randomly allocated into two groups using a blocked randomisation scheme, generated using an online randomisation software, GraphPad™ (San Diego, CA, USA). Block randomisation was used to ensure equal assignment to the two groups. The test group received a “no-water” sticker attached to their storage case and written instructions, while the control group received a storage case without the sticker and the written instructions.
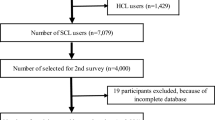
This was a double-blinded trial where both the participants and investigators were masked to group allocation until after completion of data analysis. An unmasked investigator assisted with randomisation and preparation of sealed envelopes marked with the participant enrolment number. The envelope included a new storage case of the same type that the participant was using with or without the “no-water” sticker and the written instructions. The unmasked investigator applied a “no-water” sticker on all storage cases, before microbial analysis (regardless of the group) to maintain masking of the study investigators. Figure 2 explains the participant enrolment and study procedures at the baseline and follow-up visits.
Study procedures
All participants (N = 200) underwent an ocular health and vision assessment and completed a self-administered questionnaire regarding contact lens-related hygiene habits and water exposure during contact lens wear [19, 20]. A total score of 0–8 was calculated (Table 1 in Supplementary Material) to rate compliance on the number of times the contact lens or case was exposed to non-sterile water, with a lower score indicating better compliance.
Microbial analysis of storage cases
The storage cases recovered from subjects were stored at 2–4 °C immediately and microbial analysis was performed within 48 h. The lid of the storage case was removed under aseptic conditions and any residual solution in the storage case was discarded. The right well of the case was used for the ATP assay (Bactiter Glo™, Promega, Sydney, NSW, Australia) for overall microbial contamination as per the manufacturer’s guidelines [21]. Briefly, the biofilm from the case well was removed using a magnetic stirring bar in 1 mL of 1% Luria broth in sterile phosphate-buffered saline (PBS-LB; 10.0 g/L tryptone, 5.0 g/L yeast extract and 5.0 g/L NaCl) (Oxoid Australia, Sydney, NSW, Australia) [22, 23] and 100 µL from this sample was plated in opaque walled 96-well plate (Greiner Bio-one, Radnor, PA, USA) with 100 µL of sterile PBS-LB in the control wells. One hundred microlitres of ATP reagent was added to each well and the plates were placed on an orbital shaker for ~30 s to mix the plate contents [21]. After 5 min of ambient incubation, the luminescence was measured at a wavelength of 410 nm with a spectrophotometer (Fluostar Omega, BMG Labtech, Ortenberg, Germany). A standard curve of the ATP assay was developed using Pseudomonas aeruginosa 6294 (strain widely used during in vitro testing of lens care products), Serratia marcescens ATTC 13880 (strain used in ISO testing) and Staphylococcus aureus 031 (retrieved from storage case of a contact lens wearer with a sterile corneal ulcer) as these three are known storage case contaminants and the strains are implicated in contact lens adverse events [23]. The luminescence values obtained from the ATP assay were converted into Log colony forming units (CFU)/mL from the standard curve based on serially diluted bacteria.
The left well of the storage case was used for the LAL assay to determine endotoxin levels, considered a surrogate for Gram-negative contamination. The LAL assay was performed per the manufacturer’s guidelines (Pyrochrome, Association of Cape Cod, Liverpool, UK). Briefly, biofilm from the case well was removed in 1 mL of LAL reagent water (LRW) and 100 µL of this sample was incubated with 100 µL of lysate for 67 min at 37 °C. The absorbance values of the samples were normalised to a blank of LRW and lysate [24]. The average absorbance values from three repeats for each sample were converted into endotoxin units (EU)/mL.
Safe endotoxin limits for sterile medical devices are considered to be below 0.5 EU/mL [25], however tissue culture-based and in vivo animal-based studies with endotoxin contamination below 2 EU/mL showed minimum or no adverse response [26, 27]. Based on this breakpoint, endotoxin levels were categorized as low (≤2 EU/mL) or high (>2 EU/mL).
Statistical analysis plan
Previous data suggest that 50% of asymptomatic contact lens wearers display water-contact behaviours [17, 22], and based on the expectation that the “no-water” sticker will change water-contact behaviour in half of the participants (odds ratio of 0.5 × (relative precision of 30%)), using 5% level of significance (α = 0.05) and power of 80%, a sample size of 200 wearers were required to detect a change in water-contact behaviour (G*Power, version: 3.1.9.2). Data from only those participants who provided their storage cases and completed both study visits were included in the analysis. The distribution of hygiene habits in both groups at the baseline visit was investigated using descriptive statistics (frequencies and percentages) and Chi-squared interactions to determine any group differences. A one-way analysis of covariance (ANCOVA) was conducted to examine group differences at the 6-week follow-up visit for “water exposure score” and level of contact lens storage case contamination. Logistic regression (with baseline measures as covariates) was used to determine the effect of water education on endotoxin levels and individual water-contact behaviours. Significance was determined at a confidence level of 95% and all variables with p < 0.20 in the univariate analysis were included in the multivariate analysis.
Results
A total of 188 participants successfully completed the study; age, gender and contact lens details are shown in Table 1. There were no significant differences in age, gender, lens replacement schedule and solution type between groups.
The impact of “no-water stickers” on water-contact behaviours
Water-contact behaviours including showering, swimming while wearing lenses, use of wet hands to handle lenses and use of tap water during lens/storage case hygiene were explored individually, as well as combined in the form of an “overall water exposure” score.
At the follow-up visit, the overall water exposure score was significantly lower in the test compared with the control group, when controlling for baseline scores (p = 0.005; one-way ANCOVA) (Table 2).
At the follow-up visit, participants in the control group were more likely to rinse their storage case with tap water compared with the test group, when controlling for this behaviour at the baseline visit (p = 0.043). Using wet hands to handle lenses (p = 0.060) and showering with the lenses (0.083) were slightly but not statistically significantly more common in the control group (Table 3).
Half of the study participants (53%) interpreted the “no-water” sticker as recommending wearers to not to use tap water in the storage case, 35% not to use tap water with contact lenses, 7% not to use tap water with lenses and/or the storage case and only 5% of participants considered the message as “no tap water exposure at all while wearing lenses”. One participant (0.5%) found the message on the sticker unclear.
The impact of “no-water stickers” on storage case contamination
At the baseline visit, 34 (35.8%) participants in the test group and 39 (41.9%) participants in the control group had high endotoxin levels in their storage cases with no group differences (p = 0.387). At the follow-up visit, there was a significant difference in the endotoxin levels between both groups (p = 0.020) with only 20 (21.1%) participants in the test group and 35 (37.6%) participants in the control group having high endotoxin levels in their storage cases (Fig. 3).
At the baseline visit, the average overall microbial contamination was 2.94 ± 1.05 and 3.12 ± 1.01 Log CFU/mL in the test and control group, respectively, and there was no difference between groups (p = 0.227). At the follow-up visit, the average overall microbial contamination was 2.73 ± 1.08 Log CFU/mL in the test and 2.98 ± 0.98 Log CFU/mL in the control group and no significant differences were found in the overall microbial contamination of storage cases (p = 0.173; ANCOVA) (Table 2).
Water exposure score was moderately associated with overall level of microbial contamination at both study visits (rho = 0.234, p = 0.001). In addition, a significantly higher number of participants with water exposure score of ≤1 had low endotoxin levels at both study visits, compared with those who had a water exposure score > 1 (p < 0.001).
Discussion
This study investigated the impact of water education on water-contact behaviours and storage case contamination in contact lens wearers. A key finding of this study was a significant decrease in overall water exposure score, indicating less water exposure with the addition of “no-water” stickers on contact lens wearers’ storage cases. In addition, wearers using the storage cases with the “no-water stickers” had significantly lower levels of endotoxin retrieved from their storage cases compared with those using a storage case without the sticker.
Half of the study participants reported swimming while wearing their lenses without any protective goggles. Showering and using wet hands to handle contact lenses were also identified as common hygiene habits among all participants. These findings are consistent with previous studies that reported water contact is common in the contact lens wearing community [17, 28]. In 2017, a study in USA reported 86% of soft and 67% of RGP lens users wear lenses while showering and 62% of soft and 51% of RGP lens users wear lenses when swimming [17]. Swimming while wearing lenses, specifically without tight-fitting swimming goggles, results in contact lens contamination with waterborne microorganisms [8, 29].
In the current study, the overall water-contact behaviour was improved in those participants using the “no-water” stickers, compared with those using only the written instructions. Hygiene education in the form of written instructions improved contact lens wearers’ compliance to storage case hygiene in a previous study [9], and the impact of visual imagery and its dominance over written communication in terms of recall and awareness is well documented [30, 31]. The findings of the current study are consistent with previous research where the use of visual infographics have shown a positive impact on patients by improving the understanding of disease in patients with asthma [32] and adherence to treatment [32, 33]. Using a graphic message visible each time the lenses are removed may help to reinforce the no-water message in comparison with using the graphic on the lens boxes, visible only once, although this has not been explored previously.
In this study, the participants using the “no-water” stickers on the lens storage case had lower endotoxin levels, which was considered a surrogate for Gram-negative contamination of the storage cases, compared with the controls. However, no significant differences were found in the overall contamination levels. An association has previously been shown between water exposure, where storage cases were rinsed in tap water and Gram-negative storage case contamination [7, 9]. In the current study, the water exposure score was moderately associated with the level of storage case contamination and lower water exposure score was significantly associated with low endotoxin levels at both study visits. The association between Gram-negative bacterial contamination of the storage case and water exposure during contact lens use is important as many contact lens disease-causing pathogens are waterborne Gram-negative bacteria such as Pseudomonas aeruginosa and Serratia marcescens [34, 35]. In addition, tap water exposure during contact lens wear is an established risk factor for contact lens-related Acanthamoeba keratitis [3, 5, 36] and identical strains have been retrieved from storage cases and corneal ulcers of Acanthamoeba keratitis patients [6]. Use of tap water to rinse contact lens storage case can transfer these pathogenic organisms to the case [7], which can act as a vector to transfer the microorganisms to the eye via a contaminated contact lens.
Interestingly, half of the participants linked the message on the “no-water” sticker with storage case hygiene only, indicating the importance of the position and placement of this infographic on contact lens packaging. However, daily disposable lens wearers, who do not require storage cases, are equally at risk of developing contact lens-related adverse events due to water exposure of lenses during showering/swimming or using wet hands to handle lenses [11, 37]. In this case, the placement of “no-water” stickers on lens packaging can be a useful daily reminder for disposable lens wearers. The use of water imagery (splashes, pools of water and water droplets) is widespread in marketing materials and packaging of lenses and is presumably used to denote comfort and moisture. Linking the “no-water” stickers with a website/manual including detailed information can be a useful alternative to better advocate the “absolutely no-water contact with lens/case” approach to all contact lens wearers.
Behavioural modification and healthy habit development is a long-term process and short-term behavioural changes may not be a true representation of actual habits [38]. In the current study, the 6-week timepoint was chosen for follow-up as previous research on modelling healthy habits suggests an average of 2 months time period for healthy habits to form, with changes detectable as early as 18 days [38]. In addition, previous studies have reported improvements in patients’ compliance to recommended guidelines when observed after 1–3 months [9, 32]. However, long-term non/poor adherence to the recommended positive health behaviour changes is widespread [39]. Further research involving longer follow-up visits is needed to understand the long-term impact of water education both in terms of behaviour change and reduction in the incidence of contact lens-related adverse events.
The post hoc power calculation with the final sample size of 188 participants showed 78% power to detect a change in water-contact behaviour (G*Power, 3.0.10). In addition, the post hoc calculation using 5% level of significance (α = 0.05) and power of 80% showed a required sample size of 540 contact lens wearers to detect a change in storage case contamination (G*Power, version: 3.0.10). Future studies with a larger sample size and powered specifically to determine the change in overall storage case contamination may help in exploring the relationship of behavioural education and storage case contamination further.
In conclusion, water education in the form of “no-water” stickers on contact lens storage cases improved the overall water-contact behaviour of contact lens wearers and reduced endotoxin levels in storage cases. However, there were no significant changes in individual behaviours such as using wet hands to handle lenses or showering while wearing lenses, as well as the overall level of storage case contamination. Further research to refine the messaging for “no-water” stickers by including specific signs may help in improving individual water-related behaviours. In addition, it is important to investigate the impact of this visual infographic on the long-term behavioural modifications to understand the effect on contact lens-related adverse events.
Summary
What was known before
-
Water exposure during contact lens wear has been associated with contact lens disease.
-
Despite the documented risks, water exposure is common amongst lens wearers.
What this study adds
-
Water education in the form of a no-water stickers on contact lens storage cases improved the overall water-related hygiene of contact lens wearers and reduced endotoxin levels in storage cases.
References
Richdale K, Lam DY, Wagner H, Zimmerman AB, Kinoshita BT, Chalmers R, et al. Case-control pilot study of soft contact lens wearers with corneal infiltrative events and healthy controls. Investig Ophthalmol Vis Sci. 2016;57:47–55.
Stapleton F, Keay L, Jalbert I, Cole N. The epidemiology of contact lens related infiltrates. Optom Vis Sci. 2007;84:257–72.
Brown AC, Ross J, Jones DB, Collier SA, Ayers TL, Hoekstra RM, et al. Risk factors for Acanthamoeba keratitis—a multistate case-control study, 2008-2011. Eye Contact Lens. 2017;44 Suppl 1:S173–8.
Lam JS, Tan G, Tan DT, Mehta JS. Demographics and behaviour of patients with contact lens-related infectious keratitis in singapore. Ann Acad Med Singap. 2013;42:499–506.
Cope JR, Collier SA, Schein OD, Brown AC, Verani JR, Gallen R, et al. Acanthamoeba keratitis among rigid gas permeable contact lens wearers in the United States, 2005 through 2011. Ophthalmology. 2016;123:1435–41.
Kilvington S, Gray T, Dart J, Morlet N, Beeching JR, Frazer DG, et al. Acanthamoeba keratitis: the role of domestic tap water contamination in the United Kingdom. Investig Ophthalmol Vis Sci. 2004;45:165–9.
Üstüntürk M, Zeybek Z. Microbial contamination of contact lens storage cases and domestic tap water of contact lens wearers. Wien klinische Wochenschr. 2012;124:17–22.
Wu YT, Tran J, Truong M, Harmis N, Zhu H, Stapleton F. Do swimming goggles limit microbial contamination of contact lenses? Optom Vis Sci. 2011;88:456–60.
Tilia D, Lazon de la Jara P, Zhu H, Naduvilath TJ, Holden BA. The effect of compliance on contact lens case contamination. Optom Vis Sci. 2014;91:262–71.
Minogue E, Tuite NL, Smith CJ, Reddington K, Barry T. A rapid culture independent methodology to quantitatively detect and identify common human bacterial pathogens associated with contaminated high purity water. BMC Biotechnol. 2015;15:6.
Hassan F, Bhatti A, Desai R, Barua A. Analysis from a year of increased cases of Acanthamoeba keratitis in a large teaching hospital in the UK. Contact Lens Anterior Eye. 2019. https://doi.org/10.1016/j.clae.2019.04.009.
Vijay AK, Willcox M, Zhu H, Stapleton F. Contact lens storage case hygiene practice and storage case contamination. Eye Contact Lens. 2015;41:91–7.
Department of Health, National Health Services. Contact lens safety—live well—NHS choices. Department of Health, National Health Services. 2016. http://www.nhs.uk/Livewell/Eyehealth/Pages/Contactlenssafety.aspx. Accessed 6 Jul 2018.
Center for Devices and Radiological Health. Contact lenses. Center for Devices and Radiological Health. 2019 https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/HomeHealthandConsumer/ConsumerProducts/ContactLenses/. Accessed 6 Jul 2018.
British Contact Lens Association. Do’s & dont’s factsheet for healthy contact lens care. British Contact Lens Association. 2017. https://bcla.org.uk/Public/Member_Resources/Professional_Resources/Do_s___Dont_s_Factsheet/Public/Member_Resources/Do_s___Dont_s_Factsheet_of_Contact_Lens_Care.aspx?hkey=5eb42bba-bae4-408a-8c2c-330cfa5608fb. Accessed 6 Jul 2018.
Legarreta JE, Nau AC, Dhaliwal DK. Acanthamoeba keratitis associated with tap water use during contact lens cleaning: manufacturer guidelines need to change. Eye Contact Lens. 2013;39:158–61.
Zimmerman AB, Richdale K, Mitchell GL, Kinoshita BT, Lam DY, Wagner H, et al. Water exposure is a common risk behavior among soft and gas-permeable contact lens wearers. Cornea. 2017;36:995–1001.
Carnt N, Stapleton F. Strategies for the prevention of contact lens-related Acanthamoeba keratitis: a review. Ophthalmic Physiol Opt. 2016;36:77–92.
Carnt N, Keay L, Willcox M, Evans V, Stapleton F. Higher risk taking propensity of contact lens wearers is associated with less compliance. Contact Lens Anterior Eye. 2011;34:202–6.
Radford CF, Minassian D, Dart JK, Stapleton F, Verma S. Risk factors for nonulcerative contact lens complications in an ophthalmic accident and emergency department: a case-control study. Ophthalmology. 2009;116:385–92.
Promega. BacTiter-Glo™ microbial cell viability assay. Promega. 2018 https://www.promega.com.au/products/cell-health-assays/cell-viability-and-cytotoxicity-assays/bactiter_glo-microbial-cell-viability-assay/?catNum=G8231. Accessed 18 Jun 2019.
Wu YT, Willcox MD, Stapleton F. The effect of contact lens hygiene behavior on lens case contamination. Optom Vis Sci. 2015;92:167–74.
Wu YT, Zhu H, Willcox M, Stapleton F. Removal of biofilm from contact lens storage cases. Investig Ophthalmol Vis Sci. 2010;51:6329–33.
Noda K, Goto H, Murakami Y, Ahmed ABF, Kuroda A. Endotoxin assay by bioluminescence using mutant firefly luciferase. Anal Biochem. 2010;397:152–5.
US_FDA. Guidance for industry: pyrogen and endotoxins testing: questions and answers | FDA. US_FDA. 2012 https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-industry-pyrogen-and-endotoxins-testing-questions-and-answers#_Toc315937935. Accessed 18 Jun 2019.
Sakimoto A, Sawa M, Oshida T, Sugaya S, Hirono T, Ishimori A. Minimum endotoxin concentration causing inflammation in the anterior segment of rabbit eyes. Jpn J Ophthalmol. 2009;53:425–32.
Cao Y, Bindslev DA, Kjaergaard SK. Estimation of the in vitro eye irritating and inflammatory potential of lipopolysaccharide (LPS) and dust by using reconstituted human corneal epithelium tissue cultures. Toxicol Mech Methods. 2015;25:402–9.
Bowden T, Nosch DS, Harknett T. Contact lens profile: a tale of two countries. Contact Lens Anterior Eye. 2009;32:273–82.
Choo J, Vuu K, Bergenske P, Burnham K, Smythe J, Caroline P. Bacterial populations on silicone hydrogel and hydrogel contact lenses after swimming in a chlorinated pool. Optom Vis Sci. 2005;82:134–7.
De Beni R, Moè A. Imagery and rehearsal as study strategies for written or orally presented passages. Psychonomic Bull Rev. 2003;10:975–80.
Mayeaux EJ Jr, Murphy PW, Arnold C, Davis TC, Jackson RH, Sentell T. Improving patient education for patients with low literacy skills. Am Fam Physician. 1996;53:205–11.
Ebrahimabadi M, Rezaei K, Moini A, Fournier A, Abedi A. Infographics or video; which one is more effective in asthmatic patients’ health? A randomized clinical trial. J Asthma. 2018. https://doi.org/10.1080/02770903.2018.1536143.
Dowse R, Ehlers M. Medicine labels incorporating pictograms: do they influence understanding and adherence? Patient Educ Couns. 2005;58:63–70.
Stapleton F, Keay L, Katiyar S, Edwards K, Naduvilath T. Causative organisms and disease severity in contact lens related microbial keratitis in Australia. Investig Ophthal Vis Sci. 2006;47:4729–4729.
Bourcier T, Thomas F, Borderie V, Chaumeil C, Laroche L. Bacterial keratitis: predisposing factors, clinical and microbiological review of 300 cases. Br J Ophthalmol. 2003;87:834–8.
Carnt NP, Hoffman JM, Verma S, Hau S, Radford CFP, Minassian DC, et al. Acanthamoeba keratitis: confirmation of the UK outbreak and a prospective case-control study identifying contributing risk factors. Br J Ophthalmol. 2018;102:1621–8.
Stapleton F, Naduvilath T, Keay L, Radford C, Dart J, Edwards K, et al. Risk factors and causative organisms in microbial keratitis in daily disposable contact lens wear. PLoS ONE. 2017;12:e0181343.
Lally P, Van Jaarsveld CHM, Potts HWW, Wardle J. How are habits formed: modelling habit formation in the real world. Euro J Soc Psychol. 2010;40:998–1009.
Middleton KR, Anton SD, Perri MG. Long-term adherence to health behavior change. AJLM. 2013;7:395–404.
Acknowledgements
This study was partially funded through an investigator-initiated study supported by Alcon Australia. MA was supported by joint doctoral scholarship from UNSW (tuition fee scholarship) and Higher Education Commission, Pakistan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Arshad, M., Carnt, N., Tan, J. et al. Compliance behaviour change in contact lens wearers: a randomised controlled trial. Eye 35, 988–995 (2021). https://doi.org/10.1038/s41433-020-1015-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-1015-9