Abstract
Background
To compare the outcomes of half-dose verteporfin photodynamic therapy (vPDT) for central serous chorioretinopathy (CSCR) with or without subfoveal fibrin.
Methods
One hundred seventy-three cases of CSCR treated with half-dose vPDT between September 2008 and February 2018 were retrospectively reviewed and classified into two groups: CSCR with subfoveal fibrin (fibrin group) and without subfoveal fibrin (no-fibrin group). The changes in best-corrected visual acuity (BCVA) from baseline and in central macular thickness (CMT) were recorded at 1, 3, and 6 months after the treatment.
Results
Forty-eight eyes were included in the fibrin group and 125 eyes in the no fibrin group. There were no statistical differences in the baseline characteristics including age, gender, duration of symptoms, and CMT between the groups. The baseline mean BCVA of the fibrin group was significantly worse than that of the no fibrin group (0.47 ± 0.32 versus 0.32 ± 0.31 in logMAR; p = 0.003). There was no statistically significant difference between the two groups in the improvement of BCVA at each follow-up point (1 month: p = 0.069; 3 months: p = 0.111; 6 months: p = 0.172, respectively) and in the reduction of CMT (1 month: p = 0.367; 3 months: p = 0.767; 6 months: p = 0.496, respectively). In the fibrin group, the rates of complete resolution of the subretinal fibrin at 1, 3, and 6 months after vPDT were 72.9%, 95.8%, 95.8%, respectively. The SRF resolution rate at 1, 3, and 6 months was 72.9%, 89.6% and 91.7% respectively in the fibrin group and was 62.4%, 83.2% and 84.0% in the no fibrin group. There was no significant difference of SRF resolution rate between the two groups at 1 month (p = 0.216), 3 months (p = 0.350), and 6 months (p = 0.228). No ocular adverse event was encountered in both groups.
Conclusion
Half-dose vPDT was effective and safe for CSCR patients with subfoveal fibrin.
Similar content being viewed by others
Introduction
Central serous chorioretinopathy (CSCR) is characterized by serous detachment of the neurosensory retina with or without detachment of retinal pigment epithelium (RPE). It is more frequent among healthy young men with type A personalities [1]. Usually the subretinal fluid (SRF) is transparent, allowing clear visualization of the underlying RPE and choroidal details, but sometimes it may become cloudy and greyish. This greyish-white subretinal exudate has been demonstrated to be located closely to the leakage point on fundus fluorescein angiography (FFA) [2, 3]. Optical coherence tomography (OCT) scan through the greyish-white subretinal exudate present with high reflectance material between the detached neurosensory retina and underlying RPE. A RPE detachment (PED) can often be found adjacent to the exudate [4, 5]. Histopathologic studies have demonstrated that the greyish-white exudate seen ophthalmoscopically is actually fibrin [6]. Fibrin is believed to leak into the subretinal space through RPE micro-rip [2] and has been documented in up to 61% of cases in Asian population [4, 7, 8].
Although it has been reported that half-dose verteporfin photodynamic therapy (PDT) is an effective and safe treatment option for both acute and chronic CSCR [9,10,11], to the best of our knowledge, there are currently limited clinical data on the application of this therapy for patients with fibrinous exudation, especially for patients with subfoveal fibrin. Yannuzzi suggested that more attention should be paid when treating leaks near the fovea when there is accompanied by fibrin because fibrin is capable of forming bioconjugates with verteporfin and may potentially stimulate subretinal fibrosis and fibrotic scar formation, leading to permanent visual loss [12]. The safety of half-dose verteporfin PDT (vPDT) in which the light is delivered to the subfoveal fibrin site in CSCR remains insufficiently evidenced. The purpose of this study is to compare the outcomes of half-dose vPDT for CSCR with or without subfoveal fibrin.
Methods
A consecutive series of patients diagnosed with CSCR and treated with half-dose vPDT (by the same doctor ZMW) in ophthalmology department of Peking University People’s Hospital from September 2008 to February 2018 were retrospectively reviewed. This study followed the guidelines of the Declaration of Helsinki and was approved by the Investigational Review Board of the Peking University People’s Hospital.
The patients were enrolled in the study when the following baseline criteria were fulfilled: (1) the presence of SRF involving the foveal center on OCT; (2) age between 18 and 55 years; (3) the presence of dilated choroidal vessels and choroidal hyperpermeability in the macula on indocyanine green angiography (ICGA); (4) more than 6 months follow-up with available best-corrected visual acuity (BCVA) and OCT images at 1, 3, and 6 months after vPDT. The exclusion criteria were as follows: (1) previous PDT or laser photocoagulation or anti-vascular endothelial growth factor injections to treat CSCR; (2) choroidal neovascularization, drusen, polypoidal choroidal vasculopathy or other maculopathy; (3) any retinal vascular disease or choroidal disease; (4) previous use of steroid systemically or topically at baseline.
All eyes underwent half-dose PDT with verteporfin (Visudyne, Novartis AG, Bulach, Switzerland) within 2 days after diagnosis of CSCR. Three mg/m2 of verteporfin was infused for 10 min, followed by delivery of laser energy at 689 nm at 15 min from the start of infusion. A total light energy of 50 J/cm2 was delivered for 83 s covering the hyperfluorescent area observed in the mid-phase of ICGA. Areas of choroidal hyperpermeability were measured and treated separately. After treatment, the patients were instructed to avoid strong light for 48 h.
Baseline characteristics including age, gender, duration of symptoms, BCVA, and central macular thickness (CMT) were collected. BCVA and CMT at 1, 3, and 6 months after vPDT were recorded. OCT images at baseline and each follow-up visit were reviewed by two retinal specialists (MZ and JQ). All eyes were divided into two groups based on whether subfoveal fibrin was present or absent on baseline OCT images. Eyes with subfoveal fibrin were defined as those with high reflectance material between the detached neurosensory retina and underlying RPE in the 1 mm central subfield. BCVA was changed to logarithm of the minimal angle of resolution (LogMAR) score from Snellen acuity. The CMT were defined as the distance between the inner surface of the choroid and the inner limiting membrane at the fovea centre. Ocular and nonocular adverse events were also collected from medical record and analysed.
Statistical analyses were performed on the full analysis set and all missing values of efficacy analysis were inputted using the last-observation-carried-forward method. Comparisons of baseline demographics and clinical data were made between the two groups using the two-tailed t-test and Wilcoxon signed-rank test for continuous variables and using the Pearson Chi-square test/Fisher’s exact test for binary variables. Pearson Chi-square test was applied to compare the SRF resolution rate at each follow-up visit between the two groups. All statistical analyses were performed using the Statistical Packages for the Social Sciences (SPSS, version 24, Chicago, IL, USA). P values less than 0.05 were considered statistically significant.
Results
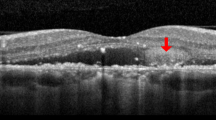
One hundred seventy-three eyes of 153 patients were enrolled in this study, 48 eyes were divided into the fibrin group (Fig. 1a) and 125 eyes were recruited into the no fibrin group (Fig. 1b).
a OCT raster scans of a 34-year-old male patient with BCVA of 0.3 logMAR; the subfoveal fibrin present as high reflectance material between the detached neurosensory retina and underlying RPE b OCT raster scans of a 47-year-old female patient with BCVA of 0.1 logMAR; there was no high reflectance material between the detached neurosensory retina and underlying RPE.
The baseline characteristics of the patients are listed in Table 1. The mean age of the patients was 44.6 ± 8.5. One hundred and twenty-eight patients were male and 45 were female. The mean logMAR BCVA before PDT was 0.36 ± 0.32 (Snellen equivalent 20/46). The mean CMT before PDT was 347.8 ± 165.3 μm. No statistical differences were identified between the two groups on age, gender, mean duration of symptoms, and CMT. The mean BCVA of the fibrin group was significantly worse than that of the no fibrin group (p = 0.003) (Table 1). In the fibrin group, nine eyes (18.8%) showed a “string-like” pattern bridging the posterior surface of the sensory retina and the RPE above the leakage site, which seemed to arise from the swelling of the outer nuclear layer (ONL) and thickening of photoreceptor of outer segment (POS) (Fig. 2a). Ten eyes (20.8%) showed hyperreflective fibrin surrounding a hyporeflective lucency on OCT (Fig. 2b). RPE abnormalities were demonstrated in 42 of 48 eyes (87.5%) in the fibrin group and 105 of 125 eyes (84.0%) in the no fibrin group (p = 0.642).
a “String-like” pattern bridging the posterior surface of the sensory retina and RPE (arrow). A-line scan from a 40-year-old male patient with BCVA in logMAR of 0.2; dipping of the posterior layer of the neurosensory retina were noted. b The RPE and hyperreflective fibrin surrounding a hyporeflective lucency in central serous chorioretinopathy (arrow head). A-line scan from a 34-year-old male patient with BCVA in logMAR of 0.3; a central hyporeflective lucency of the subretinal fibrin were found.
The average follow-up period after vPDT was 21.9 ± 22.9 months (6–110 months). Serial changes of BCVA and CMT at each follow-up visit in the two groups are presented in Fig. 3a and Fig. 3b, respectively. Both groups showed significant improvements in BCVA (p < 0.01) and CMT (p < 0.01) compared with the baseline up until the last follow-up visit (p < 0.01). There was no statistically significant difference between the two groups for the improvements of BCVA at each follow-up visit (1 month: p = 0.069; 3 months: p = 0.111; 6 months: p = 0.172; Fig. 3a) and reduction of CMT (1 month: p = 0.367; 3 months: p = 0.767; 6 months: p = 0.496; Fig. 3b).
a Serial changes of BCVA from baseline at each follow-up visit in the two groups. There was no significant difference between the two groups for improvement in BCVA at each follow-up visit (1 month: p = 0.069; 3 months: p = 0.111; 6 months: p = 0.172, respectively). b Serial changes of CMT from baseline at each follow-up visit in the two groups. There was no significant difference between the two groups for reduction of CMT at each follow-up visit (1 month: p = 0.367; 3 months: p = 0.767; 6 months: p = 0.496, respectively).
In the fibrin group, the rates of complete resolution of the subretinal fibrin at 1, 3, and 6 months after vPDT were 72.9%, 95.8%, 95.8%, respectively. The SRF was completely absorbed in 72.9%, 89.6% and 91.7% of eyes at 1, 3, and 6 months, respectively. A representative case is shown in Fig. 4. The fibrin always resolved prior to the decrease in SRF. SRF was not completely resolved in 13, 5, and 4 patients at 1, 3, and 6 months, respectively. At 1 month, only 5 patients were left with subtle fibrin exudate. At 3 months and 6 months, only 2 patients were left with subtle fibrin exudate. In the no fibrin group, the SRF was completely absorbed in 62.4% of eyes at 1 month, 83.2% at 3 months and 84.0% at 6 months. There was no significant difference of complete SRF resolution rate at 1 month (p = 0.216), 3 months, (p = 0.350) and 6 months (p = 0.228).
A 48-year-old woman with blurred vision for 3 months in the left eye. Her BCVA was 0.8 logMAR (20/126) at baseline. a A color fundus photograph and OCT showed subfoveal fibrin located between the detached neurosensory retina and irregular RPE. b. FA and ICGA images demonstrated choroidal hyperpermeability and dilated choroidal vessels. PDT was delivered for covering the hyperfluorescent area observed in the mid-phase of ICGA (yellow circle). c–e One month, 3 months, and 6 months after half-dose vPDT. Both the subretinal fluid and fibrin resolved at 1 month visit. Her visual acuity improved to 0.3 logMAR (20/40). Ellipsoid zone band irregularity was shown at 1 month visit but restored at 3 and 6 months’ visit.
In the fibrin group, four eyes (8.3%) suffered recurrence and three of them underwent a second half-dose vPDT. All of them showed completed resolution of SRF after the second PDT within 1 month. A representative case is shown in Fig. 4. In the no fibrin group, 11 eyes (8.8%) had recurrence and 4 of them underwent a second half-dose vPDT. Two of them showed completed resolution after the second PDT within 1 month, but the other two had persistent SRF during the whole follow-up period. There was no significant difference in the recurrence rate within 6 months between the two groups (p = 1.000). No ocular adverse event was encountered in both groups.
Discussion
CSCR accompanied by subretinal fibrin was firstly reported by Gass [13]. Histopathological analysis showed that the greyish-white exudate seen ophthalmoscopically is fibrin [6, 14]. Subfoveal fibrin accumulation in CSCR is a visually impairing manifestation and it may increase the risk of formation of fibrotic scars, vascularization of the fibrosis, and the formation of an RPE rip without proper treatment [15, 16].
With the advent of OCT technology, Shinojima et al. demonstrated that the fibrin were observed both within the subretinal space and beneath the RPE in 6 of 21 CSCR patients using spectral domain-OCT (SD-OCT) and confocal scanning laser ophthalmoscopy [17]. Ten eyes with CSCR were analysed with OCT and FFA by Hussain et al. and found six eyes (60%) showed subretinal fibrin over the leakage site and all these eyes had ink-blot leak [18]. These studies provide the evidence that the fibrinogen, the monomeric precursor of fibrin, may be emanated from the choriocapillaris and form fibrin beneath the RPE and gain access into the subretinal space through tiny RPE defects. In our study, RPE defects were found in 42 eyes (87.5%) in the fibrin group. Kim et al. and Fujimoto et al. found that miniscule RPE defects within a PED corresponding to the exact location of a leakage site on FA [4, 8]. This probably meant the presence of fibrin is an important sign of disease activity as the fibrin is corresponding to the leakage site and RPE abnormalities, which partially gave evidence to Yu’s hypothesis that CSCR with subretinal fibrin may be an early indicator of CSCR. In our study, hyporeflective lucency within subfoveal hyperreflective fibrin was observed in ten eyes (20.8%) on OCT. Saito et al. firstly reported the similar finding of a central lucency surrounded by hyperreflective contents using time domain-OCT (TD-OCT). They hypothesized that the exudative fluid from the choroid spring out into the subretinal space from the micro-defect of the RPE [2]. Yannuzzi et al. suggested that a central hyporeflective lucency within surrounding fibrin may be a sign of active leak by using en face OCT [5].
In this study, nine eyes (18.8%) showed a “string-like” pattern bridging the posterior surface of the sensory retina and the RPE above the leakage site. In all of these eyes, the ONL and the POS were thickened. The similar results were reported by previous studies [4, 8, 19, 20]. But as for the mechanism of this pattern, different authors hold different opinions. Yu et al. believes that the subretinal fibrin may act as a “glue” between the RPE and the neurosensory retina and then retinal sagging develops [19]. In the other hand, Besada et al. hypothesized that this sign may arise from the hydrostatic pressure of the exudative fluid that springing out from the choriocapillaris indenting and folding the outer retinal layer [21]. The swollen POS was not the consequent of the subretinal fibrin but a factor facilitating this pattern. In our study, the visual acuity of the fibrin group was significantly worse than that of the no fibrin group at baseline. We suggest that the structural defects in the outer retinal layer associated with the fibrinous exudate may explain why the visual acuity was worse when fibrin was accumulated at the subfoveal space.
The treatment for subfoveal fibrin has not been well studied. The spontaneous resolution of the subretinal fibrin in the CSCR cases has been previously reported [16, 18]. Ie et al. evaluated 11 CSCR patients accompanied by subretinal exudative fibrin. The exudate gradually dissolved without any treatment [18]. Rezai et al. reported a pregnancy-induced CSCR patients accompanied by subfoveal fibrin. Two weeks after delivery without treatment, OCT showed resolution of SRF and the disappearance of subfoveal fibrin [16]. However, Schatz et al. reviewed ten CSCR eyes with subretinal fibrin. All eyes were followed up without any intervention. Subretinal fibrin led to subretinal fibrosis in seven of the ten eyes. After the formation of fibrotic scars, vascularization of the fibrosis, and the formation of an RPE rip, the visual acuity of the eyes decreased to different extent. The authors suggested that the RPE cells beneath the subretinal fibrin tended to lose their normal, epithelial, morphologic features and “pump” functions, which can lead to severe visual loss [15].
In the past, thermal laser photocoagulation has been used for CSCR with subretinal fibrin [2, 15, 18]. Saito et al. [2] reported that after using laser photocoagulation at the leakage point in nine CSCR eyes with subretinal fibrin, SRF and fibrin were absorbed in all eyes during the follow-up period. Schatz et al. [15] reported three eyes with subretinal fibrin treated with laser photocoagulation exhibited fibrotic scarring. It is noteworthy that the locations of the fibrin in their studies were outside the central subfield. Symeonidis et al. reported a case of CSCR complicated by subretinal fibrin accumulation [22]. After intravitreal injections of ranibizumab, the subretinal fibrin was dissolved and the SRF was completely absorbed. However, no further experimental studies investigating the potential anti-vascular endothelial growth factor effect on subretinal fibrin. Although vPDT is considered to be an effective and safe therapy for CSCR [10], the use of half-dose vPDT for CSCR with subfoveal fibrin has not been well studied. Yannuzzi proposed that theoretically, exaggerated PDT responses in the macula may be related to an excessive amount of fibrin in the subretinal space at the treatment site [12]. It is still controversial to use half-dose vPDT to treat CSCR with subfoveal fibrin. In our study, all eyes underwent half-dose vPDT and the results showed that there was no statistically significant difference in the improvement of BCVA at 1, 3, and 6 months after vPDT between the group with or without subfoveal fibrin. And there was no significant difference of complete SRF resolution rate between the two groups at 1, 3, and 6 months after vPDT. These demonstrate that half-dose vPDT is effective and safe for the CSCR with subfoveal fibrin, as well as those without subfoveal fibrin. Fujimoto et al. found fibrin will remain in the subretinal space for a while after the neurosensory retina reattached [8]. In contrast, in our study, the fibrin always resolved prior to the decrease in SRF. The rapid response to PDT may suggest that this method may be an effective treatment option in the management of the CSCR complicated by subretinal fibrin accumulation.
Our study had certain limitations. First, we did not quantify the amount of fibrin. Furthermore, this study had a short follow-up period, which is an innate limitation of retrospective studies. A prospective randomized control study with long-term follow-up is needed to further investigate the advantages of half-dose vPDT for CSCR with subfoveal fibrin.
In conclusion, this study has demonstrated that half-dose vPDT is an effective and safe treatment for CSCR patients with subfoveal fibrin.
Summary
What was known before
-
Although it has been reported that half-dose verteporfin photodynamic therapy (PDT) is an effective and safe treatment option for both acute and chronic CSCR. Yannuzzi suggested that more attention should be paid when treating leaks near the fovea when there is accompanied by fibrin because fibrin is capable of forming bioconjugates with verteporfin and may potentially stimulate subretinal fibrosis and fibrotic scar formation, leading to permanent visual loss.
What this study adds
-
Half-dose vPDT was effective and safe for CSCR patients with subfoveal fibrin.
References
Gass JD. Pathogenesis of disciform detachment of the neuroepithelium. Am J Ophthalmol. 1967;63:1–139.
Saito M, Iida T, Kishi S. Ring-shaped subretinal fibrinous exudate in central serous chorioretinopathy. Jpn J Ophthalmol. 2005;49:516–9.
Iida T, Hagimura N, Sato T, Kishi S. Evaluation of central serous chorioretinopathy with optical coherence tomography. Am J Ophthalmol. 2000;129:16–20.
Kim HC, Cho WB, Chung H. Morphologic changes in acute central serous chorioretinopathy using spectral domain optical coherence tomography. Korean J Ophthalmol. 2012;26:347–54.
Yannuzzi NA, Mrejen S, Capuano V, Bhavsar KV, Querques G, Freund KB. A central hyporeflective subretinal lucency correlates with a region of focal leakage on fluorescein angiography in eyes with central serous chorioretinopathy. ophthalmic surg lasers imaging. Retina. 2015;46:832–6.
Venecia DG. Fluorescein angiographic smoke stack: case presentation at Verhoeff society Meeting, Washington, DC; April 24–25, 1982.
Nair U, Ganekal S, Soman M, Nair K. Correlation of spectral domain optical coherence tomography findings in acute central serous chorioretinopathy with visual acuity. Clin Ophthalmol. 2012;6:1949–54.
Fujimoto H, Gomi F, Wakabayashi T, Sawa M, Tsujikawa M, Tano Y. Morphologic changes in acute central serous chorioretinopathy evaluated by fourier-domain optical coherence tomography. Ophthalmology. 2008;115:1494–500.
Naseripour M, Falavarjani KG, Sedaghat A, Moghaddam AK, Nasserisina S, Alemzadeh SA. Half-dose photodynamic therapy for chronic central serous chorioretinopathy. J Ophthalmic Vis Res. 2016;11:66–9.
Tseng CC, Chen SN. Long-term efficacy of half-dose photodynamic therapy on chronic central serous chorioretinopathy. Br J Ophthalmol. 2015;99:1070–7.
Zhao M, Zhang F, Chen Y, Dai H, Qu J, Dong C, et al. A 50% vs 30% dose of verteporfin (photodynamic therapy) for acute central serous chorioretinopathy: one-year results of a randomized clinical trial. JAMA Ophthalmol. 2015;133:333–40.
Yannuzzi LA. Central serous chorioretinopathy: a personal perspective. Am J Ophthalmol. 2010;149:361–3.
Gass J Stereoscopic atlas of macular diseases: diagnosis and treatment, 4th ed. St Louis, MO: CV Mosby; 1987:56–7.
Ikui H. Histologic examination of central serous retinopathy. Nippon Ganka Kiyo. 1969;20:1035–41.
Schatz H, McDonald HR, Johnson RN, Chan CK, Irvine AR, Berger AR, et al. Subretinal fibrosis in central serous chorioretinopathy. Ophthalmology. 1995;102:1077–88.
Rezai KA, Eliott D. Optical coherence tomographic findings in pregnancy-associated central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol. 2004;242:1014–6.
Shinojima A, Hirose T, Mori R, Kawamura A, Yuzawa M. Morphologic findings in acute central serous chorioretinopathy using spectral domain-optical coherence tomography with simultaneous angiography. Retina. 2010;30:193–202.
Hussain N, Baskar A, Ram LM, Das T. Optical coherence tomographic pattern of fluorescein angiographic leakage site in acute central serous chorioretinopathy. Clin Exp Ophthalmol. 2006;34:137–40.
Yu J, Jiang C, Xu G. Study of subretinal exudation and consequent changes in acute central serous chorioretinopathy by optical coherence tomography. Am J Ophthalmol. 2014;158:752–6.e752.
Ie D, Yannuzzi LA, Spaide RF, Rabb MF, Blair NP, Daily MJ. Subretinal exudative deposits in central serous chorioretinopathy. Br J Ophthalmol. 1993;77:349–53.
Besada E, Frauens BJ, Makhlouf R, Shechtman D. Comparative tomography of central serous 2 chorioretinopathy. New Front Ophthalmol. 2016;2:43–51.
Symeonidis C, Kaprinis K, Manthos K, Androudi S, Anastassilakis K, Dimitrakos SA. Central serous chorioretinopathy with subretinal deposition of fibrin-like material and its prompt response to ranibizumab injections. Case Rep Ophthalmol. 2011;2:59–64.
Funding
This work was supported by the National Natural Science Foundation of China Grant (81770943, 81470651); National key research and development program (2016YFC0904801, 2017YFC0111204); the Research Fund for Science and Technology Program of Beijing (Nos. Z171100002217081, Z161100000516037); Peking University People’s Hospital Scientific Research Development Funds (RDY2017-31). The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liang, Z., Qu, J., Huang, L. et al. Comparison of the outcomes of photodynamic therapy for central serous chorioretinopathy with or without subfoveal fibrin. Eye 35, 418–424 (2021). https://doi.org/10.1038/s41433-020-0858-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0858-4
This article is cited by
-
Chronic Central Serous Chorioretinopathy in Elderly Subjects: Structure and Blood Flow Characteristics of Retina and Choroid
Ophthalmology and Therapy (2024)
-
Risk factors of persistent subretinal fluid after half-dose photodynamic therapy for treatment-naïve central serous chorioretinopathy
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)