Abstract
Background
A variety of treatment strategies have been proposed for macular holes that persist or recur after surgery, and the debate about the best re-treatment approach is ongoing. To allow for a comparison with alternative surgical therapies, we assessed the anatomical and functional outcome of a temporary tamponade with conventional silicone oil in persistent or recurrent full-thickness macular holes.
Methods
We retrospectively investigated consecutive patients with full-thickness macular holes that persisted or recurred following vitrectomy with internal limiting membrane peeling and gas tamponade. All patients received re-treatment by temporary tamponade of silicone oil and were allowed free postoperative positioning. Anatomical closure rate was assessed by optical coherence tomography, and change of best-corrected visual acuity (BCVA) was analyzed.
Results
A total of 33 eyes of 33 consecutive patients were included. Macular hole closure following silicone oil tamponade was achieved in 30 of 33 eyes (90.9%). Median BCVA improved from 1.00 logMAR (interquartile range, 0.60–1.00) to 0.65 logMAR (0.49–1.00; p = 0.010) after silicone oil removal. In patients with macular hole closure, 61.3% exhibited functional improvement with median BCVA changing from 1.00 logMAR (0.70–1.00) to 0.60 logMAR (0.49–1.00; p = 0.0005). Mean minimal linear diameter of macular holes before primary surgery was 391.0 µm (±137.8; range 133–630), and 48.5% of macular holes were >400 µm in diameter.
Conclusions
Treatment of persistent or recurrent full-thickness macular holes by temporary conventional silicone oil tamponade without postoperative positioning results in a high closure rate and a significant mean improvement of visual acuity.
Similar content being viewed by others
Introduction
A variety of treatment strategies have been proposed for macular holes that persist or recur following pars plana vitrectomy (PPV) with internal limiting membrane (ILM) peeling and gas tamponade. Surgical approaches include renewal of the gas tamponade, introduction of platelet concentrate or whole blood into the hole, use of ILM, lens capsule, retinal tissue, or amniotic membrane to cover or fill the hole, induction of temporary macular detachment to mobilize the hole edges, or combinations of the above. The debate about the best treatment approach is ongoing.
Studies report the closure of persistent macular holes by renewal of the intravitreal gas tamponade and postoperative prone positioning of the patient in 61% (17 of 28 eyes) [1] and 62% (22 of 36 eyes) [2] of treated eyes. Addition of autologous platelet concentrate injection to gas tamponade renewal resulted in closure rates of 57% (8 of 13 eyes) [3], 60% (62 of 103 eyes) [4], 78% (21 of 27 eyes) [5], and 85% (52 of 61 eyes) [6] in different studies.
In primary macular hole surgery, temporary tamponade using silicone oil results in macular hole closure rates of 86–92% [7, 8] but gas remains the tamponade of choice for initial surgery due to its similarly high efficacy and the lack of need for subsequent oil removal surgery. In persistent macular holes, however, secondary installation of a temporary silicone oil tamponade represents a possible treatment approach in selected cases, such as patients that are unable to comply with postoperative positioning.
Heavy silicone oil tamponade has been suggested to be superior to conventional silicone oil in persistent macular hole closure due to its presumed improved contact with the posterior retina [3, 9,10,11]. Reported closure rates by heavy silicone oil tamponade in persistent macular holes range between 46% (16 of 35 eyes) [3], 82% (9 of 11 eyes) [9], 87% (20 of 23 eyes) [11], and 92% (11 of 12 eyes) [10].
Compared to heavy silicone oil, conventional (light) silicone oil requires less extensive surgery to remove and may thus have a lower risk of complications. Furthermore, conventional silicone oil is more readily available and cheaper. Case series’ report closure of macular holes by conventional silicone oil in 2 of 2 eyes [12], 5 of 5 eyes [8], and 62% (9 of 13 eyes) [13]. However, unlike heavy silicone oil, published data on the effectiveness of conventional silicone oil is limited. To facilitate an evidence-based comparison with results of alternative treatment approaches as reported by other studies, we retrospectively assessed the closure rate of persistent or recurrent macular holes following conventional silicone oil tamponade without postoperative positioning in a cohort of 33 consecutive patients.
Materials and methods
We retrospectively reviewed consecutive patients who were diagnosed with persistent or recurrent full-thickness macular hole following PPV with ILM peeling and gas tamponade at the Department of Ophthalmology, University of Bonn, Germany, between January 1, 2011, and December 31, 2019 and who were treated by temporary silicone oil tamponade. Each surgery was performed by one of three experienced retinal surgeons of our department. We excluded patients with traumatic macular hole (n = 1), myopic macular degeneration (n = 4; range of myopia, −12 to −29 dpt), prior retinal detachment (n = 1) and loss to follow-up after silicone oil removal (n = 5).
All patients underwent optical coherence tomography (OCT) examinations (Spectralis HRA + OCT; Heidelberg Engineering, Heidelberg, Germany) at our department before initial PPV (baseline), before re-PPV with silicone oil installation, and before silicone oil removal surgery. To measure macular hole size, the OCT B-scan showing the largest extent of the macular hole was chosen from the macular volume scan, and the minimum horizontal linear diameter of the macular hole was quantified using OCT software (HEYEX Version 2.4.1; Heidelberg Engineering, Heidelberg, Germany). Identical B-scans were used for follow-up measurements whenever available.
Final study examination following silicone oil removal was performed either at our department or by the referring ophthalmologist. Patients with a follow-up time after silicone oil removal of less than 4 weeks were excluded.
Best-corrected visual acuity (BCVA) was measured by autorefractometry at each patient visit. BCVA values were converted into logarithm of the minimum angle of resolution (logMAR) for statistical analysis. Due to their presumed non-Gaussian distribution, logMAR BCVA values are expressed as median with interquartile range throughout the manuscript whereas all other study parameters are expressed as mean with standard deviation. Statistical comparison of baseline and final BCVA was performed using Wilcoxon matched-pairs signed-rank test (Prism 8, GraphPad, San Diego, USA), and differences with a two-tailed p value of 0.05 of less were considered statistically significant.
Results
We included 33 eyes of 33 consecutive patients with persistent (n = 31) or recurrent (n = 2) full-thickness macular holes following macular hole surgery with ILM peeling and gas tamponade (Table 1). Mean patient age at initial macular hole surgery was 70.0 years (±7.4; range 49.6–87.6). Patient sex was female in 72.7% (24/33 patients) and male in 27.3% (9/33 patients). Accompanying VMT was present before primary surgery in 15.2% of eyes (5/33 eyes). In the 2 eyes with recurrent macular holes, hole closure was confirmed by OCT following ILM peeling and gas tamponade but re-opening of the hole occurred after 7 months and 2.5 years, respectively.
Mean interval between first examination at our department and initial macular hole surgery was 1.8 weeks (±1.3; range 0.1–3.9). During initial surgery, all patients received macular ILM peeling assisted by ILM staining using Brilliant Blue G. As gas tamponade, C3F8 was employed in 90.9 % (30/33 eyes) and C2F6 in 9.1% (3/33 eyes). Mean interval between initial surgery and silicone oil installation was 8.7 weeks (±5.2; range 1.9–28.9) for persistent macular holes (n = 31). For the 2 eyes with recurrent macular holes, this interval was 28.3 and 131.1 weeks, respectively. In all patients, sufficient removal of the central ILM could be achieved during initial surgery and, thus, no additional ILM peeling was required during silicone oil installation. In 90.9% of eyes (30/33 eyes), PPV was 23-gauge with 2000 cSt silicone oil whereas 20-gauge PPV with 5000 cSt silicone oil was employed in 9.1% (3/33 eyes). No postoperative patient positioning was advised following silicone oil installation. Mean duration of silicone oil tamponade was 17.1 weeks (±14.1; range 6.0–78.0; median 12.1). While we usually aimed for a duration of silicone oil tamponade of 12 weeks, duration was significantly longer in some patients due to missed follow-up appointments or patient’s request.
Minimum follow-up time after silicone oil removal was 4 weeks. Patients who were reviewed in our department (n = 26) had their last study examination a mean of 7.4 weeks (±3.3; range 4.3–17.0) following silicone oil removal. In patients that were followed-up by the referring ophthalmologist (n = 7), the first examination was recommended immediately following hospital discharge and the last examination included in the study was performed a mean of 229.5 weeks (±181.0; range 7.0–457.4) after silicone oil removal.
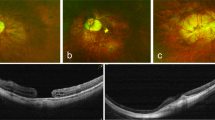
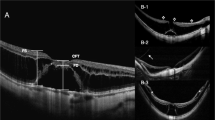
Closure of the macular hole following silicone oil tamponade was achieved in 90.9% of all study eyes (30/33 eyes; Fig. 1A–D), whereas the macular hole persisted in 9.1% of eyes (3/33 eyes; Fig. 1E–H). Subgroup analysis demonstrated hole closure in 90.3% of eyes with macular holes that persisted following primary surgery (28/31 eyes) and in 2 of 2 eyes with macular holes that recurred after previous closure following primary surgery. In one of the 31 eyes with successful macular hole closure after silicone oil tamponade, a macular hole recurred after 4 years.
OCT examinations were performed in a study patient with closed macular hole following silicone oil tamponade (A–D) and a study patient with persistent macular hole (E–H). Examinations were performed before ILM peeling and gas tamponade (A, E), after ILM peeling and gas tamponade (B, F), during silicone oil tamponade (C, G), and after silicone oil removal (D, H).
Median BCVA for all patients was 1.00 logMAR (0.60–1.00) at baseline and improved significantly to 0.65 logMAR (0.49–1.00; p = 0.010) at final study examination (Table 2). Likewise, in the subgroup of closed macular holes (n = 30), median BCVA improved significantly from 1.00 logMAR (0.70–1.00) at baseline to 0.60 logMAR (0.49–1.00; p = 0.0005) at final study examination. In eyes with closed macular holes, 61.3% (19/30 eyes) exhibited an improvement of BCVA, compared to 0% (0/3 eyes) with persistent macular holes (Fig. 2).
In 57.6% of eyes (19/33 eyes), cataract surgery was performed in combination with one of the three macular hole surgeries during the study period whereas 12.1% (4/33 eyes) remained phakic and 30.3% (10/33 eyes) were pseudophakic already at baseline. In the subgroup of eyes that were already pseudophakic at baseline (n = 10), median BCVA improved from 0.94 logMAR (0.66–1.23) at baseline to 0.60 logMAR (0.54–0.84; p = 0.031) at final study examination.
Morphological analysis of macular holes by OCT revealed a mean minimum linear diameter of 391.0 µm (±137.8; range 133–630; Table 2) at baseline. According to International Vitreomacular Traction Study Group (IVTS) classification [14], macular hole size was small (≤250 µm) in 18.2% (6/33 eyes), medium (251–400 µm) in 33.3% (11/33 eyes), and large (>400 µm) in 48.5% (16/33 eyes). At baseline, 93.9% (31/33 eyes) of macular holes exhibited a surrounding subretinal fluid cuff (Fig. 1A, E) whereas 6.1% (2/33 eyes) had a flat configuration without fluid cuff. Polycystoid changes of the macular hole rim were present in 87.9% (29/33 eyes; Fig. 1A, E) at baseline.
Of the three macular holes that did not close, one was small, one medium, and one large according to IVTS classification. All three had a subretinal fluid cuff and rim cystoid changes at baseline (Fig. 1E). In these three eyes, silicone oil tamponade was installed 2.0, 11.0, and 16.0 weeks after the first vitrectomy, respectively. All three holes exhibited a flat open configuration during silicone oil tamponade (Fig. 1G). Duration of silicone oil tamponade in these three eyes was 10.6, 33.9, and 43.7 weeks, respectively. Following silicone oil removal, all three eyes lacked signs of an epiretinal membrane causing traction on the hole or other obvious changes in OCT or fundoscopy that would explain why they did not close (Fig. 1F).
No treatment complications were observed in our cohort, and the silicone oil tamponade was well tolerated by all patients.
Discussion
While PPV with ILM peeling and gas tamponade is widely accepted as the treatment of choice for primary macular holes, the evidence on how to best treat macular holes that persist following initial surgery with ILM peeling and gas tamponade is limited. Re-installation of a gas tamponade is a commonly used treatment option but has been reported to result in closure rates of only 61% or 62% even if postoperative patient positioning is applied [1, 2]. Thus, there is an unmet medical need for alternative surgical approaches with higher efficacy in persistent macular holes.
Several treatment approaches for persistent macular holes have been evaluated, such as injection of autologous platelet concentrate or whole blood into the hole, use of ILM, lens capsule, retinal tissue, or amniotic membrane for insertion into or coverage of the hole, and induction of macular detachment to mobilize the hole edges [15,16,17,18,19,20,21,22,23]. The mechanisms of macular hole closure using platelets are not fully understood, and growth factors released by the platelets with secondary migration or proliferation of Müller cells may play a role [24]. Schaub et al. recently compared the use of either autologous platelet concentrate with gas tamponade or heavy silicone oil tamponade in 35 patients with persistent macular hole and reported closure rates of 57% and 46%, respectively [3]. These results match the closure rates for persistent macular hole following use of platelet concentrate reported by other studies that range from 60 to 85% [4,5,6]. Hillenkamp et al. investigated platelet concentrate in combination with either gas tamponade or conventional silicone oil tamponade in persistent macular holes and reported a combined closure rate of 68% (n = 28) [25].
Autologous ILM flaps have been widely studied as primary treatment for idiopathic macular holes. The inverted ILM flap technique was introduced by Michalewska et al. for primary treatment of large macular holes [26]. It has been hypothesized that the ILM flap may induce glial cell proliferation and thus enhance closure. In recent meta-analyses of the inverted ILM flap technique, the anatomical closure rate was significantly higher compared to standard surgery, however without significant difference in BCVA outcome [27, 28]. In persistent macular holes, autologous ILM transplantation has also been performed, usually by peeling a free flap of residual ILM from the edge of the initial peeling area and subsequent insertion into the hole or, alternatively, by creating a pedunculated flap from the initial peel edge to cover the hole. In two studies, the closure rate after autologous free ILM transplantation and gas tamponade was 100% and mean BCVA improved significantly [18, 19]. However, with a sample size of these studies of 10 and 12 patients, more evidence is required.
Another proposed surgical technique for persistent macular holes is the induction of a temporary central retinal detachment by subretinal fluid injection. Studies using this approach reported anatomical closure rates of 85.2% (n = 41), 87.2% (n = 39), 90% (n = 10), and 100% (n = 10) together with BCVA improvement [20,21,22,23].
Treatment of persistent macular holes by silicone oil tamponade requires and additional surgery to remove the oil but may be an option for patient unable to maintain postoperative prone positioning and other selected cases. Heavy silicone oil has been evaluated in persistent macular holes as some authors consider it to be superior to conventional silicone oil due to a presumed improved retinal contact and increased conformity with the foveal depression [3, 9,10,11]. Closure rates of persistent macular holes following heavy silicone oil tamponade have been reported to range from 46 to 92% [3, 9,10,11]. Compared to heavy silicone oil, conventional (light) silicone oil is more widely available, cheaper, and requires somewhat less extensive surgery for removal. Closure rates in studies and case series investigating conventional silicone oil tamponade for persistent macular holes range from 62% (n = 13) to 100% (2 studies, n = 2 and 5) [8, 12, 13].
In our study, we investigated 33 consecutive patients with either persistent macular hole following ILM peeling and gas tamponade or recurrent macular hole, i.e. macular holes that re-opened after initial closure following ILM peeling and gas tamponade. Of these 33 patients. 90.9% were successfully treated with temporary installation of a silicone oil tamponade, resulting in both hole closure and significant mean improvement of BCVA. This closure rate is comparable to those reported for heavy silicone oil. While our study patients were allowed free positioning following silicone oil installation, some authors recommend deterring these patients from face-up positioning as this may interfere with the tamponade effect.
Our study provides retrospective results for the use of a temporary conventional silicone oil tamponade that facilitates comparison with reported outcomes of alternative surgical strategies. Limitations of our study include the retrospective design, the resulting lack of predefined patient selection criteria and standardized study examinations such as visual acuity measurements, the variability in treatment parameters such as the duration of silicone oil tamponade, and the lack of control groups with alternative treatments. However, our study provides, to the best of our knowledge, the largest reported patient cohort for the investigated treatment approach to date. In particular in patients that are unable to comply with postoperative positioning, a temporary silicone oil tamponade represents an effective treatment option for persistent macular holes. Future prospective controlled trials may add to available evidence on the efficacy of the various persistent macular hole repair techniques and help to identify the best therapeutic strategy for the affected patients.
Summary
What was known before
-
A variety of treatment strategies have been proposed for macular holes that persistent or recur after surgery.
-
The debate about the best re-treatment approach is ongoing.
-
Data on the effectiveness of conventional silicone oil tamponade in persistent macular holes is limited.
What this study adds
-
We assessed the outcome of conventional silicone oil tamponade in persistent or recurrent macular holes.
-
In 33 consecutive patients, treatment resulted in a closure rate of 90.9% and significant mean improvement of visual acuity.
-
Silicone oil tamponade represents an effective treatment option in selected patients such as those unable to comply with postoperative positioning.
Change history
13 November 2020
We updated the original HTML version of this Article shortly after publication in order to add the missing Projekt DEAL funding acknowledgement.
References
Vishal MY, Babu N, Kohli P, Rajendran A, Ramasamy K. Retrospective study of changes in ocular coherence tomography characteristics after failed macular hole surgery and outcomes of fluid-gas exchange for persistent macular hole. Indian J Ophthalmol. 2018;66:1130–5.
Rao X, Wang N-K, Chen Y-P, Hwang Y-S, Chuang L-H, Liu I-C, et al. Outcomes of outpatient fluid-gas exchange for open macular hole after vitrectomy. Am J Ophthalmol. 2013;156:326–333.e1.
Schaub F, Gözlügöl N, von Goscinski C, Enders P, Heindl LM, Dahlke C. Outcome of autologous platelet concentrate and gas tamponade compared to heavy silicone oil tamponade in persistent macular hole surgery. Eur J Ophthalmol. 2020.https://doi.org/10.1177/1120672120903704.
Degenhardt V, Busch C, Jochmann C, Meier P, Unterlauft JD, Mößner A, et al. Prognostic factors in patients with persistent full-thickness idiopathic macular holes treated with re-vitrectomy with autologous platelet concentrate. Ophthalmologica. 2019;242:214–21.
Dimopoulos S, William A, Voykov B, Ziemssen F, Bartz-Schmidt KU, Spitzer MS. Anatomical and visual outcomes of autologous thrombocyte serum concentrate in the treatment of persistent full-thickness idiopathic macular hole after ILM peeling with brilliant blue G and membrane blue dual. Acta Ophthalmol. 2017;95:e429–30.
Purtskhvanidze K, Frühsorger B, Bartsch S, Hedderich J, Roider J, Treumer F. Persistent full-thickness idiopathic macular hole: anatomical and functional outcome of revitrectomy with autologous platelet concentrate or autologous whole blood. Ophthalmologica. 2018;239:19–26.
Van De Moere A, Stalmans P. Anatomical and visual outcome of macular hole surgery with infracyanine green-assisted peeling of the internal limiting membrane, endodrainage, and silicone oil tamponade. Am J Ophthalmol. 2003;136:879–87.
Goldbaum MH, McCuen BW, Hanneken AM, Burgess SK, Chen HH. Silicone oil tamponade to seal macular holes without position restrictions. Ophthalmology 1998;105:2140–7.
Cillino S, Cillino G, Ferraro LL, Casuccio A, TREATMENT OF. Persistently open macular holes with heavy silicone oil (densiron 68) versus C2F6. A prospective randomized study. Retina. 2016;36:688–94.
Lappas A, Foerster AMH, Kirchhof B. Use of heavy silicone oil (Densiron-68) in the treatment of persistent macular holes. Acta Ophthalmol. 2009;87:866–70.
Rizzo S, Genovesi-Ebert F, Vento A, Cresti F, Miniaci S, Romagnoli MC. Heavy silicone oil (Densiron-68) for the treatment of persistent macular holes: Densiron-68 endotamponade for persistent macular holes. Graefes Arch Clin Exp Ophthalmol. 2009;247:1471–6.
Da Mata AP, Burk SE, Foster RE, Riemann CD, Petersen MR, Nehemy M árcio B, et al. Long-term follow-up of indocyanine green-assisted peeling of the retinal internal limiting membrane during vitrectomy surgery for idiopathic macular hole repair. Ophthalmology. 2004;111:2246–53.
Nowroozzadeh MH, Ashraf H, Zadmehr M, Farvardin M. Outcomes of light silicone oil tamponade for failed idiopathic macular hole surgery. J Ophthalmic Vis Res. 2018;13:130–7.
Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 2013;120:2611–9.
Chen S-N, Yang C-M. Lens capsular flap transplantation in the management of refractory macular hole from multiple etiologies. Retina. 2016;36:163–70.
Peng J, Chen C, Jin H, Zhang H, Zhao P. Autologous lens capsular flap transplantation combined with autologous blood application in the management of refractory macular hole. Retina. 2018;38:2177–83.
Grewal DS, Charles S, Parolini B, Kadonosono K, Mahmoud TH. Autologous retinal transplant for refractory macular holes: multicenter international collaborative study group. Ophthalmology. 2019;126:1399–408.
Morizane Y, Shiraga F, Kimura S, Hosokawa M, Shiode Y, Kawata T, et al. Autologous transplantation of the internal limiting membrane for refractory macular holes. Am J Ophthalmol. 2014;157:861–869.e1.
Pires J, Nadal J, Gomes NL. Internal limiting membrane translocation for refractory macular holes. Br J Ophthalmol. 2017;101:377–82.
Fotis K, Alexander P, Sax J, Reddie I, Kang CY, Chandra A. Macular detachment for the treatment of persistent full-thickness macular holes. Retina. 2019;39:S104–7.
Felfeli T, Mandelcorn ED. Macular hole hydrodissection: surgical technique for the treatment of persistent, chronic, and large macular holes. Retina. 2019;39:743–52.
Frisina R, Tozzi L, Sabella P, Cacciatori M, Midena E. Surgically induced macular detachment for treatment of refractory full-thickness macular hole: anatomical and functional results. Ophthalmologica. 2019;242:98–105.
Meyer CH, Szurman P, Haritoglou C, Maier M, Wolf A, Lytvynchuk L, et al. Application of subretinal fluid to close refractory full thickness macular holes: treatment strategies and primary outcome: APOSTEL study. Graefes Arch Clin Exp Ophthalmol. 2020;258:2151–61.
Bringmann A, Jochmann C, Unterlauft JD, Wiedemann R, Rehak M, Wiedemann P. Different modes of foveal regeneration after closure of full-thickness macular holes by (re)vitrectomy and autologous platelet concentrate. Int J Ophthalmol. 2020;13:36–48.
Hillenkamp J, Kraus J, Framme C, Jackson TL, Roider J, Gabel V-P, et al. Retreatment of full-thickness macular hole: predictive value of optical coherence tomography. Br J Ophthalmol. 2007;91:1445–9.
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology 2010;117:2018–25.
Shen Y, Lin X, Zhang L, Wu M. Comparative efficacy evaluation of inverted internal limiting membrane flap technique and internal limiting membrane peeling in large macular holes: a systematic review and meta-analysis. BMC Ophthalmol. 2020;20:14. 8
Yuan J, Zhang L-L, Lu Y-J, Han M-Y, Yu A-H, Cai X-J. Vitrectomy with internal limiting membrane peeling versus inverted internal limiting membrane flap technique for macular hole-induced retinal detachment: a systematic review of literature and meta-analysis. BMC Ophthalmol. 2017;17:219. 28
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JQL has nothing to disclose. RB has nothing to disclose. FGH reports personal fees from Acucela, grants and personal fees from Allergan, grants and personal fees from Bayer, personal fees from Bioeq, personal fees from Boehringer Ingelheim, grants and personal fees from Carl Zeiss Meditec, grants and personal fees from Genentech, grants and personal fees from Heidelberg Engineering, personal fees from Merz, personal fees from NightstarX, grants and personal fees from Novartis, personal fees from Optos, personal fees from Pixium, personal fees from Roche, and personal fees from Thea, outside the submitted work. TUK reports personal fees from Alimera Sciences, personal fees from Allergan, grants and personal fees from Bayer, personal fees from Heidelberg Engineering, grants and personal fees from Novartis, and personal fees from Roche, outside the submitted work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, J.Q., Brinken, R., Holz, F.G. et al. Silicone oil tamponade for persistent macular holes. Eye 35, 2206–2212 (2021). https://doi.org/10.1038/s41433-020-01228-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01228-9