Introduction
Posterior capsule rupture (PCR) rates are used to measure cataract surgeons’ quality. We wished to evaluate the internal non-visible surfaces of metal irrigation/aspiration (I/A) tips to identify potential mechanisms for PCR via novel metallographic imaging.
Methods
Ten metal I/A instruments underwent metallographic preparation by fine sectioning to expose inner surfaces near the aspiration opening. Analysis of inner bore, lumen, and opening aperture of metal aspiration tips was performed by optical microscopy, scanning electron microscopy (SEM), and 3D volume X-ray computational tomography (XCT). Distances from external aperture to first sharp metal surface were obtained and compared with a silicone-tipped instrument.
Results
We identified metal burrs near the aspiration apertures and manufacturing defects within all tips. XCT confirmed optical and SEM findings of significant defects and metal irregularities within aspiration tips. Samples also showed variation in lumen size/thickness, rough surfaces and material inhomogeneity, most pronounced at the internal tip. Median distance from outer aperture opening to first metal burr was 30 microns (range 10–120) and to internal tip irregularity (manufacturing flaw) was 250 microns (range 100–350). By comparison, distance to metal from the silicone outer aperture opening was 850 microns.
Conclusions
We have demonstrated the hidden sharp metallic irregularities within commonly used metal I/A tips. If an aspirated capsule encounters these sharp metal flaws, PCR could result. Minimising this risk would require lengthening potential distance between capsule and bare metal (as with polymer/silicone tips). Our study provides unique imaging evidence endorsing this principle and illustrates a hidden mechanism contributing to PCR.
Similar content being viewed by others
Introduction
Debate continues regarding the best methods to measure the quality of surgery in ophthalmology. In cataract surgery, this discussion currently focuses on visual outcomes, patient-related outcome measures (PROMs) and publishing of complication rates. In the world of big data collection, transparency and the Royal College of Ophthalmologists’ National Ophthalmology Database, concern exists that surgeons may choose to only operate on more straightforward cases to preserve their low complication figures, to the detriment of overall patient care in the population [1]. The literature suggests that higher volume surgeons have been associated with lower complication rates, but that does not reflect case mix complexity, as lower volume surgeons have been shown to operate on more complex cases [2, 3]. Despite this ambiguity, posterior capsule rupture rates are currently used as an individual marker of surgical quality in cataract surgery, regardless of the case complexity [1, 4]. As inadequate management of PCR carries a higher risk of endophthalmitis (eight times more likely—odds ratio [OR] = 7.94), retinal detachment (OR = 41.66) and cystoid macular oedema (relative risk [RR] = 2.61), it follows that all efforts should be made to reduce the incidence of PCR [5].
Appropriate case selection for training future ophthalmologists based on risk stratification has been shown to reduce the incidence of posterior capsule rupture (PCR) [6, 7]. Combined with simulation training, appropriate surgical adjunct use, refinements in techniques and equipment, modern cataract surgery is now generally safe with very successful outcomes [8, 9].
In light of this high success rate, there is a temptation to view the procedure as “just a phaco”, and therefore lose concentration after the main cataract nucleus has been removed. Trainees and consultants alike should be counselled not to adopt this mindset, as it should always be remembered that the lens capsule has a mean thickness of only 3.5 microns at the posterior pole [10]. In the early 1990s, Cruz et al. reported 72% of cases of vitreous loss occurred during cortex removal when a metal I/A tip was used by ophthalmology residents [11]. This was confirmed by Osher and Cionni (28% of the PCR occurred during I/A) and Gimbel et al. (39.7% occurring during I/A) [12, 13]. More recent research from Malaysia published in 2015 identified that PCR occurred most commonly during cortical removal (35.2%), followed by nuclear segment removal (25.4%) [14].
At the most basic level, anterior chamber stability is a balance between fluidic inflow and outflow contributing to a stable intraocular pressure to ensure the fragile internal structures (iris, capsule) remain in predictable safe positions during cataract surgery. Modern phacoemulsification machines have had their tubing, wounds, and instrumentation adapted to try and ensure a closed system arrangement to maximise stability [15].
There are a variety of coaxial and bimanual equipment options available for performing irrigation/aspiration (I/A) of lens cortex or viscoelastic removal. These include metal, polymer and silicone tips. We wanted to evaluate commonly used ‘bare metal’ instruments by utilising novel metallographic imaging techniques to identify any hidden internal flaws or irregularities, which could potentially contribute to PCR.
Methods
A variety of commonly available metal I/A instruments were obtained. Samples included a coaxial I/A from Medicel AG (Widnau, Switzerland), and a range of bimanual I/As from Bürki inno med AG (Widnau, Switzerland), BeaverVisitec International Ltd (Waltham, MA, USA), Bausch & Lomb GmbH (Heidelberg, Germany) and Alcon (Geneva, Switzerland). A silicone coaxial tip (Bausch & Lomb GmbH) was used for comparison.
Analysis of these ten metal I/A tips was undertaken at the Advanced Materials Research Laboratory, University of Strathclyde, Glasgow, UK. Metallographic preparation involved the removal of side and back wall by fine sectioning to expose the inner bore adjacent and opposite the aspiration opening. Cut edges were peeled back to reveal the inner surface. Macrophotography and microphotography was undertaken. Analysis of the inner bore, lumen and opening aperture was performed by optical microscopy and scanning electron microscopy (SEM) with the use of secondary electron mode (SE) for cross-sectional microstructural characterisation using a Hitachi S3700S tungsten filament at 15 kV.
For XCT, the tips were sectioned to 10 mm long to allow the high resolution images to be obtained. The samples were then mounted on in-house built aluminium cylindrical holders, with a central hole to host the blade tip. The blade tip was inserted into the rod and the position was maintained by gluing the tip to the holder. A Nikon XT H 225 LC X-ray computed tomography system was used to generate a 3D volume image of the discs to identify detrimental features underneath the protective ring and braze layer that may have been lost through sectioning of the discs.
The presence or absence of sharp metal at the external and internal edges of the aspiration opening was noted, as were any internal irregularities or defects. Distances from the outer aspiration opening to the first sharp/irregular metal edge were measured. These distances were compared to those for a coaxial silicone tip (Bausch & Lomb GmbH).
Results
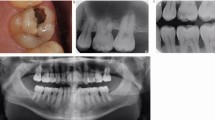
Optical micrographs before fine sectioning revealed metal irregularities visible at the aspiration apertures and irregular manufacturing defects on the external roughened surfaces often used for capsular polishing on all samples analysed [see Fig. 1]. Cross-sectioning of the metal instruments and subsequent SEM revealed significant defects and sharp metal irregularities within the external and internal aspiration apertures. All samples also showed variation in lumen size/thickness, rough surfaces and material inhomogeneity, most pronounced within the internal tip surface. The XCT scans confirmed the optical and SEM findings of significant hidden sharp metal defects within the aspiration tips. The samples all showed variation in wall thickness as well as inhomogeneity of the metal material at the closed tip of the instrument, presumed due to manufacturing methods [see Figs. 2–4].
The 3D volume renderings for both the bimanual and coaxial metal I/As revealed variability in the wall thickness, internal roughness, and inhomogeneity at the internal tip. The circle indicates poor manufacturing and a potential fracture site with marked irregularity, which is further illustrated in the cross-sectional renderings [see Fig. 5].
The median distance from the outer aperture opening to the first metal burr was 30 microns (range 10–120 microns), with most burrs present within the entrance of the aspiration aperture. The median distance from the outer opening to the internal tip irregularity (manufacturing flaw) was 250 microns (range 100–350 microns). By comparison, the distance to any metal surface from the outer aperture opening of a sample silicone I/A tip (Bausch & Lomb GmbH) was 850 microns.
Discussion
In 1987, Docherty noted that certain co-axial equipment designs for I/A can confer intrinsic dangers, particularly when the removal of cortical material is hampered by the steepness of instrument approach, leading to potential PCR [16]. He went on to make suggested improvements to the original coaxial needle, creating a 45 degree bend to allow rotational movement, and suggested standardisation of the length of the projecting tip (1.5 mm with a slightly bulbous end to eliminate snagging the posterior capsule) [16]. Other authors identified attempted removal of the sub-incisional cortex with a coaxial approach as the main contributor to PCR and made surgical advances including a J-shaped irrigating cannula to free these awkward cortical adhesions, changeable tips and wound modifications [17, 18].
A further major step forward in surgical safety was associated with the development of a bimanual I/A technique. Separation of irrigation and aspiration through smaller side-port incisions (rather than the larger main wound) encouraged greater anterior chamber stability and consequently reduced the potential anterior billowing movements of the posterior capsule [19,20,21]. The greater potential angles of approach with bimanual instrumentation enabled better ease of access to the cortex, and this was resulted in a reported reduction in PCR.
Modern cataract machine manufacturers pride themselves in improved anterior chamber stability, and this, combined with the bimanual approach, can help to minimise abnormal iris movement in intraoperative Floppy Iris Syndrome, as the irrigation remains above the iris plane and could have a dampening effect on the unstable iris behaviour [22]. This contrasts with coaxial I/A systems, as irrigation beneath the floppy iris will induce greater billowing movements and encourage the iris to seek lower pressure gradients by prolapsing through the corneal incisions.
Scanning electronic microscopy (SEM) has been previously utilised to evaluate metal instruments associated with PCR [23]. In that study, SEM of the tip revealed burrs on the aspiration portion of the tip, as well as poor finishing around the irrigation ports. Our study is the first to investigate the internal hidden structures through SEM, XCT and novel 3D reconstruction. We found the evidence of internal irregularities, sharp metal burrs, manufacturing tapering flaws, rough edges within areas of lumen narrowing and discontinuities to a variable degree within all the metal instruments we surveyed. These findings are clearly illustrated in our Figs. 1–5. Additionally, our use of 3D reconstruction is unique within the ophthalmic literature and highlights the short distances involved between the external aspiration openings to the irregular and sharp internal crimping within the end of the metal tips.
It follows that one method to avoid this intrinsic risk would involve switching from “bare metal” to non-metal options for I/A, such as silicone and/or polymer tips. Fifteen years ago, Blomquist and Pluenneke reported a significant reduction in vitreous loss associated with I/A following switching from a metal (1.2%) to a silicone tip (0.1%; p = 0.004) [24]. More recent publications have confirmed this finding, particularly in the teaching hospital setting [25].
Silicone tip I/A instrumentation, associated with appropriate case-selection from evidence-based identification of risk factors has been heralded as one of the major advances in modern cataract surgery training, resulting in better outcomes due to reductions in PCR rates [6, 7, 25]. Maubon and Ursell recently published a retrospective analysis of cataract surgeries performed by trainee surgeons before and after the introduction of a silicone-tipped I/A. Their non-silicone I/A (conventional) group performed 782 surgeries and had a PCR rate of 3.6% versus 1.6% from 933 surgeries in the silicone-tip I/A group. Although this difference was not found to be statistically significant following adjustment for risk factors (p-value 0.057), it was notable that the silicone tip group had no I/A-related PCR complications (vs. 12% in the non-silicone group) [25]. This paper requires further consideration as to the clinical significance to the patient from these two approaches, particularly in the university hospital teaching environment. However, even modern instrumentation is not flawless. Temel and Osher advised “surgeons must be vigilant as to the possibility that any instrument can be inadvertently damaged” [26]. They have reported PCR due to unexpected metal burrs on a Y-hook metal instrument used for positioning an IOL, and the potential for IOLs to have irregular sharp edges which can traumatise the capsule [26]. Even silicone-based instruments are not immune. PCR can occur if there is misalignment of the silicone tip related to the metal shaft [27]. SEM of reusable silicone tip instruments associated with cases of PCR implicated hidden metal burrs of the inner metallic shafts and corresponding tears in the silicone sleeves [28]. These reports demonstrate the inherent concern with reusable instrumentation being vulnerable to unknown damage during the sterilisation process and supports the benefits of reliable, high-quality, single use instruments [29]. Their authors recommended that manufacturers should ‘eliminate metallic burrs on any instrument that could contact the posterior capsule at any timeʼ [27, 28].
Our paper provides photographic and novel 3D XCT reconstruction evidence of the potential intrinsic and internal sources of sharp metal and gives additional insight as to the potential mechanism of PCR during cortical removal. The cataract surgeon is attempting to cleave and aspirate loose cortex, leaving behind the delicate support structures of the capsule, which is held in place by the zonules. Our research would suggest that PCR could occur whenever the capsule is inadvertently brought into contact with hidden sharp metal, either at the internal aspiration apertures or irregularities within the metal tip. If these abnormal features did not exist, then the capsule would continue to be aspirated and if persisted with, would result in zonule damage and capsule dislocation. This has been observed clinically with the use of silicone tip I/A (i.e., smooth, no sharp metal) and so requires adaption in surgical technique to avoid capsule loss in the setting of weak zonules [30].
Limitations and proposal for future research
This work has revealed the internal (hidden) irregularities within commonly used metal I/A equipment. We assume that these sharp regions contribute to PCR whenever the capsule encounters these flaws. Further work is indicated to discern the rate of PCR in ophthalmic surgical centres which use metal tipped instrumentation compared to those which use polymer and/or silicone I/A tips, including the cost implications and benefits of each approach. This level of equipment detail is not currently available from the complications data in the National Ophthalmology Database for cataract surgery in the UK. However, any cost analysis of surgical instrumentation use should also consider the real-world costs of managing versus avoiding PCR. The true costs of managing PCR are significantly greater, as PCR has immediate and longer-term implications for the patient beyond the operating theatre [9].
Conclusion
Through applying novel metallographic techniques to fine bore ophthalmic instruments, we have demonstrated the inherent internal metallic irregularities within commonly used metal I/A tips. These hidden metal edges could contribute to PCR and this paper gives clarity as to the mechanisms involved in this intraoperative complication during cortical or viscoelastic removal by irrigation/aspiration. One way to minimise this risk would be to lengthen the potential distance between the capsule and ‘bare metal’, as is the case with polymer and/or silicone tips. Clinical publications suggest trainee silicone I/A tip use results in significant reduction (even elimination) of PCR. Our study provides unique and clear evidence endorsing this ‘non-metal’ principle, by demonstrating the inherent dangers of metal instruments containing unknown sharp and irregular internal edges.
What was previously known
-
Posterior capsule rupture (PCR) rates are used as a marker of cataract surgical quality.
-
There are a variety of coaxial and bimanual irrigation/aspiration (I/A) metal tips commonly used for cortical removal.
-
The mechanism of PCR associated with metal tips has not been clearly demonstrated.
What we now know
-
We have demonstrated the inherent hidden metallic irregularities (median distance 30 microns) within commonly used I/A tips through scanning electronic microscopy and X-ray computational tomography 3D reconstruction.
-
This study provides evidence as to a potential mechanism resulting in PCR during the I/A stage of cataract surgery.
-
One way to minimise this risk would be to lengthen the potential distance between the capsule and ‘bare metal’, as is the case with polymer or silicone tips (distance to metal 850 microns).
References
Qin VL, Conti FF, Singh RP. Measuring outcomes in cataract surgery. Curr Opin Ophthalmol. 2018;29:100–4.
Stein JD. Serious adverse events after cataract surgery. Curr Opin Ophthalmol. 2012;23:219–25.
Habib MS, Bunce CV, Fraser SG. The role of case mix in the relation of volume and outcome in phacoemulsification. Br J Ophthalmol. 2005;89:1143–6.
Johnston RL, Taylor H, Smith R, Sparrow JM. The Cataract National Dataset electronic multi-centre audit of 55,567 operations: variation in posterior capsule rupture rates between surgeons. Eye. 2010;24:888–93.
Day AC, Donachie PH, Sparrow JM, Johnston RL, Royal College of Ophthalmologists’ National Ophthalmology Database. The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 1, visual outcomes and complications. Eye. 2015;29:552–60.
Nderitu P, Ursell P. Updated cataract surgery complexity stratification score for trainee ophthalmic surgeons. J Cataract Refract Surg. 2018;44:709–17.
Kim BZ, Patel DV, McKelvie J, Sherwin T, McGhee CNJ. The Auckland cataract study II: reducing complications by preoperative risk stratification and case allocation in a teaching hospital. Am J Ophthalmol. 2017;181:20–25.
Ferris JD, Donachie PH, Johnston RL, Barnes B, Olaitan M, Sparrow JM. Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 6. The impact of EyeSi virtual reality training on complications rates of cataract surgery performed by first and second year trainees. Br J Ophthalmol. 2020;104:324–9.
Jamison A, Benjamin L, Lockington D. Quantifying the real-world cost saving from using surgical adjuncts to prevent complications during cataract surgery. Eye. 2018;32:1530–6.
Barraquer RI, Michael R, Abreu R, Lamarca J, Tresserra F. Human lens capsule thickness as a function of age and location along the sagittal lens perimeter. Invest Ophthalmol Vis Sci. 2006;47:2053–60.
Cruz OA, Wallace GW, Gay CA, Matoba AY, Koch DD. Visual results and complications of phacoemulsification with intraocular lens implantation performed by ophthalmology residents. Ophthalmology. 1992;99:448–52.
Osher RH, Cionni RJ. The torn posterior capsule: its intraoperative behavior, surgical management, and long-term consequences. J Cataract Refract Surg. 1990;16:490–4.
Gimbel HV, Sun R, Ferensowicz M, Anderson Penno E, Kamal A. Intraoperative management of posterior capsule tears in phacoemulsification and intraocular lens implantation. Ophthalmology. 2001;108:2186–9.
Thanigasalam T, Sahoo S, Ali MM. Posterior capsule rupture with/without vitreous loss during phacoemulsification in a hospital in Malaysia. J Asia Pac J Ophthalmol. 2015;4:166–70.
Benjamin L. Fluidics and rheology in phaco surgery: what matters and what is the hype? Eye. 2018;32:204–9.
Docherty PT. A modified irrigating-aspirating needle. Br J Ophthalmol. 1988;72:368–9.
Dewey SH. Cortical removal simplified by J-cannula irrigation. J Cataract Refract Surg. 2002;28:11–4.
Hagan JC III. Irrigation/aspiration handpiece with changeable tips for cortex removal in small incision phacoemulsification. J Cataract Refract Surg. 1992;18:318–20.
Colvard DM. Bimanual technique to manage subincisional cortical material. J Cataract Refract Surg. 1997;23:707–9.
Brauweiler P. Bimanual irrigation/aspiration. J Cataract Refract Surg. 1996;22:1013–6.
Sakamoto T, Shiraki K, Inoue K, Yanagihara N, Ataka S, Kurita K. A simple, safe bimanual technique for subincisional cortex aspiration. Ophthalmic Surg Lasers. 2002;33:337–9.
Lockington D, Gavin MP. Intraoperative floppy-iris syndrome: role of the bimanual approach. J Cataract Refract Surg. 2009;35:964.
Reed-Miller C, Heslin K, Liebowitz S. Scanning electron microscopy of an irrigation/aspiration tip following a posterior capsular rupture. J Am Intraocul Implant Soc. 1985;11:391–2.
Blomquist PH, Pluenneke AC. Decrease in complications during cataract surgery with the use of a silicone-tipped irrigation/aspiration instrument. J Cataract Refract Surg. 2005;31:1194–7.
Maubon LG, Ursell PG. Reduced posterior capsular rupture rate observed among trainee surgeons utilizing a disposable silicone-tipped irrigation and aspiration handpiece for soft lens removal. Expert Rev Ophthalmol. 2018;13:293–7.
Temel M, Osher RH. Posterior capsule tear resulting from faulty instrumentation. J Cataract Refract Surg. 2003;29:619–20.
Barros MG, Osher RH. Posterior capsule tear caused by misalignment within a silicone irrigation/aspiration tip. J Cataract Refract Surg. 2004;30:1570–1.
Hart JC Jr, Tanner M, Rooney DM. Electron microscopy of silicone irrigation/aspiration tips involved in posterior capsule rupture. J Cataract Refract Surg. 2018;44:1517–20.
Lockington D, Macdonald E, Mantry S, Ramaesh K. A case for single-use disposable corneal forceps: equipment reliability should be the primary concern. Br J Ophthalmol. 2010;94:388–9.
Nakano CT, Motta AF, Hida WT, Nakamura CM, Tzelikis PF, Ruiz Alves M, et al. Hurricane cortical aspiration technique: one-step continuous circular aspiration maneuver. J Cataract Refract Surg. 2014;40:514–6.
Acknowledgements
A version of this paper is a free paper presentation at the (virtual) 38th ESCRS Congress in October 2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Nil relevant to this work. DL has received educational and KOL honoraria from Alcon, Bausch & Lomb, Santen and Thea. AM, TM, FS: nothing to declare.
Consent for publication
Granted.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lockington, D., Macente, A., Marrocco, T. et al. Novel internal analysis of metal irrigation/aspiration tips could explain mechanisms of posterior capsule rupture. Eye 35, 1915–1921 (2021). https://doi.org/10.1038/s41433-020-01181-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01181-7