Abstract
Purpose
To report the demographics, frequency of potential predisposing factors, presentation and outcomes of Acanthamoeba keratitis (AK) at a quaternary eye hospital in Sydney, Australia over a 15-year period.
Methods
A retrospective review of all patients diagnosed with AK at the Sydney Eye Hospital, Sydney, Australia between January 2002 and December 2016 was conducted.
Results
A total of 52 patients with AK at the quaternary referral hospital in Sydney, Australia, between January 2002 and December 2016, were included. The most commonly documented potential predisposing factors were contact lens wear (83%) and organic trauma (10%) in the non-contact lens wearers. An initial misdiagnosis of herpetic eye disease was made in 37% of patients. The presenting clinical features in order of frequency included; punctate epitheliopathy in 65% (n = 34), perineural infiltrate 46% (n = 24), stromal infiltrates 46% (n = 24), anterior uveitis 39% (n = 20), epithelial defect 35% (n = 18), limbitis 31% (n = 16), pseudo-dendrite 19% (n = 10), and ring infiltrate 4% (n = 7). Twenty-seven of the patients completed their follow-up at the Sydney Eye Hospital, improving their vision from 1.02 logMAR at presentation to 0.57 logMAR at last follow-up. Thirty-nine complications developed in 32 eyes and included corneal scarring and vascularisation, three patients experienced recurrences of AK and one patient developed a late-onset scleritis.
Conclusion
In Australia, AK occurred predominantly in contact lens wearers with typical clinical features including epitheliopathy and perineural infiltrates. The patient demographics, frequency of potential predisposing factors and clinical presentation of AK were similar to case series from the UK and New Zealand.
Similar content being viewed by others
Introduction
Acanthamoeba species are ubiquitous, free living amoeba living in soil and water and are an opportunistic human pathogen. The organism was first reported to cause keratitis (AK) in 1973 [1]. Since then the incidence of AK has been increasing, this has been attributed to increased contact lens (CL) wear and improved diagnostic yield [1,2,3]. The incidence varies significantly in different population groups, and is estimated to be 1–2 per million contact lens wearers in the United States [4]. The majority (88–96%) of AK occurs in CL wearers, with poor lens hygiene and water exposure the leading risk factors [3, 5,6,7,8,9,10]. In non-contact lens wearers, AK is commonly associated with ocular trauma involving organic matter or water exposure [6]. The most common primary misdiagnosis in these patients is herpes simplex keratitis, made in up to 70% of cases [5].
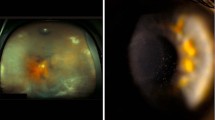
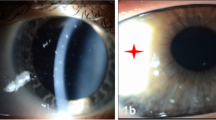
Acanthamoeba infection involves the epithelium of the cornea first and extends to involve the deeper layers progressively. Clinical features therefore follow chronologically as deeper layers of the cornea become involved, namely; epitheliopathy, pseudo-dendrites, perineurial infiltrates, ring infiltrate, corneal ulceration, hypopyon, scleritis, and a stromal abscess. Pain out of proportion to the clinical picture is commonly cited, but may be absent in some cases [1,2,3].
Variations exist in the management of these patients with cysticidal agents as the mainstay of therapy and adjunctive therapies include the use of anti-fungals, antibiotics, corticosteroids, and immunosuppressives [1, 2, 11, 12]. The prognosis of AK is directly related to the time it takes to initiate anti-amoebic therapy. A case series in the UK showed all patients that were diagnosed and started anti-amoebic therapy within a month recovered 6/12 vision or better, whereas only 64% of patients diagnosed after a month achieved this [5, 13]. A late diagnosis is also more commonly associated with the need for corneal surgery in the management algorithm [7].
Regional variation in AK has been reported, which can be related to environmental differences and contact lens wear habits [14]. Knowledge of regional variations in AK can assist in the prevention, diagnosis, management and determination of prognosis. Current data on AK in Australia is lacking, with only two case series in the literature [8, 15]. To our knowledge this is the largest case series of AK in Australia reporting on the demographics, frequency of potential predisposing factors, presentation and outcomes over a 15-year period at a quaternary eye hospital.
Methods
A retrospective review of all patients diagnosed with AK at the Sydney Eye Hospital, over a 16 year period, January 2002–December 2016 was conducted. The research protocol adhered to the Declaration of Helsinki and was approved by the Human Research Ethics Committee of the South Eastern Sydney Local Health District (13/338).
Patients with AK in New South Wales, Australia, received topical cysticidal treatment from the Sydney Eye Hospital pharmacy. All investigations for AK were processed through the South Eastern Area Laboratory Service (SEALS) with all confocal microscopy investigations performed at the Sydney Eye Hospital (SEH). Cases were therefore identified from the Sydney Eye Hospital pharmacy and SEALS databases. Patients were included if they had medical records at the SEH and a diagnosis of AK was confirmed. A diagnosis was confirmed if acanthamoeba spp. were identified on culture, polymerase chain reaction (PCR) or confocal microscopy (CM); or if they had perineurial infiltrates, or if they had a typical clinical course with a therapeutic response only to anti-amoebic agents [2].
Patients were excluded if they had investigations for acanthamoeba conducted at a laboratory other than SEALS, did not have confocal microscopy on record or had been commenced on anti-amoebic therapy before presentation as the diagnosis of AK could therefore not be confirmed with certainty. In the case of bilateral ocular involvement only one eye was included in the study, as decided by simple randomisation.
Data collected from the medical records were entered into a REDCap database designed for the study [16]. Data included demographics, patient history, documentation of potential predisposing factors, contact lens history, clinical features, pathology results, management and outcomes.
Clinical criteria
The clinical features of AK, identified from a review of the literature [1,2,3, 9, 11], were recorded if present as; keratitis with pain out of proportion to the clinical picture; punctate epitheliopathy; pseudodendrites; epithelial defect; perineurial infiltrate; epithelial and sub-epithelial infiltrates; ring infiltrate; limbitis; anterior uveitis; hypopyon; corneal thinning; scleritis and dacryoadenitis.
Disease stage at presentation was divided into three categories [17]. Stage 1 AK was defined as the presence of corneal epitheliopathy only. Stage 2 AK was the presence of a corneal epithelial defect, perineural infiltrate, or stromal infiltrate in addition to stage 1 findings. Stage 3 disease required the presence of a corneal ring infiltrate and one or more features of stage 2 disease.
Diagnostic tests
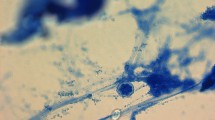
All patients had a corneal scrape, whereby superficial corneal samples were directly smeared onto glass slides and inoculated onto culture media in the clinic. Acanthamoeba was detected on microscopy of the glass slide; culture of non-nutrient or water agar plates with an E. coli overlay or PCR. Confocal microscopy was performed in the clinic by an experienced technician.
For some patients with progressive or non-resolving keratitis a corneal biopsy was performed. In our institution, the specific corneal biopsy technique varied by surgeon as outlined previously [18]. The specimen was divided into two halves, one placed in non-preserved saline for delivery to the microbiology laboratory, and the other half in formalin for histopathological examination.
Statistical analysis
The prevalence of potential predisposing factors, outcome data such as visual acuity were summarised using descriptive statistics. Temporal trends in the number of cases of keratitis were plotted over the 15-year period and the case load per month compared between the swimming months in Sydney, NSW, Australia (December–April) and the remainder of the year. Linear regression was used to investigate determinants of final visual acuity. This model investigated the impact of treatment delays defined as 21 days or longer based on previous research [17] and for the stage of disease at presentation, adjusting for age, sex, ocular and systemic disease.
Results
Patient demographics
Fifty-two patients were diagnosed with AK at the Sydney Eye Hospital during the period January 2002–December 2016 with a preponderance of females (60%). Demographic data for the included patients are shown in Table 1a. Four patients had bilateral involvement, of the remaining 48 patients the right eye was involved in 54% (n = 26) of the cases and the left in 46% (n = 22).
Potential predisposing factors
Ten patients had pre-existing ocular conditions and eight pre-existing systemic conditions (Table 1b). Contact lens wear was documented in 83% (n = 43) of patients (Table 1c). Soft contact lenses with a monthly replacement schedule was the predominant lens in use. (Table 2) The specific CL-related potential predisposing factors identified were water exposure in 47% (n = 20), overnight wear 21% (n = 9) and uninterrupted continuous wear for two-month periods in a patient (n = 1) with cosmetic CL. The monthly caseload over the study period of AK was higher in the summer months (December–April) with 5.4 cases per month versus 3.3 cases per month for the rest of the year, indicating a seasonal variation favouring the swimming months (Fig. 1).
Corneal abrasions following trauma were documented in 8% (n = 4) and organic matter was present in all these cases. Two patients (4%) had a history of a corneal foreign body on presentation. Lastly, water exposure was documented in 27% (n = 14) of patients, where 21% (n = 3) were non-CL wearers and had no history of ocular foreign bodies or trauma.
Presenting features
The time from the onset of symptoms to first presentation ranged from 0 to 25 days, with a mean of 4 days. The first recorded point of contact was an ophthalmologist in 54% (n = 28), general practitioner (GP) 21% (n = 11), optometrist 6% (n = 3) and directly to the hospital in 19% (n = 10).
Thirty patients (58%) were being treated with a topical antibiotic on presentation and 19 patients (37%) were being treated for herpetic eye disease with an antiviral agent.
Best corrected visual acuity in the affected eye on presentation ranged from 0 to 4 logMar with a mean of 1.0 logMar. The vision was corrected in 64% (n = 33) of patients, with spectacle correction in 94% (n = 31), soft CLs 3% (n = 1) and scleral lenses 3% (n = 1).
Pain out of proportion to the clinical signs was seen in 35% of the patients at presentation (Table 3). Punctate epitheliopathy (65%, n = 34), perineural infiltrate (46%, n = 24) and infiltrates (46%, n = 24) were the most common clinical findings. The remaining presenting clinical features and their frequency are highlighted in Table 3. Intra-ocular pressure was documented in 56% (n = 29) of patients on presentation and was raised above 21 mmHg in one of these patients.
The time from symptom onset to presentation at the hospital ranged from 1 to 195 days (mean: 26 days) and the time from symptom onset to the initiation of anti-amoebic therapy ranged from 1 to 222 days (mean: 29 days).
Patients were staged according to disease severity, with nine patients in stage 1 (17%), 36 in stage 2 (69%) and seven classified as stage 3 disease (14%) (Table 3). The mean duration from onset to stage 1, 2 and 3 disease was 23 ± 29, 30 ± 48 and 31 ± 37 days, respectively, (p = 0.69). The mean final BCVA for stage 1, 2 and 3 patients was −0.03 ± 0.05, 0.50 ± 0.82 and 1.32 ± 1.69 logMAR, respectively, (p = 0.04).
Anti-amoebic agents were started at the discretion of the treating doctor and included: polyhexamethylene biguanide (PHMB) (n = 46), chlorhexidine (n = 34) and propamidine (n = 48). Twenty-eight patients used a combination of three agents initially, while 23 used dual therapy and one patient used a single agent. The mean duration of therapy was 11 months. Oral voriconazole was used as an adjunctive agent in nine patients, which decreased the duration of anti-amoebic therapy from an average of 12–9 months, when compared to patients not using adjunctive voriconazole.
Outcomes
Patients were admitted for their initial management in 89% (n = 46) of cases. Four patients were admitted more than once, ranging from 2 to 5 admissions. Twenty-seven (52%) patients completed their follow up at the hospital, requiring a mean of 15 (range: 4–66) follow-up outpatient visits. The final visit recorded for management of the AK was between 1 and 182 months following presentation, mean 33 months.
Visual acuity at the last visit ranged from −0.10 to 4.00 logMAR with a median of 0.57 logMAR (Table 4a). Patients who were started on treatment within 21 days of symptom onset had a final corrected mean VA of 0.35 ± standard deviation (SD) 1.02, and those started on treatment after 21 days had a final corrected mean VA of 0.86 ± SD 0.98 (p = 0.2).
Ten corneal procedures were performed in five of the patients, including biopsies (n = 6) for a tissue diagnosis, therapeutic penetrating keratoplasty for disease control (n = 1), and for an optical indication penetrating keratoplasties (n = 2), and a deep anterior lamellar keratoplasty (n = 1). There were no recurrences in the three transplants performed for visual recovery and two of these grafts were surviving at the last follow up, recorded at 9 and 10 years post presentation.
Complications of AK in our series were documented in 32 patients (62%) and detailed in Table 4b. Patients with scarring and vascularisation had a final corrected VA of 0.69 (95% confidence interval [CI], 0.18–1.20), whereas those without had a final corrected VA of 0.17 (95% CI, −0.28 to 0.61), p = 0.28.
Discussion
Our retrospective case series includes 52 patients diagnosed with AK at a quaternary eye hospital in Sydney, Australia between January 2002 and December 2016. The demographics demonstrated a female preponderance and a mean age of 39 years, which is similar to other case series in the UK and New Zealand [6, 8]. Contact lens wear was the most commonly reported predisposing factor, followed by organic trauma in the non-CL wearers. It is of interest to note that four cases were associated with orthokeratology, a relatively uncommon practice that is proposed as a means of myopia control but with an uncertain safety profile [19,20,21]. Twenty-seven of the patients completed their follow-up at the Sydney Eye Hospital, with a mean visual recovery to 0.57 logMar from 1.02 logMar at presentation. Patients developed corneal scarring and vascularisation as the main complications.
Our case series showed an annual caseload of 3.5 cases per year. A retrospective review by Butler et al. [8] from 1997 to 2002, reviewed 20 patients with AK at the Sydney Eye Hospital and reported an annualised rate of three cases/year. The number of cases each year in our study ranged from 1 to 4 cases, except in 2007 and 2014 where there were ten and seven new cases, respectively. The number of cases in 2007 could be accounted for by the outbreak associated with the use of the AMO complete moisture plus multipurpose cleaning solution, with a similar rise in cases reported in Brisbane in that year [15, 22]. The increased cases in 2014 are not mirrored elsewhere in the literature. The mean annual number of cases after 2007 was 3.6 cases per year, which is higher than the average of 2.6 cases per year before 2007. This is likely attributed to the gradual increase in the use of CL but could also be related to increased case detection and/or expansion of services at this clinic.
Predisposing factors
Contact lens use was the most prevalent potential predisposing factor, reported in 83% (n = 43) of cases, with soft CLs being used most frequently (n = 34), in keeping with the prevalence of use of these CLs [23]. This is well documented in peer literature where CL use ranges from 80 to 96% in AK cases [3, 5,6,7,8]. In addition to the use of CLs, we assessed documentation of behaviour patterns of the CL wearers. Water exposure, almost equally shared between tap and swimming water, was the most commonly documented behaviour. Seawater exposure occurred in 45% of patients that reported swimming with their lenses, which is likely attributed to the coastal location of the city. In contrast, sea water exposure was found to be a risk factor and prevalent in 21% of AK patients in a study by Redford et al. [6] in the UK, with chlorinated water (52%) the leading water related risk factor. The monthly number of cases of AK over the study period was higher (5.4 vs 3.3) in the summer months (December–April), indicating a seasonal variation favouring the swimming months (Fig. 1). This may also be accounted for by the warmer weather as AK incidence has been reported to be higher in warmer climates and summer months in other settings [3, 14].
In the non-CL wearers, trauma associated with organic matter (in 10%) was the leading potential predisposing risk factor reported, which is in keeping with case series from the UK and Australia [1, 2, 11]. In the remaining five patients, two patients reported exposure to water as an isolated potential predisposing factor, and three patients had no discernible predisposing factor to developing AK. Sharma et al. [24] reported cases of non-CL related AK in Southern India, with organic material trauma implicated in 38% of patients, isolated water exposure in 8% and no identifiable risk factor in 51% of patients.
Presentation
Patients presented most commonly (54%) to an Ophthalmologist before being referred to the Sydney Eye Hospital. This is interesting in a country with well-established GP and optometrist networks, as it would be expected that a GP or optometrist would be the first point of contact. Keay et al. [25] reported on the referral pathways for microbial keratitis in Australia and New Zealand and found that 75% of patients were seen by a GP or optometrist first. It is likely that the referral documented in the patient records was the final path of referral and that the patient may have in fact started at a GP or optometrist before being referred to an ophthalmologist and finally to the Sydney Eye Hospital.
The mean VA at presentation was 1.02 logMar, of which 64% was corrected. Intra-ocular pressure (IOP) was in the normal range in 90% of patients, with only one patient whose IOP was between 21 and 30 mmHg. With HSK as the leading misdiagnosis in AK [2], this may be a factor that can help distinguish between the two in advanced cases, as herpes simplex stromal and endothelial keratitis have been shown to be associated with an increased IOP in 38% of cases [26]. We were unable to identify a pattern of clinical features distinct to early or late disease presentation. This is in contrast to other case series where limbitis, perineurial infiltrates, and punctate keratitis were predominate in early disease; and limbitis, ring infiltrate, uveitis, and epithelial loss predominating in late disease [5, 8]. It is interesting to note that only 35% of patients reported severe pain and 46% had a perineurial infiltrate, both of which are considered defining features of AK [2].
The delay from symptom onset to initiation of anti-amoebic therapy ranged from 1 to 222 days, with a mean of 29 days. Two patients were outliers, one with delayed presentation (195 days) and one that was managed as HSK for 220 days before being referred to the hospital. Removing these two outliers, brings the mean duration from symptom onset to initiation of anti-amoebic therapy to 22 days. It is commonly reported in the literature that HSK is the most common misdiagnosis for AK [5, 6]. Our study found that 37% of patients were being treated for HSK at presentation. In 20% of our early AK cases, presentation was with a dendritic ulcer compared with up to 70% of cases in reported literature [5]. In addition, patients may have a co-infection with herpes simplex that may complicate the clinical picture [27]. This highlights the importance of maintaining a high index of suspicion for AK in CL wearers and patients who have sustained corneal trauma involving organic material, even in the presence of a positive bacterial/fungal culture or viral PCR [2]. A patient with keratitis not responding to appropriate management based on a microbiology result should be re-investigated.
Fifty-one patients were started on a combination of anti-amoebic agents and nine were given adjunctive oral voriconazole. The voriconazole decreased the average duration of anti-amoebic therapy by 3 months. Patients who were started on treatment within 21 days of symptom onset had a trend to better vision, but this was not statistically significant (p = 0.2). This is in contrast to Dart et al. [2], who found that early treatment, within 3 weeks, was a good prognostic indicator. However, smaller AK case numbers in the current series may account for the lack of a significant finding.
Outcomes of Acanthamoeba keratitis
Patients were staged according to disease severity, with nine of the patients in stage 1, 32 in stage 2, and seven in stage 3, with patients with more advance disease having poorer vision [17]. This highlights the relationship between more advanced AK and poorer final visual outcome. Stage of disease at presentation showed a statistically significant correlation to visual outcomes, with stage 1 disease having a better final BCVA (p = 0.04). Similarly, Robaei et al. [17] described a fivefold increase in the odds of a poor visual outcome in patients with stage 3 disease compared to stage 1.
Twenty-seven patients completed their follow-up at the Sydney Eye Hospital, with a mean of 15 outpatient visits; highlighting the burden to the patient and health system of AK. A medical cure was achieved in 96% of patients, with only one patient requiring a penetrating keratoplasty to achieve disease control. This is higher than an earlier series at the same hospital, where the medical cure rate was 86% [5]. Mean VA improved from 1.02 to 0.57 logMar of which 82% was corrected. Three patients underwent optical keratoplasty, of which two grafts were clear at the last follow-up. This contrasts to the study by Butler et al. [8] at our institution from 1997 to 2002, who had a surgical intervention rate of 35%, with five of the seven patients having the surgery for disease control and a higher recurrence rate of 25% to the 11% in our study. The difference may be explained by a delay in the initiation of anti-amoebic therapy; as the mean duration of therapy was 11 months in our series versus 18 months in the series by Butler et al. An earlier study by Bacon et al. [5] had a surgery rate of 32%, of which 62% were performed in inflamed eyes for disease control. This reflects the increased reliance and efficacy of medical therapy to achieve a cure in these patients. Indeed, a recent large case series reported poor outcomes in patients undergoing therapeutic keratoplasty with better visual outcomes in patients who underwent an optical keratoplasty [28]. Supporting our findings that medical therapy alone can achieve a cure in most cases.
Corneal scarring and vascularisation were the two most common complications of AK in our series, occurring in 72% and 19% respectively. This developed more commonly in patients using PHMB. Of note no patients developed glaucoma, which contrasts with Kelley et al. [29] reporting a 30% incidence of secondary glaucoma after AK.
Our retrospective study had inherent limitations including selection bias. Data were collected from patient records and hence the completeness of the data set was dependent on the quality of these records. Data documenting follow-up to quiescence were available in 52%, limiting the statistical power of the outcomes data, as the Sydney Eye Hospital is a referral hospital for a large geographic area, such that patients who are improving on treatment complete follow up at their local ophthalmologist. This may have skewed the results, in that the outcomes may represent a higher proportion of complicated patients who completed follow up at the Sydney Eye Hospital. Despite these limitations this is a large contemporary case series of consecutive AK cases at a quaternary referral hospital in Australia and provides valuable clinical and epidemiologic data.
Over 15 years in Sydney, Australia 52 patients were diagnosed with AK. Demographics, potential predisposing factors, presentation and outcomes were similar to that reported in case series and epidemiologic studies from other geographic locations [5, 6, 8]. Despite increasing awareness of AK, we found delays in diagnosis and initiation of anti-amoebic therapy highlighting the need for increased vigilance. Over the 15-year period, the mean incidence of AK increased from 2.6 cases per year before 2007 to 3.6 cases per year after 2007. Following AK vision was reduced and some patients were left with life-long ocular morbidity. Timely diagnosis and improved therapies are needed.
Summary
What was known before
-
Contact lens is the leading cause of Acanthamoeba keratitis.
-
Early diagnosis is associated with improved visual outcomes.
-
Acanthamoeba keratitis is a challenging diagnosis to make.
What this study adds
-
There is an increase in the incidence of Acanthamoeba keratitis in Australia.
-
The summer months are associated with a higher number of new cases of Acanthamoeba keratitis.
-
There is a greater medical cure rate than previously with surgery reserved for optical visual rehabilitation.
References
Illingworth CD, Cook SD. Acanthamoeba keratitis. Surv Ophthalmol. 1998;42:493–508.
Dart JKG, Saw VPJ, Kilvington S. Acanthamoeba keratitis: diagnosis and treatment update 2009. Am J Ophthalmol. 2009;148:487–.e2.
Radford CF, Lehmann OJ, Dart JK. Acanthamoeba keratitis: multicentre survey in England 1992–6. Br J Ophthalmol. 1998;82:1387–92.
CDC—Acanthamoeba Infection—Resources for Health Professionals—Acanthanmoeba Keratitis Fact Sheet. (2017). Available at: https://www.cdc.gov/parasites/acanthamoeba/health_professionals/acanthamoeba_keratitis_hcp.html. (Accessed: 14th October 2017).
Bacon AS, et al. A review of 72 consecutive cases of Acanthamoeba keratitis, 1984–92. Eye. 1993;7:719–25.
Radford CF, Minassian DC, Dart JKG. Acanthamoeba keratitis in England and Wales: incidence, outcome, and risk factors. Br J Ophthalmol. 2002;86:536–42.
Patel DV, Rayner S, McGhee CN. Resurgence of Acanthamoeba keratitis in Auckland, New Zealand: a 7-year review of presentation and outcomes. Clin Exp Ophthalmol. 2010;38:15–20.
Butler TK, et al. Six-year review of Acanthamoeba keratitis in New South Wales, Australia: 1997–2002. Clin Exp Ophthalmol. 2005;33:41–46.
Radford CF, Bacon AS, Dart JK, Minassian DC. Risk factors for acanthamoeba keratitis in contact lens users: a case-control study. BMJ. 1995;310:1567–70.
Kilvington S. Acanthamoeba keratitis: the role of domestic tap water contamination in the United Kingdom. Investig Ophthalmol Vis Sci. 2004;45:165–9.
Maycock NJ, Jayaswal R. Update on Acanthamoeba keratitis: diagnosis, treatment, and outcomes. Cornea. 2016;35:713–20.
Seal DV. Acanthamoeba keratitis update—incidence, molecular epidemiology and new drugs for treatment. Eye. 2003;17:893.
Bacon AS, Dart JK, Ficker LA, Matheson MM, Wright P. Acanthamoeba keratitis. he value of early diagnosis. Ophthalmology. 1993;100:1238–43.
Watson ST, Dart JK. Acanthamoeba keratitis. In The epidemiology of eye disease. (Arnold, London, England, 2003). pp. 200–5.
Ku JY, Chan FM, Beckingsale P. Acanthamoeba keratitis cluster: an increase in Acanthamoeba keratitis in Australia. Clin Exp Ophthalmol. 2009;37:181–90.
Harris PA, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Robaei D, Carnt N, Minassian DC, Dart JKG. The impact of topical corticosteroid use before diagnosis on the outcome of acanthamoeba keratitis. Ophthalmology. 2014;121:1383–8.
Lee P, Green WR. Corneal biopsy. Indications, techniques, and a report of a series of 87 cases. Ophthalmology. 1990;97:718–21.
Li S-M, et al. Efficacy, safety and acceptability of orthokeratology on slowing axial elongation in myopic children by meta-analysis. Curr Eye Res. 2016;41:600–8.
Van Meter WS, et al. Safety of overnight orthokeratology for myopia. Ophthalmology. 2008;115:2301–.e1.
Tran T, Samarawickrama C, Petsoglou C, Watson S. Recent cluster of childhood microbial keratitis due to orthokeratology. Clin Exp Ophthalmol. 2014;42:793–4.
Joslin CE, et al. The association of contact lens solution use and Acanthamoeba keratitis. Am J Ophthalmol. 2007;144:169–.e2.
Efron N, Nichols JJ, Woods CA, Morgan PB. Trends in US contact lens prescribing 2002 to 2014. Optom Vis Sci. 2015;92:758–67.
Sharma S, Garg P, Rao GN. Patient characteristics, diagnosis, and treatment of non-contact lens related Acanthamoeba keratitis. Br J Ophthalmol. 2000;84:1103–8.
Keay L, Edwards K, Stapleton F. Referral pathways and management of contact lens-related microbial keratitis in Australia and New Zealand. Clin Exp Ophthalmol. 2008;36:209–16.
Miserocchi E, Fogliato G, Bianchi I, Bandello F, Modorati G. Clinical features of ocular herpetic infection in an Italian referral center. Cornea. 2014;33:565–70.
Mathers WD, Goldberg MA, Sutphin JE, Ditkoff JW, Folberg R. Coexistent Acanthamoeba keratitis and herpetic keratitis. Arch Ophthalmol Chic Ill 1960. 1997;115:714–8.
Robaei D, Carnt N, Minassian DC, Dart JKG. Therapeutic and optical keratoplasty in the management of Acanthamoeba keratitis. Ophthalmology. 2015;122:17–24.
Kelley PS. et al. Secondary glaucoma associated with advanced acanthamoeba keratitis. Eye Contact Lens. 2006;32:178–82.
Acknowledgements
The Sydney Eye Hospital Foundation and the Sydney Eye Hospital Pharmacy provided assistance. Prof. SLW was supported by a National Health and Medical Research Career Development Fellowship (APP1050524) and a Sydney Medical School Foundation Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Höllhumer, R., Keay, L. & Watson, S.L. Acanthamoeba keratitis in Australia: demographics, associated factors, presentation and outcomes: a 15-year case review. Eye 34, 725–732 (2020). https://doi.org/10.1038/s41433-019-0589-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0589-6
This article is cited by
-
Update on the Management of Acanthamoeba Keratitis
Current Ophthalmology Reports (2022)