Abstract
Objective
This systematic review aimed to evaluate the influence of the nature of diet (vegan, vegetarian, and omnivore) on the oral health status in adults.
Methods
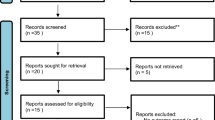
This systematic review and meta-analysis was performed using the PRISMA guidelines. Electronic databases [PubMed, Embase, CENTRAL], online search engines (Google Scholar), research portals, and hand searches were performed systematically to identify studies. The last literature search was performed February 1st, 2021. Studies were included if they reported on the influence of the nature of diet on the oral health status (oral hygiene, periodontal health, dental status, and salivary function) in adults, by two investigators. Inter-investigator reliability was evaluated using Kappa (κ) statistics. PROSPERO registration number: CRD42020211567.
Results
Twenty-two studies were included for data extraction and final analysis. The meta-analysis revealed that the bleeding on probing measure was higher in omnivores (Z = −4.057, p < 0.0001; 95% CI: −0.684, −0.238; I2 = 0.0%) and the overall periodontal health was significantly better in vegan/vegetarians than omnivores (Z = −2.632, p = 0.008; 95% CI: −0.274, −0.073; I2 = 29.7%). Vegan/vegetarians demonstrated more dental erosion (Z = 3.325, p = 0.001; 95% CI: 0.170, 0.659; I2 = 0.0%). In adults over 60 years old, the prevalence of caries was higher in omnivores (Z = 3.244, p = 0.001; 95% CI: 0.092, 0.371; I2 = 0.0%), while complete edentulism was more prevalent in vegetarians (Z = −4.147, p < 0.0001; 95% CI: −0.550, −0.197; I2 = 0.0%).
Conclusions
This review reveals that adults on an omnivore diet may be associated with a higher risk for periodontal problems and dental caries, while vegetarians/vegans may be associated with a higher risk for dental erosion.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
All the data extracted and analyzed are presented in the manuscript, further information can be made available on request in writing.
References
World Health Organization. Noncommunicable diseases. Key Facts. 2021. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
Bouvard V, Loomis D, Guyton KZ, Grosse Y, Ghissassi FE, Benbrahim-Tallaa L, et al. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015;16:1599–600. https://doi.org/10.1016/S1470-2045(15)00444-1.
World Health Organization. IARC monographs evaluate consumption of red meat and processed meat. 2015. https://www.iarc.who.int/wp-content/uploads/2018/07/pr240_E.pdf.
Abid Z, Cross AJ, Sinha R. Meat, dairy, and cancer. Am J Clin Nutr. 2014;100:386S–93S. https://doi.org/10.3945/ajcn.113.071597.
Kroenke CH, Kwan ML, Sweeney C, Castillo A, Caan BJ. High- and low-fat dairy intake, recurrence, and mortality after breast cancer diagnosis. J Natl Cancer Inst. 2013;105:616–23. https://doi.org/10.1093/jnci/djt027.
zur Hausen H, de Villiers EM. Dairy cattle serum and milk factors contributing to the risk of colon and breast cancers. Int J Cancer. 2015;137:959–67. https://doi.org/10.1002/ijc.29466.
Sargsyan A, Dubasi HB. Milk consumption and prostate cancer: a systematic review. World J Mens Health. 2021;39:419–28. https://doi.org/10.5534/wjmh.200051.
Aune D, Navarro Rosenblatt DA, Chan DS, Vieira AR, Vieira R, Greenwood DC, et al. Dairy products, calcium, and prostate cancer risk: a systematic review and meta-analysis of cohort studies. Am J Clin Nutr. 2015;101:87–117. https://doi.org/10.3945/ajcn.113.067157.
Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Willett WC, et al. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr. 2011;94:1088–96. https://doi.org/10.3945/ajcn.111.018978.
Micha R, Michas G, Mozaffarian D. Unprocessed red and processed meats and risk of coronary artery disease and type 2 diabetes-an updated review of the evidence. Curr Atheroscler Rep. 2012;14:515–24. https://doi.org/10.1007/s11883-012-0282-8.
Schwingshackl L, Hoffmann G, Lampousi AM, Knüppel S, Iqbal K, Schwedhelm C, et al. Food groups and risk of type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol. 2017;32:363–75. https://doi.org/10.1007/s10654-017-0246-y.
Barnard N, Levin S, Trapp C. Meat consumption as a risk factor for type 2 diabetes. Nutrients. 2014;6:897–910. https://doi.org/10.3390/nu6020897.
Malekinejad H, Rezabakhsh A. Hormones in dairy foods and their impact on public health—a narrative review article. Iran J Public Health. 2015;44:742–58.
Tuso PJ, Ismail MH, Ha BP, Bartolotto C. Nutritional update for physicians: plant-based diets. Perm J. 2013;17:61–6. https://doi.org/10.7812/tpp/12-085.
Medawar E, Huhn S, Villringer A, Veronica Witte A. The effects of plant-based diets on the body and the brain: a systematic review. Transl Psychiatry. 2019;9:226. https://doi.org/10.1038/s41398-019-0552-0.
World Health Organization. Regional Office for Europe Plant-based diets and their impact on health, sustainability and the environment: a review of the evidence: WHO European Office for the Prevention and Control of Noncommunicable Diseases. World Health Organization. Regional Office for Europe; 2021.
Ruby MB. Vegetarianism. A blossoming field of study. Appetite. 2012;58:141–50. https://doi.org/10.1016/j.appet.2011.09.019.
Preece R. Sins of the flesh: a history of ethical vegetarian thought. 2029 West Mall, Vancouver, BC V6T 1Z2 604-822-5959, Canada: UBC Press; 2009.
Leitzmann C. Vegetarian nutrition: past, present, future. Am J Clin Nutr. 2014;100:496s–502s. https://doi.org/10.3945/ajcn.113.071365.
Marrone G, Guerriero C, Palazzetti D, Lido P, Marolla A, Di Daniele F, et al. Vegan diet health benefits in metabolic syndrome. Nutrients. 2021;13:817. https://doi.org/10.3390/nu13030817.
Alwarith J, Kahleova H, Crosby L, Brooks A, Brandon L, Levin SM, et al. The role of nutrition in asthma prevention and treatment. Nutr Rev. 2020;78:928–38. https://doi.org/10.1093/nutrit/nuaa005.
McMacken M, Shah S. A plant-based diet for the prevention and treatment of type 2 diabetes. J Geriatr Cardiol. 2017;14:342–54. https://doi.org/10.11909/j.issn.1671-5411.2017.05.009.
Joshi S, Hashmi S, Shah S, Kalantar-Zadeh K. Plant-based diets for prevention and management of chronic kidney disease. Curr Opin Nephrol Hypertens. 2020;29:16–21. https://doi.org/10.1097/mnh.0000000000000574.
Craig WJ. Health effects of vegan diets. Am J Clin Nutr. 2009;89:1627s–33s. https://doi.org/10.3945/ajcn.2009.26736N.
Dinu M, Abbate R, Gensini GF, Casini A, Sofi F. Vegetarian, vegan diets and multiple health outcomes: a systematic review with meta-analysis of observational studies. Crit Rev Food Sci Nutr. 2017;57:3640–9. https://doi.org/10.1080/10408398.2016.1138447.
Haghighatdoost F, Bellissimo N, Totosy de Zepetnek JO, Rouhani MH. Association of vegetarian diet with inflammatory biomarkers: a systematic review and meta-analysis of observational studies. Public Health Nutr. 2017;20:2713–21. https://doi.org/10.1017/s1368980017001768.
Sakkas H, Bozidis P, Touzios C, Kolios D, Athanasiou G, Athanasopoulou E, et al. Nutritional status and the influence of the vegan diet on the gut microbiota and human health. Medicina. 2020;56:88 https://doi.org/10.3390/medicina56020088.
Smits KPJ, Listl S, Jevdjevic M. Vegetarian diet and its possible influence on dental health: a systematic literature review. Community Dent Oral Epidemiol. 2020;48:7–13. https://doi.org/10.1111/cdoe.12498.
Linkosalo E. Dietary habits and dental health in Finnish Seventh-Day Adventists. Proc Finn Dent Soc. 1988;84:109–15.
Atarbashi-Moghadam F, Moallemi-Pour S, Atarbashi-Moghadam S, Sijanivandi S, Baghban AA. Effects of raw vegan diet on periodontal and dental parameters. Tzu Chi Med J. 2020;32:357–61. https://doi.org/10.4103/tcmj.tcmj_161_19.
Linkosalo E, Markkanen H. Dental erosions in relation to lactovegetarian diet. Scand J Dent Res. 1985;93:436–41. https://doi.org/10.1111/j.1600-0722.1985.tb01336.x.
Pedrao AMN, Andrews Portes L, Padilha Gomes E, Figueira Teixeira FC, da Costa Pereira A, de Oliveira NC. Erosive tooth wear and dietary patterns: a clinical study. Oral Health Prev Dent. 2018;16:145–51. https://doi.org/10.3290/j.ohpd.a40321.
Staufenbiel I, Adam K, Deac A, Geurtsen W, Gunay H. Influence of fruit consumption and fluoride application on the prevalence of caries and erosion in vegetarians-a controlled clinical trial. Eur J Clin Nutr. 2015;69:1156–60. https://doi.org/10.1038/ejcn.2015.20.
Staufenbiel I, Weinspach K, Forster G, Geurtsen W, Gunay H. Periodontal conditions in vegetarians: a clinical study. Eur J Clin Nutr. 2013;67:836–40. https://doi.org/10.1038/ejcn.2013.101.
De Filippis F, Vannini L, La Storia A, Laghi L, Piombino P, Stellato G, et al. The same microbiota and a potentially discriminant metabolome in the saliva of omnivore, ovo-lacto-vegetarian and Vegan individuals. PLoS ONE. 2014;9:e112373. https://doi.org/10.1371/journal.pone.0112373.
Kumar HA, Shetty NJ. Correlation between type of diet and periodontal parameters. Indian J Public Health Res Dev. 2018;9:195–200. https://doi.org/10.5958/0976-5506.2018.01832.6.
Johansson G, Widerstrom L. Change from mixed diet to lactovegetarian diet: influence on IgA levels in blood and saliva. Scand J Dent Res. 1994;102:350–4. https://doi.org/10.1111/j.1600-0722.1994.tb01482.x.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2022. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Sterne JAC, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. 2001. https://www.sciencedirect.com/science/article/pii/S0895435601003778.
Zotti F, Laffranchi L, Fontana P, Dalessandri D, Bonetti S. Effects of fluorotherapy on oral changes caused by a vegan diet. Minerva Stomatol. 2014;63:179–88.
Mapare SA, Rao PK, Reddy RV, Kumar MM, Gorthi VC, Raju PK. A comparative clinical evaluation of diet intake and effect of various nutritions on aggressive periodontitis patients. J Contemp Dent Pract. 2013;14:930–8. https://doi.org/10.5005/jp-journals-10024-1428.
Bartlett DW, Fares J, Shirodaria S, Chiu K, Ahmad N, Sherriff M. The association of tooth wear, diet and dietary habits in adults aged 18-30 years old. J Dent. 2011;39:811–6. https://doi.org/10.1016/j.jdent.2011.08.014.
Liuliakina EG, Kukhaskaia LK, Salmina AB, Shishlov PA. [Biochemical indices of lactovegetarians’ saliva]. Stomatologiia (Mosk). 2009;88:41–4.
Shah N, Sundaram KR. Impact of socio-demographic variables, oral hygiene practices, oral habits and diet on dental caries experience of Indian elderly: a community-based study. Gerodontology. 2004;21:43–50. https://doi.org/10.1111/j.1741-2358.2004.00010.x.
Ganss C, Schlechtriemen M, Klimek J. Dental erosions in subjects living on a raw food diet. Caries Res. 1999;33:74–80. https://doi.org/10.1159/000016498.
Sherfudhin H, Abdullah A, Shaik H, Johansson A. Some aspects of dental health in young adult Indian vegetarians. A pilot study. Acta Odontol Scand. 1996;54:44–8. https://doi.org/10.3109/00016359609003508.
Linkosalo E, Ohtonen S, Markkanen H, Karinpaa A, Kumpusalo E. Caries, periodontal status and some salivary factors in lactovegetarians. Scand J Dent Res. 1985;93:304–8. https://doi.org/10.1111/j.1600-0722.1985.tb01973.x.
Linkosalo E, Markkanen H, Syrjanen S. Effects of a lacto-ovo-vegetarian diet on the free amino acid composition of wax-stimulated whole human saliva. J Nutr. 1985;115:588–92. https://doi.org/10.1093/jn/115.5.588.
Linkosalo E. Lactovegetarian diet and dental health. Proc Finn Dent Soc. 1988;84:1–77.
Linkosalo E, Syrjanen S, Alakuijala P. Salivary composition and dental erosions in lacto-ovo-vegetarians. Proc Finn Dent Soc. 1988;84:253–60.
Krishna M, Hegde MN, Shetty A, Shetty N. Prevalence of tooth wear due to dietary factors in population of South Karnataka, India. Res J Pharm Biol Chem Sci. 2019;10:1413–7.
Manaf ZA, Lee MT, Ali NH, Samynathan S, Jie YP, Ismail NH, et al. Relationship between food habits and tooth erosion occurrence in Malaysian University students. Malays J Med Sci. 2012;19:56–66.
Walti A, Lussi A, Seemann R. The effect of a chewing-intensive, high-fiber diet on oral halitosis: a clinical controlled study. Swiss Dent J. 2016;126:782–95.
Bartlett DW, Lussi A, West NX, Bouchard P, Sanz M, Bourgeois D. Prevalence of tooth wear on buccal and lingual surfaces and possible risk factors in young European adults. J Dent. 2013;41:1007–13. https://doi.org/10.1016/j.jdent.2013.08.018.
Belstrøm D, Holmstrup P, Nielsen CH, Kirkby N, Twetman S, Heitmann BL, et al. Bacterial profiles of saliva in relation to diet, lifestyle factors, and socioeconomic status. J Oral Microbiol. 2014;6. https://doi.org/10.3402/jom.v6.23609.
Kavitha D, Varghese A, Prabath S, Sreeram R, Asha J, Ravi AB. Prevalence of dental caries in adult South Indian population in association with dietary pattern: a comparative study. J Pharm Bioallied Sci. 2020;12:S546–9. https://doi.org/10.4103/jpbs.JPBS_155_20.
Değirmenci A, Ünalan Değirmenci B. How do the diet, oral hygiene habits and body mass index affect tooth caries in the students of the faculty of dentistry. Eastern J Med. 2020;25:225–33. https://doi.org/10.5505/ejm.2020.15046.
Tinker L, Millen A, Wactawski‐Wende J, Pettinger M, Sarto G, Vitolins M, et al. Association of diet quality score with periodontal disease in postmenopausal women: evidence from the Women’s Health Initiative Observational Study (WHI-OS). FASEB J. 2013;27:245.2–245.2. https://doi.org/10.1096/fasebj.27.1_supplement.245.2.
Milledge K, Cumming R, Wright F, et al. Dietary intake of nutrients and compromised periodontal health: the concord health and ageing men project. Ann Nutr Metab. 2017;71:359–60. https://doi.org/10.1159/000480486.
NCT. Impact of dietary advice on the progression of tooth wear. 2015. https://clinicaltrials.gov/show/NCT02493803.
West NX, Sanz M, Lussi A, Bartlett D, Bouchard P, Bourgeois D. Prevalence of dentine hypersensitivity and study of associated factors: a European population-based cross-sectional study. J Dent. 2013;41:841–51. https://doi.org/10.1016/j.jdent.2013.07.017.
Herman K, Czajczynska-Waszkiewicz A, Kowalczyk-Zajac M, Dobrzynski M. Assessment of the influence of vegetarian diet on the occurrence of erosive and abrasive cavities in hard tooth tissues. Postepy Hig Med Dosw. 2011;65:764–9. https://doi.org/10.5604/17322693.967066.
Kumar M, Verma R, Bansal M, Singh S, Rehan S, Kumar V, et al. To evaluate the severity, distribution of occlusal tooth wear and its correlation with bite force in young North Indian adults. Open Dent J. 2018;12:735–41. https://doi.org/10.2174/1745017901814010735.
Laffranchi L, Zotti F, Bonetti S, Dalessandri D, Fontana P. Oral implications of the vegan diet: observational study. Minerva Stomatol. 2010;59:583–91.
Rafeek RN, Marchan S, Eder A, Smith WA. Tooth surface loss in adult subjects attending a university dental clinic in Trinidad. Int Dent J. 2006;56:181–6. https://doi.org/10.1111/j.1875-595x.2006.tb00092.x.
Shah N, Parkash H, Sunderam KR. Edentulousness, denture wear and denture needs of Indian elderly—a community-based study. J Oral Rehabil. 2004;31:467–76. https://doi.org/10.1111/j.1365-2842.2004.01260.x.
Smith WA, Marchan S, Rafeek RN. The prevalence and severity of non-carious cervical lesions in a group of patients attending a university hospital in Trinidad. J Oral Rehabil. 2008;35:128–34. https://doi.org/10.1111/j.1365-2842.2007.01763.x.
Hou XM, Zhang Q, Gao XJ, Wang JS. [Pilot study of dental erosion and associated factors in university student volunteers]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2005;40:478–80.
Mazur M, Bietolini S, Bellardini D, Lussi A, Corridore D, Maruotti A, et al. Oral health in a cohort of individuals on a plant-based diet: a pilot study. Clin Ter. 2020;171:e142–8. https://doi.org/10.7417/CT.2020.2204.
Booth J, Hurry J. The impact of a vegan diet on oral health and the role of the GDP. BDJ In Practice. 2020;33:20–1. https://doi.org/10.1038/s41404-020-0385-9.
Hansen TH, Kern T, Bak EG, Kashani A, Allin KH, Nielsen T, et al. Impact of a vegan diet on the human salivary microbiota. Sci Rep. 2018;8:5847. https://doi.org/10.1038/s41598-018-24207-3.
Bridges G. The vegan dental patient. Dent Nurs. 2016;12:452–3. https://doi.org/10.12968/denn.2016.12.8.452.
Johansson G, Birkhed D. Effect of a long-term change from a mixed to a lactovegetarian diet on human saliva. Arch Oral Biol. 1994;39:283–8. https://doi.org/10.1016/0003-9969(94)90118-x.
Muralidharan NP, Swathy S. Salivary pH as a factor in oral health and its correlation with diet. Indian J Public Health Res Dev. 2019;10:554–8.
Woelber JP, Gärtner M, Breuninger L, Anderson A, König D, Hellwig E, et al. The influence of an anti-inflammatory diet on gingivitis. A randomized controlled trial. J Clin Periodontol. 2019;46:481–90. https://doi.org/10.1111/jcpe.13094.
Devanathan N, Hegde MN, Shetty S, Sadananda V. Prevalence of tooth wear due to dietary factors in population of South Karnataka. EJBPS. 2018;5:616–9.
Khan AA, Jain SK, Shrivastav A. Prevalence of dental caries among the population of Gwalior (India) in relation of different associated factors. Eur J Dent. 2008;2:81–85.
Wade WG. The oral microbiome in health and disease. Pharmacol Res. 2013;69:137–43. https://doi.org/10.1016/j.phrs.2012.11.006.
Vollaard EJ, Clasener HA. Colonization resistance. Antimicrob Agents Chemother. 1994;38:409–14. https://doi.org/10.1128/AAC.38.3.409.
Rosan B, Lamont RJ. Dental plaque formation. Microbes Infect. 2000;2:1599–607. https://doi.org/10.1016/s1286-4579(00)01316-2.
Coventry J, Griffiths G, Scully C, Tonetti M. ABC of oral health: periodontal disease. BMJ. 2000;321:36–9. https://doi.org/10.1136/bmj.321.7252.36.
World Health Organization. Oral Health. Key facts. 2020. https://www.who.int/news-room/fact-sheets/detail/oral-health.
Moynihan P, Petersen PE. Diet, nutrition and the prevention of dental diseases. Public Health Nutr. 2004;7:201–26. https://doi.org/10.1079/phn2003589.
Santonocito S, Polizzi A, Palazzo G, Indelicato F, Isola G. Dietary factors affecting the prevalence and impact of periodontal disease. Clin Cosmet Investig Dent. 2021;13:283–92. https://doi.org/10.2147/CCIDE.S288137.
Orlich MJ, Jaceldo-Siegl K, Sabate J, Fan J, Singh PN, Fraser GE. Patterns of food consumption among vegetarians and non-vegetarians. Br J Nutr. 2014;112:1644–53. https://doi.org/10.1017/S000711451400261X.
Preshaw PM, Alba AL, Herrera D, Jepsen S, Konstantinidis A, Makrilakis K, et al. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012;55:21–31. https://doi.org/10.1007/s00125-011-2342-y.
Larvin H, Kang J, Aggarwal VR, Pavitt S, Wu J. Risk of incident cardiovascular disease in people with periodontal disease: a systematic review and meta-analysis. Clin Exp Dent Res. 2021;7:109–22. https://doi.org/10.1002/cre2.336.
Wang W, Yang Z, Wang Y, Gao H, Wang Y, Zhang Q. Association between periodontitis and carotid artery calcification: a systematic review and meta-analysis. Biomed Res Int. 2021;2021:3278351. https://doi.org/10.1155/2021/3278351.
Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol. 2018;89:S159–72. https://doi.org/10.1002/JPER.18-0006.
World Health Organization. Sugars and dental caries. 2017. https://apps.who.int/iris/bitstream/handle/10665/259413/WHO-NMH-NHD-17.12-eng.pdf.
Moynihan PJ. Dietary advice in dental practice. Br Dent J. 2002;193:563–8. https://doi.org/10.1038/sj.bdj.4801628.
Lussi A, Jaeggi T, Zero D. The role of diet in the aetiology of dental erosion. Caries Res. 2004;38:34–44. https://doi.org/10.1159/000074360.
Lussi A, Schlueter N, Rakhmatullina E, Ganss C. Dental erosion-an overview with emphasis on chemical and histopathological aspects. Caries Res. 2011;45:2–12. https://doi.org/10.1159/000325915.
Schlueter N, Luka B. Erosive tooth wear—a review on global prevalence and on its prevalence in risk groups. Br Dent J. 2018;224:364–70. https://doi.org/10.1038/sj.bdj.2018.167.
Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NH. Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes. 2010;8:126. https://doi.org/10.1186/1477-7525-8-126.
Allès B, Baudry J, Méjean C, Touvier M, Péneau S, Hercberg S, et al. Comparison of sociodemographic and nutritional characteristics between self-reported vegetarians, vegans, and meat-eaters from the NutriNet-Santé study. Nutrients. 2017;9:1023.
Davey GK, Spencer EA, Appleby PN, Allen NE, Knox KH, Key TJ. EPIC-Oxford: lifestyle characteristics and nutrient intakes in a cohort of 33 883 meat-eaters and 31 546 non meat-eaters in the UK. Public Health Nutr. 2003;6:259–69. https://doi.org/10.1079/PHN2002430.
Glenny AM, Nieri M, Worthington H, Espostio M. The importance of the study design: from the case report to the randomised controlled clinical trial. Eur J Oral Implantol. 2008;1:317–21.
Acknowledgements
The authors wish to thank Mrs. Elena van der Heijden from the Clinic of General, Special Care and Geriatric Dentistry for her help in translating and guidance with studies published in Russian language.
Funding
None.
Author information
Authors and Affiliations
Contributions
LGA designed research, conducted research, provided essential materials, analyzed data, wrote paper, read, and approved the final manuscript. NF conducted research, provided essential materials, analyzed data, read, and approved the final manuscript. MS designed research, provided essential materials, analyzed data, performed statistical analysis, had primary responsibility for final content, read and approved the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Azzola, L.G., Fankhauser, N. & Srinivasan, M. Influence of the vegan, vegetarian and omnivore diet on the oral health status in adults: a systematic review and meta-analysis. Evid Based Dent 24, 43–44 (2023). https://doi.org/10.1038/s41432-023-00853-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41432-023-00853-z