Abstract
Objectives
The standard treatment for short bowel syndrome is home parenteral nutrition. Patients’ strict adherence to protocols is essential to decrease the risk of complications such as infection or catheter thrombosis. Patient training can even result in complete autonomy in daily care. However, some patients cannot or do not want too much responsibility. However, doctors often encourage them to acquire these skills. Based on qualitative investigations with patients, we wanted to document issues of importance concerning perceptions of autonomy in daily care.
Methods
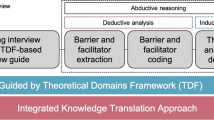
Semistructured interviews were conducted with 13 adult patients treated by home parenteral nutrition using a maximum variation sampling strategy. We proceeded to a thematic analysis following an inductive approach.
Results
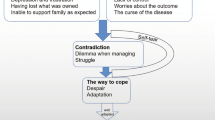
After achieving clinical management of symptoms, a good quality of life is within the realm of possibility for short bowel syndrome patients with home parenteral nutrition. In this context, achieving autonomy in home parenteral nutrition could be a lever to sustain patients’ quality of life by providing better life control. However, counterintuitively, not all patients aim at reducing constraints by reaching autonomy in home parenteral nutrition. First, they appreciate the social contact with the nurses, which is particularly true among patients who live alone. Second, they can feel safer with the nurse’s visits. Regaining freedom was the main motivation for patients in the training program and the main benefit for those who were already autonomous.
Conclusions
Medical teams should consider patients’ health locus of control (internal or external) for disease management to support them concerning the choice of autonomy in daily care for parenteral nutrition.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The data that support the findings are available on request from the authors.
References
Jeppesen PB. Spectrum of short bowel syndrome in adults. J Parenter Enter Nutr. 2014;38:8S–13S.
von Websky MW, Liermann U, Buchholz BM, Kitamura K, Pascher A, Lamprecht G, et al. Short bowel syndrome in Germany. Estimated prevalence and standard of care. Chirurg. 2014;85:433–9.
Billiauws L, Maggiori L, Joly F, Panis Y. Medical and surgical management of short bowel syndrome. J Visc Surg. 2018;155:283–91.
Siddiqui MT, Al-Yaman W, Singh A, Kirby DF. Short-bowel syndrome: epidemiology, hospitalization trends, in-hospital mortality, and healthcare utilization. J Parenter Enter Nutr. 2021;45:1441–55.
Sowerbutts AM, Panter C, Dickie G, Bennett B, Ablett J, Burden S, et al. Short bowel syndrome and the impact on patients and their families: a qualitative study. J Hum Nutr Diet. 2020;33:767–74.
Carlsson E, Berglund B, Nordgren S. Living with an ostomy and short bowel syndrome: practical aspects and impact on daily life. J Wound Ostomy Cont Nurs. 2001;28:96–105.
Silver HJ. The lived experience of home total parenteral nutrition: an online qualitative inquiry with adults, children, and mothers. Nutr Clin Pr. 2004;19:297–304.
Winkler MF, Hagan E, Wetle T, Smith C, Maillet JO, Touger-Decker R. An exploration of quality of life and the experience of living with home parenteral nutrition. JPEN J Parenter Enter Nutr. 2010;34:395–407.
Heaney A, McKenna SP, Wilburn J, Rouse M, Taylor M, Burden S, et al. The impact of Home Parenteral Nutrition on the lives of adults with Type 3 intestinal failure. Clin Nutr ESPEN. 2018;24:35–40.
Harris C, Scolapio JS. Initial evaluation and care of the patient with new-onset intestinal failure. Gastroenterol Clin North Am. 2019;48:465–70.
Saqui O, Fernandes G, Allard J. Central venous catheter infection in Canadian home parenteral nutrition patients: a 5-year multicenter retrospective study. Br J Nurs. 2020;29:S34–42.
Kumpf VJ. Challenges and obstacles of long-term home parenteral nutrition. Nutr Clin Pr. 2019;34:196–203.
Messing B, Joly F. Guidelines for management of home parenteral support in adult chronic intestinal failure patients. Gastroenterology. 2006;130:S43–51.
Bond A, Teubner A, Taylor M, Cawley C, Abraham A, Dibb M, et al. Assessing the impact of quality improvement measures on catheter related blood stream infections and catheter salvage: Experience from a national intestinal failure unit. Clin Nutr. 2018;37:2097–101.
Joly F, Boehm V, Bataille J, Billiauws L, Corcos O. Parcours de soins du patient adulte souffrant de syndrome de grêle court avec insuffisance intestinale. Nutr Clin et Métabolisme. 2016;30:385–98.
Beurskens-Meijerink J, Huisman-de Waal G, Wanten G. Evaluation of quality of life and caregiver burden in home parenteral nutrition patients: A cross sectional study. Clin Nutr ESPEN. 2020;37:50–7.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57.
Ames H, Glenton C, Lewin S. Purposive sampling in a qualitative evidence synthesis: a worked example from a synthesis on parental perceptions of vaccination communication. BMC Med Res Methodol. 2019;19:26.
Marshall B, Cardon P, Poddar A, Fontenot R. Does Sample size matter in qualitative research?: A review of qualitative interviews in is research. J Comp Inf Syst. 2013;54:11–22.
Mason M Sample Size and Saturation in PhD Studies Using Qualitative Interviews. FQS [Internet]. 24 août 2010 [cité 4 mai 2021];11. Disponible sur: https://www.qualitative-research.net/index.php/fqs/article/view/1428.
Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15:398–405.
McDonald N, Schoenebeck S, Forte A. Reliability and inter-rater reliability in qualitative research: norms and guidelines for CSCW and HCI practice. Proc ACM Hum-Comput Interact. 2019;3:72:1–72:23.
Carter N, Bryant-Lukosius D, DiCenso A, Blythe J, Neville AJ. The use of triangulation in qualitative research. Oncol Nurs Forum. 2014;41:545–7.
Nordsten CB, Molsted S, Bangsgaard L, Fuglsang KA, Brandt CF, Niemann MJ, et al. High parenteral support volume is associated with reduced quality of life determined by the short-bowel syndrome quality of life scale in nonmalignant intestinal failure patients. JPEN J Parenter Enter Nutr. 2021;45:926–32.
Jeppesen PB, Shahraz S, Hopkins T, Worsfold A, Genestin E. Impact of intestinal failure and parenteral support on adult patients with short-bowel syndrome: A multinational, noninterventional, cross-sectional survey. JPEN J Parenter Enter Nutr. 2022;46:1650–9.
Parrish CR, DiBaise JK. Managing the adult patient with short bowel syndrome. Gastroenterol Hepatol (N. Y). 2017;13:600–8.
Ricci L, Villegente J, Loyal D, Ayav C, Kivits J, Rat AC. Tailored patient therapeutic educational interventions: A patient centred communication model. Health Expect. 2021;25:276–289.
Nazareth M, Richards J, Javalkar K, Haberman C, Zhong Y, Rak E, et al. Relating health locus of control to health care use, adherence, and transition readiness among youths with chronic conditions, North Carolina, 2015. Prev Chronic Dis. 2016;13:E93.
Marton G, Pizzoli SFM, Vergani L, Mazzocco K, Monzani D, Bailo L, et al. Patients’ health locus of control and preferences about the role that they want to play in the medical decision-making process. Psychol Health Med. 2021;26:260–6.
Russo S, Jongerius C, Faccio F, Pizzoli SFM, Pinto CA, Veldwijk J, et al. Understanding patients’ preferences: a systematic review of psychological instruments used in patients’ preference and decision studies. Value Health. 2019;22:491–501.
Polit DF, Beck CT. Generalization in quantitative and qualitative research: Myths and strategies. Int J Nurs Stud. 2010;47:1451–8.
Galdas P. Revisiting bias in qualitative research: reflections on its relationship with funding and impact. Int J Qual Methods. 2017;16:1609406917748992.
Morse JM, Barrett M, Mayan M, Olson K, Spiers J. Verification strategies for establishing reliability and validity in qualitative research. Int J Qual Methods. 2008;1:13–22.
Singh GK, Daus GP, Allender M, Ramey CT, Martin EK, Perry C, et al. Social determinants of health in the united states: addressing major health inequality trends for the nation, 1935–2016. Int J MCH AIDS. 2017;6:139–64.
Arcaya MC, Arcaya AL, Subramanian SV. Inequalities in health: definitions, concepts, and theories. Glob Health Action. 2015;8:27106.
Massironi S, Cavalcoli F, Rausa E, Invernizzi P, Braga M, Vecchi M. Understanding short bowel syndrome: current status and future perspectives. Dig Liver Dis. 2020;52:253–61.
Acknowledgements
We thank Justine Krier and Martin Clement Sonia –RN- for their help in the recruitment process. We acknowledge the work of Emilie Culminique and Sandrine GrandClere for contributing to transcription and the contribution of Yacine Haroun in encoding the data. We also thank Marjorie Starck for her help in administrative management of the project.
Funding
LR received a Baxter award delivered under the auspices of la Société Francophone de Nutrition Clinique et Métabolisme (2018).
Author information
Authors and Affiliations
Contributions
LR, FJ and FG contributed to the conception and design of the research. LR, AC and DQ contributed to the acquisition of data. LR, FJ and DQ helped interpret the data. LR wrote the original draft. All authors critically revised the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The Comité de Protection des Personnes (CPP (Sud-Ouest et Outre-Mer III)) approved the protocol (no. ID‐RCB: 2019‐A0203453‐46). All participants gave their oral consent and received an information and opposition form.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ricci, L., Joly, F., Coly, A. et al. Important issues in proposing autonomy training in home parenteral nutrition for short bowel syndrome patients: a qualitative insight from the patients’ perspectives. Eur J Clin Nutr (2024). https://doi.org/10.1038/s41430-024-01415-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41430-024-01415-x