Abstract
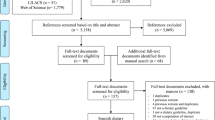
A dramatic shift in the global food system is occurring with the rapid growth of ultra-processed foods (UPFs) consumption, which poses potentially serious health risks. Systematic review (SR) method has been used to summarise the association between UPF consumption and multiple health outcomes; however, a suboptimal-quality SR may mislead the decision-making in clinical practices and health policies. Therefore, a methodological review was conducted to identify the areas that can be improved regarding the risk of bias and reporting quality of relevant SRs. Systematic searches to collect SRs with meta-analyses of UPFs were performed using four databases from their inception to April 14, 2023. The risk of bias and reporting quality were evaluated using ROBIS and PRISMA 2020, respectively. The key characteristics of the included SRs were summarised descriptively. Excel 2019 and R 4.2.3 were used to analyse the data and draw graphs. Finally, 16 relevant SRs written in English and published between 2020 and 2023 in 12 academic journals were included. Only one SR was rated as low risk of bias, and the others were rated as higher risk of bias mainly because the risk of bias in the original studies was not explicitly addressed when synthesising the evidence. The reporting was required to be advanced significantly, involving amendments of registration and protocol, data and analytic code statement, and lists of excluded studies with justifications. The reviews’ results could improve the quality, strengthen future relevant SRs’ robustness, and further underpin the evidence base for supporting clinical decisions and health policies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets used and analysed in the current methodological systematic review are presented in the text and appendix.
References
Popkin BM, Ng SW. The nutrition transition to a stage of high obesity and noncommunicable disease prevalence dominated by ultra-processed foods is not inevitable. Obes Rev. 2022;23:e13366.
Monteiro CA, Cannon G, Moubarac JC, Levy RB, Louzada MLC, Jaime PC. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018;21:5–17.
Srour B, Kordahi MC, Bonazzi E, Deschasaux-Tanguy M, Touvier M, Chassaing B. Ultra-processed foods and human health: from epidemiological evidence to mechanistic insights. Lancet Gastroenterol Hepatol. 2022;7:1128–40.
Zeraatkar D, Bhasin A, Morassut RE, Churchill I, Gupta A, Lawson DO, et al. Characteristics and quality of systematic reviews and meta-analyses of observational nutritional epidemiology: a cross-sectional study. Am J Clin Nutr. 2021;113:1578–92.
Le JT, Qureshi R, Twose C, Rosman L, Han G, Fapohunda K, et al. Evaluation of systematic reviews of interventions for retina and vitreous conditions. JAMA Ophthalmol. 2019;137:1399–405.
Murad MH, Montori VM, Ioannidis JP, Jaeschke R, Devereaux PJ, Prasad K, et al. How to read a systematic review and meta-analysis and apply the results to patient care: users’ guides to the medical literature. JAMA. 2014;312:171–9.
Ioannidis JP. The mass production of redundant, misleading, and conflicted systematic reviews and meta-analyses. Milbank Q. 2016;94:485–514.
Cronin P, Rawson JV, Heilbrun ME, Lee JM, Kelly AM, Sanelli PC, et al. How to critically appraise the clinical literature. Acad Radio. 2014;21:1117–28.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Bonetti AF, Tonin FS, Della Rocca AM, Lucchetta RC, Fernandez-Llimos F, Pontarolo R. Methodological quality and risk of bias of meta-analyses of pharmacy services: a systematic review. Res Soc Adm Pharm. 2022;18:2403–9.
Yuan L, Hu H, Li T, Zhang J, Feng Y, Yang X, et al. Dose-response meta-analysis of ultra-processed food with the risk of cardiovascular events and all-cause mortality: evidence from prospective cohort studies. Food Funct. 2023;14:2586–96.
Wang M, Du X, Huang W, Xu Y. Ultra-processed foods consumption increases the risk of hypertension in adults: a systematic review and meta-analysis. Am J Hypertens. 2022;35:892–901.
Taneri PE, Wehrli F, Roa-Díaz ZM, Itodo OA, Salvador D, Raeisi-Dehkordi H, et al. Association between ultra-processed food intake and all-cause mortality: a systematic review and meta-analysis. Am J Epidemiol. 2022;191:1323–35.
Narula N, Chang NH, Mohammad D, Wong ECL, Ananthakrishnan AN, Chan SSM, et al. Food processing and risk of inflammatory bowel disease: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2023;21:2483–e1.
Moradi S, Entezari MH, Mohammadi H, Jayedi A, Lazaridi AV, Kermani MAH, et al. Ultra-processed food consumption and adult obesity risk: a systematic review and dose-response meta-analysis. Crit Rev Food Sci Nutr. 2023;63:249–60.
Lu C, Ke L, Li J, Zhao H, Lu T, Mentis AFA, et al. Saffron (Crocus sativus L.) and health outcomes: a meta-research review of meta-analyses and an evidence mapping study. Phytomedicine. 2021;91:153699.
Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34.
Moradi S, Kermani MAH, Bagheri R, Mohammadi H, Jayedi A, Lane MM, et al. Ultra-processed food consumption and adult diabetes risk: a systematic review and dose-response meta-analysis. Nutrients. 2021;13:4410.
Askari M, Heshmati J, Shahinfar H, Tripathi N, Daneshzad E. Ultra-processed food and the risk of overweight and obesity: a systematic review and meta-analysis of observational studies. Int J Obes. 2020;44:2080–91.
Cascaes AM, Ribeiro Jorge Da Silva N, Dos Santos Fernandez M, Bomfim RA, Vaz JDS. Ultra-processed foods consumption and dental caries in children and adolescents: a systematic review and meta-Analysis. Br J Nutr. 2022;27:1–10.
Delpino FM, Figueiredo LM, Bielemann RM, Da Silva BGC, Dos Santos FS, Mintem GC, et al. Ultra-processed food and risk of type 2 diabetes: a systematic review and meta-analysis of longitudinal studies. Int J Epidemiol. 2022;51:1120–41.
Delpino FM, Figueiredo LM, Flores TR, Silveira EA, Silva Dos Santos F, Werneck AO, et al. Intake of ultra-processed foods and sleep-related outcomes: a systematic review and meta-analysis. Nutrition. 2022;106:111908.
Lane MM, Davis JA, Beattie S, Gómez-Donoso C, Loughman A, O’Neil A, et al. Ultraprocessed food and chronic noncommunicable diseases: a systematic review and meta-analysis of 43 observational studies. Obes Rev. 2021;22:e13146.
Lane MM, Gamage E, Travica N, Dissanayaka T, Ashtree DN, Gauci S, et al. Ultra‐processed food consumption and mental health: a systematic review and meta‐analysis of observational studies. Nutrients. 2022;14:2568.
Mazloomi SN, Talebi S, Mehrabani S, Bagheri R, Ghavami A, Zarpoosh M, et al. The association of ultra-processed food consumption with adult mental health disorders: a systematic review and dose-response meta-analysis of 260,385 participants. Nutr Neurosci. 2022;26:913–31.
Pagliai G, Dinu M, Madarena MP, Bonaccio M, Iacoviello L, Sofi F. Consumption of ultra-processed foods and health status: a systematic review and meta-analysis. Br J Nutr. 2021;125:308–18.
Paula WO, Patriota ESO, Gonçalves VSS, Pizato N. Maternal consumption of ultra-processed foods-rich diet and perinatal outcomes: a systematic review and meta-analysis. Nutrients. 2022;14:3242.
Suksatan W, Moradi S, Naeini F, Bagheri R, Mohammadi H, Talebi S, et al. Ultra‐processed food consumption and adult mortality risk: a systematic review and dose–response meta‐analysis of 207,291 participants. Nutrients. 2022;14:174.
Wang Z, Lu C, Cui L, Fenfen E, Shang W, Wang Z, et al. Consumption of ultra-processed foods and multiple health outcomes: an umbrella study of meta-analyses. Food Chem. 2023;434:137460.
Ioannidis JP, Greenland S, Hlatky MA, Khoury MJ, Macleod MR, Moher D, et al. Increasing value and reducing waste in research design, conduct, and analysis. Lancet. 2014;383:166–75.
Popkin BM, Barquera S, Corvalan C, Hofman KJ, Monteiro C, Ng SW, et al. Towards unified and impactful policies to reduce ultra-processed food consumption and promote healthier eating. Lancet Diabetes Endocrinol. 2021;9:462–70.
Adams J, Hofman K, Moubarac JC, Thow AM. Public health response to ultra-processed food and drinks. BMJ. 2020;369:m2391.
Pieper D, Rombey T. Where to prospectively register a systematic review. Syst Rev. 2022;11:8.
Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions version 6.3. 2022. www.training.cochrane.org/handbook.
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol. 2012;175:66–73.
Orsini N, Bellocco R, Greenland S. Generalized least squares for trend estimation of summarized dose–response data. Stata J. 2006;6:40–57.
Crippa A, Orsini N. Multivariate dose-response meta-analysis: the dosresmeta R package. J Stat Softw Code Snippets. 2016;72:1–15.
Schwingshackl L, Knüppel S, Schwedhelm C, Hoffmann G, Missbach B, Stelmach-Mardas M, et al. Perspective: NutriGrade: a scoring system to assess and judge the meta-evidence of randomized controlled trials and cohort studies in nutrition research. Adv Nutr. 2016;7:994–1004.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Katikireddi SV, Egan M, Petticrew M. How do systematic reviews incorporate risk of bias assessments into the synthesis of evidence? A methodological study. J Epidemiol Community Health. 2015;69:189–95.
Lindekilde N, Scheuer SH, Rutters F, Knudsen L, Lasgaard M, Rubin KH, et al. Prevalence of type 2 diabetes in psychiatric disorders: an umbrella review with meta-analysis of 245 observational studies from 32 systematic reviews. Diabetologia. 2022;65:440–56.
Dos Santos MBF, Agostini BA, Bassani R, Pereira GKR, Sarkis-Onofre R. Protocol registration improves reporting quality of systematic reviews in dentistry. BMC Med Res Methodol. 2020;20:57.
Page MJ, Nguyen PY, Hamilton DG, Haddaway NR, Kanukula R, Moher D, et al. Data and code availability statements in systematic reviews of interventions were often missing or inaccurate: a content analysis. J Clin Epidemiol. 2022;147:1–10.
Park HY, Suh CH, Woo S, Kim PH, Kim KW. Quality reporting of systematic review and meta-analysis according to PRISMA 2020 guidelines: results from recently published papers in the Korean Journal of Radiology. Korean J Radio. 2022;23:355–69.
Funding
This work was supported by the Major Program of the National Science Found of China “Research on the Theoretical System, International Experience and Chinese Path of Evidence-based Social Science” [Grant number: 19ZDA142] and A clinical comprehensive evaluation of traditional Chinese medicine in the treatment of hypertension [Grant number: 22JR5RA510]. The funder did not play any role in each process of this review.
Author information
Authors and Affiliations
Contributions
CL designed this study. ZW and YW performed the search. ZW and WS selected the literature. ZW and YW collected data. WS and WL rechecked data. ZW and CL assessed the quality. CL, ZW, YW, and WS performed analysis. ZW, CL, YW, and WS drafted the manuscript. XL, KY, WL, LC, JH, CL, ZC, and ZW revised the manuscript. All authors approved the final version of this manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Z., Wang, Y., Shang, W. et al. Reporting quality and risk of bias of systematic reviews of ultra-processed foods: a methodological study. Eur J Clin Nutr 78, 171–179 (2024). https://doi.org/10.1038/s41430-023-01383-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-023-01383-8