Abstract
Background
Metabolic dysfunction-associated fatty liver disease was proposed by international consensus to redefine the metabolic abnormal condition. However, its impact on liver transplant recipients with hepatitis B virus-related hepatocellular carcinoma has not been explored.
Methods
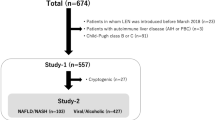
A two-center retrospective cohort study on liver transplant recipients with hepatitis B virus-related hepatocellular carcinoma was performed to analyze the impact of metabolic dysfunction-associated fatty liver disease on the clinicopathologic parameters and prognosis.
Results
There were 201 liver transplant recipients enrolled from two hospitals in our study. The pre- and post-transplant prevalences of metabolic dysfunction-associated fatty liver disease were 9.95% and 28.86%, respectively. The clinicopathological parameters revealed a similarity between patients with and without pre-transplant metabolic dysfunction-associated fatty liver disease. In contrast, the group with post-transplant metabolic dysfunction-associated fatty liver disease was linked with older age, a higher hepatitis recurrence rate and incidence of cardiovascular disease, usage of calcineurin inhibitors, a greater body mass index and waist circumference, lower albumin and high-density lipoprotein cholesterol levels, and poorer tumor-free survival and overall survival. The multivariate analysis showed the largest tumor size >4 cm (95% confidence intervals: 0.06~0.63, p = 0.006), microvascular invasion (95% confidence intervals: 1.61~14.92, p = 0.005), post-transplant metabolic dysfunction-associated fatty liver disease (95% confidence intervals: 1.40~10.60, p = 0.009), and calcineurin inhibitors-based regimen (95% confidence intervals: 0.33~0.96, p = 0.036) were the independent risk factors for recurrent hepatocellular carcinoma.
Conclusions
Our study suggests that post-transplant metabolic dysfunction-associated fatty liver disease is more closely to metabolic abnormalities and that it can help identify liver transplant recipients at high risk of recurrent hepatocellular carcinoma.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Zhang S, Wang F, Zhang Z. Current advances in the elimination of hepatitis B in China by 2030. Front Med. 2017;11:490–501.
Arends P, Sonneveld MJ, Zoutendijk R, Carey I, Brown A, Fasano M, et al. Entecavir treatment does not eliminate the risk of hepatocellular carcinoma in chronic hepatitis B: limited role for risk scores in Caucasians. Gut. 2015;64:1289–95.
Petrick JL, Florio AA, Znaor A, Ruggieri D, Laversanne M, Alvarez CS, et al. International trends in hepatocellular carcinoma incidence, 1978–2012. Int J Cancer. 2020;147:317–30.
Wong MCS, Huang JLW, George J, Huang J, Leung C, Eslam M, et al. The changing epidemiology of liver diseases in the Asia-Pacific region. Nat Rev Gastroenterol Hepatol. 2019;16:57–73.
White DL, Kanwal F, El-Serag HB. Association between nonalcoholic fatty liver disease and risk for hepatocellular cancer, based on systematic review. Clin Gastroenterol Hepatol. 2012;10:1342–59.e2.
Muthiah MD, Cheng Han N, Sanyal AJ. A clinical overview of non-alcoholic fatty liver disease: a guide to diagnosis, the clinical features, and complications—what the non-specialist needs to know. Diabetes Obes Metab. 2022;24:3–14.
Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62:S47–64.
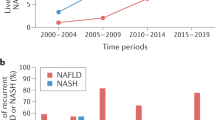
Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11–20.
Estes C, Anstee QM, Arias-Loste MT, Bantel H, Bellentani S, Caballeria J, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J Hepatol. 2018;69:896–904.
Farrell GC, Chitturi S, Lau GK, Sollano JD, Asia-Pacific Working Party on N. Guidelines for the assessment and management of non-alcoholic fatty liver disease in the Asia-Pacific region: executive summary. J Gastroenterol Hepatol. 2007;22:775–7.
Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–9.
Eslam M, Sanyal AJ, George J, International Consensus P. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020;158:1999–2014.e1.
Liang Y, Chen H, Liu Y, Hou X, Wei L, Bao Y, et al. Association of MAFLD with diabetes, chronic kidney disease, and cardiovascular disease: a 4.6-year cohort study in China. J Clin Endocrinol Metab. 2022;107:88–97.
Ioannou GN. Epidemiology and risk-stratification of NAFLD-associated HCC. J Hepatol. 2021;75:1476–84.
Alharthi J, Gastaldelli A, Cua IH, Ghazinian H, Eslam M. Metabolic dysfunction-associated fatty liver disease: a year in review. Curr Opin Gastroenterol. 2022;38:251–60.
Kawaguchi T, Tsutsumi T, Nakano D, Eslam M, George J, Torimura T. MAFLD enhances clinical practice for liver disease in the Asia-Pacific region. Clin Mol Hepatol. 2022;28:150–63.
Chan KE, Koh TJL, Tang ASP, Quek J, Yong JN, Tay P, et al. Global prevalence and clinical characteristics of metabolic-associated fatty liver disease: a meta-analysis and systematic review of 10 739 607 individuals. J Clin Endocrinol Metab. 2022;107:2691–700.
Pan F, Cao S, Li XL, Jia YN, Wang RL, He Q, et al. The model for end-stage liver disease score and the follow-up period can cause the shift of circulating lymphocyte subsets in liver transplant recipients. Front Med (Lausanne). 2021;8:779443.
Reuben A. Long-term management of the liver transplant patient: diabetes, hyperlipidemia, and obesity. Liver Transpl. 2001;7:S13–21.
Watt KD, Charlton MR. Metabolic syndrome and liver transplantation: a review and guide to management. J Hepatol. 2010;53:199–206.
Kurdi A, Martinet W, De Meyer GRY. mTOR inhibition and cardiovascular diseases: dyslipidemia and atherosclerosis. Transplantation. 2018;102:S44–S6.
Jindal RM, Sidner RA, Milgrom ML. Post-transplant diabetes mellitus. The role of immunosuppression. Drug Saf. 1997;16:242–57.
Xu WL, Wang RL, Liu Z, Wu Q, Li XL, He Q, et al. Granzyme B-producing B cells function as a feedback loop for T helper cells in liver transplant recipients with acute rejection. Inflammation. 2021;44:2270–8.
Zhu JQ, Wang J, Li XL, Xu WL, Lv SC, Zhao X, et al. A combination of the percentages of IFN-gamma(+)CD4(+)T cells and granzyme B(+)CD19(+)B cells is associated with acute hepatic rejection: a case control study. J Transl Med. 2021;19:187.
Bechtold M, Palmer J, Valtos J, Iasiello C, Sowers J. Metabolic syndrome in the elderly. Curr Diab Rep. 2006;6:64–71.
Jimenez-Perez M, Gonzalez-Grande R, Omonte Guzman E, Amo Trillo V, Rodrigo Lopez JM. Metabolic complications in liver transplant recipients. World J Gastroenterol. 2016;22:6416–23.
Kral JG, Thung SN, Biron S, Hould FS, Lebel S, Marceau S, et al. Effects of surgical treatment of the metabolic syndrome on liver fibrosis and cirrhosis. Surgery. 2004;135:48–58.
Wang MD, Tang SC, Li C, Sun LY, Xu X, Liang YJ, et al. Association of concurrent metabolic syndrome with long-term oncological prognosis following liver resection for hepatocellular carcinoma among patients with Chronic Hepatitis B virus infection: a multicenter study of 1753 patients. Ann Surg Oncol. 2023;30:346–58.
Dai J, Zhu X, Shen J, Zhang Y, Xie F, Yu Y, et al. The effect of metabolic syndrome on the outcome of Hepatitis B-associated hepatocellular carcinoma patients after hepatectomy: a multicenter study. Front Oncol. 2022;12:811084.
Tabrizian P, Holzner ML, Mehta N, Halazun K, Agopian VG, Yao F, et al. Ten-year outcomes of liver transplant and downstaging for hepatocellular carcinoma. JAMA Surg. 2022;157:779–88.
Vitale A, Peck-Radosavljevic M, Giannini EG, Vibert E, Sieghart W, Van Poucke S, et al. Personalized treatment of patients with very early hepatocellular carcinoma. J Hepatol. 2017;66:412–23.
Mehta N, Heimbach J, Harnois DM, Sapisochin G, Dodge JL, Lee D, et al. Validation of a risk estimation of tumor recurrence after transplant (retreat) score for hepatocellular carcinoma recurrence after liver transplant. JAMA Oncol. 2017;3:493–500.
Schnitzbauer AA, Filmann N, Adam R, Bachellier P, Bechstein WO, Becker T, et al. mTOR inhibition is most beneficial after liver transplantation for hepatocellular carcinoma in patients with active tumors. Ann Surg. 2020;272:855–62.
Rodriguez-Peralvarez M, Colmenero J, Gonzalez A, Gastaca M, Curell A, Caballero-Marcos A, et al. Cumulative exposure to tacrolimus and incidence of cancer after liver transplantation. Am J Transpl. 2022;22:1671–82.
Yun B, Ahn SH, Oh J, Yoon JH, Kim BK. Prognostic impact of MAFLD following surgical resection of Hepatitis B virus-related hepatocellular carcinoma: a nationwide cohort study. Cancers (Basel). 2022;14:5002.
Lin YP, Wang PM, Chuang CH, Yong CC, Liu YW, Huang PY, et al. Metabolic risks are increasing in non-B non-C early-stage hepatocellular carcinoma: a 10-year follow-up study. Front Oncol. 2022;12:816472.
Author information
Authors and Affiliations
Contributions
HDD and HQ contributed conception and design of the study; ZJQ, YXY, and YSW organized the database; RZY, LJZ, and JYN performed the analysis; LZ, DC, KJT, and LXL performed the follow-up and collected the data; ZJQ, YXY, and YSW wrote the first draft of the manuscript; the rest wrote and revised sections of the manuscript. All authors contributed to the manuscript revision, read and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Institutional Review Board of both hospitals in accordance with the 1964 Helsinki Declaration and its later amendments. Written informed consent from patients was waived since it was a retrospective study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, JQ., Ye, XY., Yang, SW. et al. Impact of metabolic dysfunction-associated fatty liver disease on liver transplant recipients with hepatitis B virus-related hepatocellular carcinoma. Eur J Clin Nutr 78, 107–113 (2024). https://doi.org/10.1038/s41430-023-01363-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-023-01363-y