Abstract
Background and objectives
Cumulative lipid profile burden is designed to dynamically measure lipid accumulation, and its effect on hypertension has been poorly studied. Our main purpose was to investigate the effect of cumulative lipid profile burden on the incidence of essential hypertension (EH) and to investigate whether cumulative lipid burden mediates the pathogenesis of the effects of diet and obesity on EH.
Subjects and methods
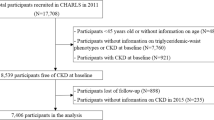
A total of 1295 participants were included in the study, which started in 2017. The average follow-up time was 2.98 years. A total of 240 EH patients occurred during the follow-up period.
Results
The HR (95% CI) of the highest quartile in cumulative Total cholesterol (TC), triglyceride (TG) and high density lipoprotein (HDL) burden were 1.747 (1.145 - 2.664), 1.502 (1.038 - 2.173), 0.615 (0.413 - 0.917) for incidence of EH respectively, compared to the respective reference groups. Participants with EH consumed more red meat and refined grains, and red meat was positively associated with cumulative TC burden. BMI and Waist-To-Height Ratio (WHtR) increased the incidence of EH, and obesity was positively correlated with cumulative TG burden. Mediating analysis showed that cumulative TG had a partial mediating effect in the causal relationship between obesity and EH, and Mendelian randomization (MR) also proved this result. Diet was not found to influence EHn through cumulative lipid profile burden.
Conclusions
The cumulative TG burden partially mediates the effect of obesity on EH.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Original data may be reasonably requested from corresponding authors.
References
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–50.
Chen S, Cheng W. Relationship between lipid profiles and hypertension: a cross-sectional study of 62,957 chinese adult males. Front Public Health. 2022;10:895499–510.
van Oort S, Beulens J, van Ballegooijen AJ, Grobbee DE, Larsson SC. Association of cardiovascular risk factors and lifestyle behaviors with hypertension: a mendelian randomization study. Hypertension. 2020;76:1971–9.
Ference BA, Graham I, Tokgozoglu L, Catapano AL. Impact of lipids on cardiovascular health: jacc health promotion series. J Am Coll Cardiol. 2018;72:1141–56.
Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366:321–9.
Wu J, Wang Y, Kang K, Wang A, Xu J, Zhao X. Association between cumulative exposure to different lipid parameters and risk of newly developed carotid plaque. Stroke Vasc Neurol. 2021;6:359–65.
Dai L, Xu J, Zhang Y, Wang A, Chen Z, Mo J, et al. Cumulative burden of lipid profiles predict future incidence of ischaemic stroke and residual risk. Stroke Vasc Neurol. 2021;6:581–8.
Ozemek C, Laddu DR, Arena R, Lavie CJ. The role of diet for prevention and management of hypertension. Curr Opin Cardiol. 2018;33:388–93.
Hassannejad R, Moosavian SP, Mohammadifard N, Mansourian M, Roohafza H, Sadeghi M, et al. Long-term association of red meat consumption and lipid profile: a 13-year prospective population-based cohort study. Nutrition. 2021;86:111144–51.
Hollaender PL, Ross AB, Kristensen M. Whole-grain and blood lipid changes in apparently healthy adults: a systematic review and meta-analysis of randomized controlled studies. Am J Clin Nutr. 2015;102:556–72.
Darand M, Alizadeh S, Mansourian M. The effect of brassica vegetables on blood glucose levels and lipid profiles in adults. A systematic review and meta-analysis. Phytother Res. 2022;36:1914–29.
Dehghan M, Mente A, Rangarajan S, Mohan V, Lear S, Swaminathan S, et al. Association of egg intake with blood lipids, cardiovascular disease, and mortality in 177,000 people in 50 countries. Am J Clin Nutr. 2020;111:795–803.
Chen R, Zuo Z, Li Q, Wang H, Li N, Zhang H, et al. Dha substitution overcomes high-fat diet-induced disturbance in the circadian rhythm of lipid metabolism. Food Funct. 2020;11:3621–31.
Zhao C, Qu Q, Yang F, Li Z, Yang P, Han L, et al. Monascus ruber fermented panax ginseng ameliorates lipid metabolism disorders and modulate gut microbiota in rats fed a high-fat diet. J Ethnopharmacol. 2021;278:114300–9.
Landsberg L, Aronne LJ, Beilin LJ, Burke V, Igel LI, Lloyd-Jones D, et al. Obesity-related hypertension: pathogenesis, cardiovascular risk, and treatment: a position paper of the obesity society and the american society of hypertension. J Clin Hypertens (Greenwich). 2013;15:14–33.
Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res. 2017;122:1–7.
Powell-Wiley TM, Poirier P, Burke LE, Despres JP, Gordon-Larsen P, Lavie CJ, et al. Obesity and cardiovascular disease: a scientific statement from the american heart association. Circulation. 2021;143:e984–1010.
Zhang T, Chen J, Tang X, Luo Q, Xu D, Yu B. Interaction between adipocytes and high-density lipoprotein:new insights into the mechanism of obesity-induced dyslipidemia and atherosclerosis. Lipids Health Dis. 2019;18:223–34.
Duong M, Uno K, Nankivell V, Bursill C, Nicholls SJ. Induction of obesity impairs reverse cholesterol transport in ob/ob mice. PLoS One. 2018;13:e202102–19.
Yamada R, Okura H, Kume T, Neishi Y, Kawamoto T, Watanabe N, et al. Histological characteristics of plaque with ultrasonic attenuation: a comparison between intravascular ultrasound and histology. J Cardiol. 2007;50:223–8.
Bogaert YE, Linas S. The role of obesity in the pathogenesis of hypertension. Nat Clin Pract Nephrol. 2009;5:101–11.
Revision JCFG. 2018 chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. 2019;16:182–241.
Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in chinese adults–study on optimal cut-off points of body mass index and waist circumference in chinese adults. Biomed Environ Sci. 2002;15:83–96.
Zuo YQ, Gao ZH, Yin YL, Yang X, Feng PY. Association between the cardiometabolic index and hyperuricemia in an asymptomatic population with normal body mass index. Int J Gen Med. 2021;14:8603–10.
Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, et al. Visceral adiposity index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33:920–2.
Members ATF, CPG ECFP, Societies ENC. 2019 esc/eas guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Atherosclerosis. 2019;290:140–205.
National Cholesterol Education Program NCEP Expert Panel On Detection EATO. Third report of the national cholesterol education program (ncep) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel iii) final report. Circulation. 2002;106:3143–421.
Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: theory, methods, and prescriptions. Multivariate Behav Res. 2007;42:185–227.
Relton CL, Davey SG. Two-step epigenetic mendelian randomization: a strategy for establishing the causal role of epigenetic processes in pathways to disease. Int J Epidemiol. 2012;41:161–76.
MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614.
Halperin RO, Sesso HD, Ma J, Buring JE, Stampfer MJ, Gaziano JM. Dyslipidemia and the risk of incident hypertension in men. Hypertension. 2006;47:45–50.
Ahanchi NS, Tamehri ZS, Khalili D, Azizi F, Hadaegh F. Sex specific trajectories of central adiposity, lipid indices, and glucose level with incident hypertension: 12 years follow-up in tehran lipid and glucose study. J Transl Med. 2021;19:84–96.
He D, Fan F, Jia J, Jiang Y, Sun P, Wu Z, et al. Lipid profiles and the risk of new-onset hypertension in a chinese community-based cohort. Nutr Metab Cardiovasc Dis. 2021;31:911–20.
Welsh C, Celis-Morales CA, Brown R, Mackay DF, Lewsey J, Mark PB, et al. Comparison of conventional lipoprotein tests and apolipoproteins in the prediction of cardiovascular disease. Circulation. 2019;140:542–52.
Tomita Y, Sakata S, Arima H, Yamato I, Ibaraki A, Ohtsubo T, et al. Relationship between casual serum triglyceride levels and the development of hypertension in japanese. J Hypertens. 2021;39:677–82.
Kamigaki AS, Siscovick DS, Schwartz SM, Psaty BM, Edwards KL, Raghunathan TE, et al. Low density lipoprotein particle size and risk of early-onset myocardial infarction in women. Am J Epidemiol. 2001;153:939–45.
Chen H, Chen Y, Wu W, Chen Z, Cai Z, Chen Z, et al. Prolonged hyperlipidemia exposure increases the risk of arterial stiffness in young adults: a cross-sectional study in a cohort of chinese. BMC Public Health. 2020;20:1091–1100.
Navar-Boggan AM, Peterson ED, D’Agostino RS, Neely B, Sniderman AD, Pencina MJ. Hyperlipidemia in early adulthood increases long-term risk of coronary heart disease. Circulation. 2015;131:451–8.
Ferroni P, Basili S, Falco A, Davi G. Oxidant stress and platelet activation in hypercholesterolemia. Antioxid Redox Signal. 2004;6:747–56.
Moriel P, Plavnik FL, Zanella MT, Bertolami MC, Abdalla DS. Lipid peroxidation and antioxidants in hyperlipidemia and hypertension. Biol Res. 2000;33:105–12.
Wang JA, Zhen EZ, Guo ZZ, Lu YC. Effect of hyperlipidemic serum on lipid peroxidation, synthesis of prostacyclin and thromboxane by cultured endothelial cells: protective effect of antioxidants. Free Radic Biol Med. 1989;7:243–9.
Karki P, Birukov KG. Lipid mediators in the regulation of endothelial barriers. Tissue Barriers. 2018;6:e1385515–73.
Martin SS, Michos ED. Mapping hyperlipidemia in young adulthood to coronary risk: importance of cumulative exposure and how to stay young. Circulation. 2015;131:445–7.
Wang L, Gaziano JM, Liu S, Manson JE, Buring JE, Sesso HD. Whole- and refined-grain intakes and the risk of hypertension in women. Am J Clin Nutr. 2007;86:472–9.
Yu D, Shu XO, Li H, Xiang YB, Yang G, Gao YT, et al. Dietary carbohydrates, refined grains, glycemic load, and risk of coronary heart disease in chinese adults. Am J Epidemiol. 2013;178:1542–9.
Van Horn L, Carson JA, Appel LJ, Burke LE, Economos C, Karmally W, et al. Recommended dietary pattern to achieve adherence to the american heart association/american college of cardiology (aha/acc) guidelines: a scientific statement from the american heart association. Circulation. 2016;134:e505–29.
Gaesser GA. Perspective: refined grains and health: genuine risk, or guilt by association? Adv Nutr. 2019;10:361–71.
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the american heart association. Circulation. 2020;141:e139–596.
NCD-RisC NRFC. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Preston KJ, Scalia RG, Autieri MV. Adipocyte phenotype flexibility and lipid dysregulation. Cells. 2022;11:817–82.
Li H, Ma J, Zheng D, Li X, Guo X, Wang J, et al. Sex differences in the non-linear association between bmi and ldl cholesterol in middle-aged and older adults: findings from two nationally representative surveys in china. Lipids Health Dis. 2021;20:112–62.
Shamai L, Lurix E, Shen M, Novaro GM, Szomstein S, Rosenthal R, et al. Association of body mass index and lipid profiles: evaluation of a broad spectrum of body mass index patients including the morbidly obese. Obes Surg. 2011;21:42–47.
Vincent HK, Innes KE, Vincent KR. Oxidative stress and potential interventions to reduce oxidative stress in overweight and obesity. Diabetes Obes Metab. 2007;9:813–39.
Franssen R, Monajemi H, Stroes ES, Kastelein JJ. Obesity and dyslipidemia. Med Clin North Am. 2011;95:893–902.
de Jongh RT, Serne EH, Ijzerman RG, de Vries G, Stehouwer CD. Free fatty acid levels modulate microvascular function: relevance for obesity-associated insulin resistance, hypertension, and microangiopathy. Diabetes. 2004;53:2873–82.
Wang H, Li H, Hou Z, Pan L, Shen X, Li G. Role of oxidative stress in elevated blood pressure induced by high free fatty acids. Hypertens Res. 2009;32:152–8.
Kim J, Kim J, Kang Y. Noodle consumption is positively associated with incident hypertension in middle-aged and older korean women. Nutr Res Pract. 2019;13:141–9.
Allen TS, Bhatia HS, Wood AC, Momin SR, Allison MA. State-of-the-art review: evidence on red meat consumption and hypertension outcomes. Am J Hypertens. 2022;35:679–87.
Diarz EJ, Leyaro BJ, Kivuyo SL, Ngowi BJ, Msuya SE, Mfinanga SG, et al. Red meat consumption and its association with hypertension and hyperlipidaemia among adult maasai pastoralists of ngorongoro conservation area, tanzania. PLoS One. 2020;15:e233777–95.
Jung H, Lee G, Lim K, Shin S. Association of milk consumption with management and incidence of hypertension among south korean adults: a prospective analysis of the health examinees study cohort. Nutr Metab Cardiovasc Dis. 2022;32:2515–25.
Acknowledgements
Thanks to the lab teachers and students for their efforts in the cohort follow-up process, and thanks to the participants in the cohort study for participating in this study.
Funding
This work was supported by the National Natural Science Foundation of China (NO.81660566), the Open Project Fund of the Key Laboratory of Cardiovascular and Cerebrovascular Diseases of the Ministry of Education (XN201907).
Author information
Authors and Affiliations
Contributions
TZ is responsible for collecting data, analyzing data and assisting in paper writing; QW, XC, YZ, TX, YD and FG are responsible for collecting, sorting out and analyzing data; QW and MD are responsible for assisting in paper writing; XL is responsible for research design and paper writing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The research proposal was approved by the Ethics Committee of Gannan medical university.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41430_2023_1348_MOESM8_ESM.docx
Supplementary table 5 MR directional pleiotropy test (MR Egger) of the associations of education, intelligence, or cognition with hypertension and blood pressure.
Supplementary table 10 MVMR estimates for the causal associations of triglyceride with hypertension.
41430_2023_1348_MOESM16_ESM.docx
Supplementary table 13 Mendelian randomization (MR) estimates of proportions mediated by triglyceride in the causal association between obesity and hypertension.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, T., Wang, Q., Cui, Xm. et al. Mediating effect of cumulative lipid profile burden on the effect of diet and obesity on hypertension incidence: a cohort study of people aged 35-65 in rural China. Eur J Clin Nutr 78, 54–63 (2024). https://doi.org/10.1038/s41430-023-01348-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-023-01348-x