Abstract
Background & objective
To investigate the causal effects of plasma Polyunsaturated fatty acids (PUFAs) on the risk of juvenile idiopathic arthritis (JIA) and ocular comorbidity through Mendelian randomization (MR) analysis.
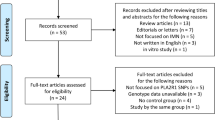
Methods
Genetic variants (formerly single nucleotide polymorphisms, SNPs) that are strongly associated with PUFAs levels (P < 5×10−8) were selected as instrumental variables. Summary-level MR was performed with outcome estimates for JIA (n = 31,142) and JIA associated iridocyclitis (n = 94,197). The inverse variance-weighted (IVW) method was employed as the main approach to combine the estimation for each SNP. Two set of models with summary statistics were conducted and multiple sensitivity analyses were applied for testing of pleiotropic bias.
Results
In model 1, genetically predicted n-6 PUFAs linoleic acid (LA) and arachidonic acid (AA) were associated with lower and higher risk of JIA associated iridocyclitis using IVW (ORLA = 0.940, 95% CI: 0.895–0.988, P = 0.015; ORAA = 1.053, 95% CI: 1.007–1.101, P = 0.024). No such association was observed between each plasma PUFAs and JIA susceptibility (P > 0.05). In further MR analysis, results from model 2 also showed a consistent trend. Besides, multiple sensitivity analyses revealed that there was no obvious evidence for unknown pleiotropy (P > 0.05).
Conclusions
Our MR study provides genetic evidence on the possible causality that plasma LA level might protect against JIA associated iridocyclitis, whereas AA was responsible for opposite effect.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data and material that support the findings of this study are available from public datasets in NHGRIEBI GWAS Catalog and MRC IEU Open GWAS Project.
References
Manners PJ, Bower C. Worldwide prevalence of juvenile arthritis why does it vary so much? J Rheumatol. 2002;29:1520–30. e-pub ahead of print 2002/07/26
Tugal-Tutkun I, Quartier P, Bodaghi B. Disease of the year: juvenile idiopathic arthritis-associated uveitis-classification and diagnostic approach. Ocul Immunol Inflamm. 2014;22:56–63. https://doi.org/10.3109/09273948.2013.871565. e-pub ahead of print 2014/01/15
Tugal-Tutkun I, Havrlikova K, Power WJ, Foster CS. Changing patterns in uveitis of childhood. Ophthalmology. 1996;103:375–83. https://doi.org/10.1016/s0161-6420(96)30682-9. e-pub ahead of print 1996/03/01
Al-Mayouf SM, Al Mutairi M, Bouayed K, Habjoka S, Hadef D, Lotfy HM, et al. Epidemiology and demographics of juvenile idiopathic arthritis in Africa and Middle East. Pediatr Rheumatol Online J. 2021;19:166 https://doi.org/10.1186/s12969-021-00650-x. e-pub ahead of print 2021/12/04
Finch SL, Rosenberg AM, Vatanparast H. Vitamin D and juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2018;16:34 https://doi.org/10.1186/s12969-018-0250-0. e-pub ahead of print 2018/05/18
Majumder S, Aggarwal A. Juvenile idiopathic arthritis and the gut microbiome: Where are we now. Best Pr Res Clin Rheumatol. 2019;33:101496 https://doi.org/10.1016/j.berh.2020.101496. e-pub ahead of print 2020/03/17
Gorska A, Urban M, Pietrewicz E, Gorski S. Composition of linoleic and arachidonic acids in phosphatidylcholine of erythrocytes membrane and IL-6 and TNF-alpha in serum and C-reactive protein concentration in children with juvenile idiopathic arthritis. Pol Merkur Lekarski. 2006;21:551–3. e-pub ahead of print 2007/04/05
Gorczyca D, Postepski J, Czajkowska A, Pasciak M, Prescha A, Olesinska E, et al. The profile of polyunsaturated fatty acids in juvenile idiopathic arthritis and association with disease activity. Clin Rheumatol. 2017;36:1269–79. https://doi.org/10.1007/s10067-017-3586-9. e-pub ahead of print 2017/03/02
Kremer JM, Lawrence DA, Jubiz W, DiGiacomo R, Rynes R, Bartholomew LE, et al. Dietary fish oil and olive oil supplementation in patients with rheumatoid arthritis. Clin immunologic Eff Arthritis Rheum. 1990;33:810–20. https://doi.org/10.1002/art.1780330607. e-pub ahead of print 1990/06/01
Miles EA, Calder PC. Influence of marine n-3 polyunsaturated fatty acids on immune function and a systematic review of their effects on clinical outcomes in rheumatoid arthritis. Br J Nutr. 2012;107(Suppl 2):S171–184. https://doi.org/10.1017/S0007114512001560. e-pub ahead of print 2012/05/25
de Pablo P, Romaguera D, Fisk HL, Calder PC, Quirke AM, Cartwright AJ, et al. High erythrocyte levels of the n-6 polyunsaturated fatty acid linoleic acid are associated with lower risk of subsequent rheumatoid arthritis in a southern European nested case-control study. Ann Rheum Dis. 2018;77:981–7. https://doi.org/10.1136/annrheumdis-2017-212274. e-pub ahead of print 2018/02/14
Park Y, Lee A, Shim SC, Lee JH, Choe JY, Ahn H, et al. Effect of n-3 polyunsaturated fatty acid supplementation in patients with rheumatoid arthritis: a 16-week randomized, double-blind, placebo-controlled, parallel-design multicenter study in Korea. J Nutr Biochem. 2013;24:1367–72. https://doi.org/10.1016/j.jnutbio.2012.11.004. e-pub ahead of print 2013/01/22
Bosdriesz JR, Stel VS, van Diepen M, Meuleman Y, Dekker FW, Zoccali C, et al. Evidence-based medicine-When observational studies are better than randomized controlled trials. Nephrol (Carlton). 2020;25:737–43. https://doi.org/10.1111/nep.13742. e-pub ahead of print 2020/06/17
Smith GD, Ebrahim S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003;32:1–22. https://doi.org/10.1093/ije/dyg070. e-pub ahead of print 2003/04/12
Burgess S, Scott RA, Timpson NJ, Davey Smith G, Thompson SG, Consortium E-I. Using published data in Mendelian randomization: a blueprint for efficient identification of causal risk factors. Eur J Epidemiol. 2015;30:543–52. https://doi.org/10.1007/s10654-015-0011-z. e-pub ahead of print 2015/03/17
Lopez-Isac E, Smith SL, Marion MC, Wood A, Sudman M, Yarwood A et al. Combined genetic analysis of juvenile idiopathic arthritis clinical subtypes identifies novel risk loci, target genes and key regulatory mechanisms. Ann Rheum Dis 2020. e-pub ahead of print 2020/10/28; https://doi.org/10.1136/annrheumdis-2020-218481
Lemaitre RN, Tanaka T, Tang W, Manichaikul A, Foy M, Kabagambe EK, et al. Genetic loci associated with plasma phospholipid n-3 fatty acids: a meta-analysis of genome-wide association studies from the CHARGE Consortium. PLoS Genet. 2011;7:e1002193 https://doi.org/10.1371/journal.pgen.1002193. e-pub ahead of print 2011/08/11
Guan W, Steffen BT, Lemaitre RN, Wu JHY, Tanaka T, Manichaikul A, et al. Genome-wide association study of plasma N6 polyunsaturated fatty acids within the cohorts for heart and aging research in genomic epidemiology consortium. Circ Cardiovasc Genet. 2014;7:321–31. https://doi.org/10.1161/CIRCGENETICS.113.000208. e-pub ahead of print 2014/05/16
Tomata Y, Larsson SC, Hagg S. Polyunsaturated fatty acids and risk of Alzheimer’s disease: a Mendelian randomization study. Eur J Nutr. 2020;59:1763–6. https://doi.org/10.1007/s00394-019-02126-x. e-pub ahead of print 2019/11/05
Wang K, Zhong Y, Yang F, Hu C, Liu X, Zhu Y, et al. Causal effects of N-6 polyunsaturated fatty acids on age-related macular degeneration: a mendelian randomization study. J Clin Endocrinol Metab. 2021;106:e3565–e3572. https://doi.org/10.1210/clinem/dgab338. e-pub ahead of print 2021/05/14
Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50:693–8. https://doi.org/10.1038/s41588-018-0099-7. e-pub ahead of print 2018/04/25
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37:658–65. https://doi.org/10.1002/gepi.21758. e-pub ahead of print 2013/10/12
Burgess S, Thompson SG. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur J Epidemiol. 2017;32:377–89. https://doi.org/10.1007/s10654-017-0255-x. e-pub ahead of print 2017/05/21
Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40:304–14. https://doi.org/10.1002/gepi.21965. e-pub ahead of print 2016/04/12
May-Wilson S, Sud A, Law PJ, Palin K, Tuupanen S, Gylfe A, et al. Pro-inflammatory fatty acid profile and colorectal cancer risk: A Mendelian randomisation analysis. Eur J Cancer. 2017;84:228–38. https://doi.org/10.1016/j.ejca.2017.07.034. e-pub ahead of print 2017/08/23
Illig T, Gieger C, Zhai G, Romisch-Margl W, Wang-Sattler R, Prehn C, et al. A genome-wide perspective of genetic variation in human metabolism. Nat Genet. 2010;42:137–41. https://doi.org/10.1038/ng.507. e-pub ahead of print 2009/12/29
Hoglund J, Rafati N, Rask-Andersen M, Enroth S, Karlsson T, Ek WE, et al. Improved power and precision with whole genome sequencing data in genome-wide association studies of inflammatory biomarkers. Sci Rep. 2019;9:16844 https://doi.org/10.1038/s41598-019-53111-7. e-pub ahead of print 2019/11/16
Gheita T, Kamel S, Helmy N, El-Laithy N, Monir A. Omega-3 fatty acids in juvenile idiopathic arthritis: effect on cytokines (IL-1 and TNF-alpha), disease activity and response criteria. Clin Rheumatol. 2012;31:363–6. https://doi.org/10.1007/s10067-011-1848-5. e-pub ahead of print 2011/09/17
Huang X, Ye Z, Cao Q, Su G, Wang Q, Deng J, et al. Gut Microbiota Composition and Fecal Metabolic Phenotype in Patients With Acute Anterior Uveitis. Invest Ophthalmol Vis Sci. 2018;59:1523–31. https://doi.org/10.1167/iovs.17-22677. e-pub ahead of print 2018/04/07
Uchi SH, Yanai R, Kobayashi M, Hatano M, Kobayashi Y, Yamashiro C, et al. Dendritic cells mediate the anti-inflammatory action of omega-3 long-chain polyunsaturated fatty acids in experimental autoimmune uveitis. PLoS One. 2019;14:e0219405 https://doi.org/10.1371/journal.pone.0219405. e-pub ahead of print 2019/07/25
Shoda H, Yanai R, Yoshimura T, Nagai T, Kimura K, Sobrin L, et al. Dietary omega-3 fatty acids suppress experimental autoimmune uveitis in association with inhibition of Th1 and Th17 cell function. PLoS One. 2015;10:e0138241 https://doi.org/10.1371/journal.pone.0138241. e-pub ahead of print 2015/09/24
Chu X, Jaeger M, Beumer J, Bakker OB, Aguirre-Gamboa R, Oosting M, et al. Integration of metabolomics, genomics, and immune phenotypes reveals the causal roles of metabolites in disease. Genome Biol. 2021;22:198 https://doi.org/10.1186/s13059-021-02413-z. e-pub ahead of print 2021/07/08
Porcu E, Gilardi F, Darrous L, Yengo L, Bararpour N, Gasser M, et al. Triangulating evidence from longitudinal and Mendelian randomization studies of metabolomic biomarkers for type 2 diabetes. Sci Rep. 2021;11:6197 https://doi.org/10.1038/s41598-021-85684-7. e-pub ahead of print 2021/03/20
Davies NM, Holmes MV, Davey Smith G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ. 2018;362:k601 https://doi.org/10.1136/bmj.k601. e-pub ahead of print 2018/07/14
Zhao JV, Schooling CM. Role of linoleic acid in autoimmune disorders: a Mendelian randomisation study. Ann Rheum Dis. 2019;78:711–3. https://doi.org/10.1136/annrheumdis-2018-214519. e-pub ahead of print 2018/11/10
Park S, Lee S, Kim Y, Lee Y, Kang M, Kim K et al. Causal Effects of Serum Levels of n-3 or n-6 Polyunsaturated Fatty Acids on Coronary Artery Disease: Mendelian Randomization Study. Nutrients; 13. e-pub ahead of print 2021/05/01; https://doi.org/10.3390/nu13051490 2021
Zhao JV, Schooling CM. Effect of linoleic acid on ischemic heart disease and its risk factors: a Mendelian randomization study. BMC Med. 2019;17:61 https://doi.org/10.1186/s12916-019-1293-x. e-pub ahead of print 2019/03/15
Zhao JV, Schooling CM. The role of linoleic acid in asthma and inflammatory markers: a Mendelian randomization study. Am J Clin Nutr. 2019;110:685–90. https://doi.org/10.1093/ajcn/nqz130. e-pub ahead of print 2019/07/10
Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches. Pediatr Rheumatol Online J. 2021;19:135 https://doi.org/10.1186/s12969-021-00629-8. e-pub ahead of print 2021/08/25
Barut K, Adrovic A, Sahin S, Kasapcopur O. Juvenile Idiopathic Arthritis. Balk Med J. 2017;34:90–101. https://doi.org/10.4274/balkanmedj.2017.0111. e-pub ahead of print 2017/04/19
Huang X, Yi S, Hu J, Du Z, Wang Q, Ye Z, et al. Linoleic acid inhibits in vitro function of human and murine dendritic cells, CD4(+)T cells and retinal pigment epithelial cells. Graefes Arch Clin Exp Ophthalmol. 2021;259:987–98. https://doi.org/10.1007/s00417-020-04972-6. e-pub ahead of print 2020/10/21
Elison JR, Weinstein JE, Sheets KG, Regan CE Jr, Lentz JJ, Reinoso M, et al. Platelet-activating factor (PAF) receptor antagonism modulates inflammatory signaling in experimental uveitis. Curr Eye Res. 2018;43:821–7. https://doi.org/10.1080/02713683.2018.1454476. e-pub ahead of print 2018/04/12
Liao T, Ke Y, Shao WH, Haribabu B, Kaplan HJ, Sun D, et al. Blockade of the interaction of leukotriene b4 with its receptor prevents development of autoimmune uveitis. Invest Ophthalmol Vis Sci. 2006;47:1543–9. https://doi.org/10.1167/iovs.05-1238. e-pub ahead of print 2006/03/28
Eskandarpour M, Nunn MA, Weston-Davies W, Calder VL. Immune-Mediated Retinal Vasculitis in Posterior Uveitis and Experimental Models: The Leukotriene (LT)B4-VEGF Axis. Cells; 10. e-pub ahead of print 2021/03/07; https://doi.org/10.3390/cells10020396 2021
Adam O, Beringer C, Kless T, Lemmen C, Adam A, Wiseman M, et al. Anti-inflammatory effects of a low arachidonic acid diet and fish oil in patients with rheumatoid arthritis. Rheumatol Int. 2003;23:27–36. https://doi.org/10.1007/s00296-002-0234-7. e-pub ahead of print 2003/01/28
Acknowledgements
We thank all the investigators of the NHGRIEBI GWAS Catalog and the MRC IEU Open GWAS Project for providing the data publicly.
Author information
Authors and Affiliations
Contributions
QS, CZ, and JY were involved in the conceptualization, the design of the study and drafted the manuscript; QS and CZ acquired and analyzed the data; YL, SH and JM helped to design the research; JZ revise the manuscript, supervise the study and perform data interpretation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All analyses were based on previous published studies; thus, no ethical approval and patient consent are required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shu, Q., Zhao, C., Yu, J. et al. Causal analysis of serum polyunsaturated fatty acids with juvenile idiopathic arthritis and ocular comorbidity. Eur J Clin Nutr 77, 75–81 (2023). https://doi.org/10.1038/s41430-022-01196-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01196-1