Abstract
Objectives
The study aimed to explore the risk factors for the outcome of nutrition support teams (NSTs) for elderly patients. Previously identified risk factors lack general versatility owing to slightly subjective judgment standards; this study aimed to explore an objective and simple index of NST outcome and identify the risk factors for NST outcome.
Subjects
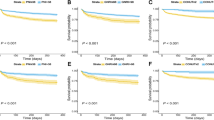
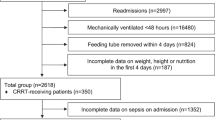
This retrospective observational study analyzed, 372 elderly patients enrolled in the NST between January 2014 and July 2018. We identified that the energy fill rate to total energy expenditure (%TEE) at the time of NST termination (post-%TEE) < 75.0% was the most valid index for the outcome in our previous study. The cutoff values of continuous variables at the time of NST enrollment (pre-) were set for post-%TEE < 75.0% using receiver operating characteristic curve analysis, and hazard ratios (HRs) were calculated.
Results
From the multivariable Cox proportional hazard analysis, pre-%TEE < 62.6% (HR: 1.96; 95% confidence interval [95% CI]: 1.29–2.99; p = 0.002), presence of pressure ulcers (HR: 1.74; 95% CI: 1.02–2.98; p = 0.042), pre-prognostic nutritional index (PNI) < 32.7 (HR: 1.78; 95% CI: 1.13–2.82; p = 0.014), and presence of pre-peripheral parenteral nutrition (PPN) (HR: 1.74; 95% CI: 1.19–2.56; p = 0.005) were identified as independent risk factors for post-%TEE < 75.0%.
Conclusion
Post-%TEE < 75.0% was the objective and simple index for NST outcomes. Patients with low pre-%TEE, pressure ulcers, low pre-PNI, or pre-PPN require early nutritional intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Additional data are available from the corresponding author on reasonable request.
References
Potter JF, Schafer DF, Bohi RL. In-hospital mortality as a function of body mass index: an age-dependent variable. J Gerontol. 1988;43:M59–63.
Guigoz Y, Vellas B, Garry PJ. Assessing the nutritional status of the elderly: The Mini Nutritional Assessment as part of the geriatric evaluation. Nutr Rev. 1996;54:S59–65.
Antonelli Incalzi R, Landi F, Cipriani L, Bruno E, Pagano F, Gemma A, et al. Nutritional assessment: a primary component of multidimensional geriatric assessment in the acute care setting. J Am Geriatr Soc. 1996;44:166–74.
Gavazzi G, Krause K-H. Ageing and infection. Lancet Infect Dis. 2002;2:659–66.
Martín S, Pérez A, Aldecoa C. Sepsis and immunosenescence in the elderly patient: A review. Front Med. 2017;4:20.
Akner G, Cederhol T. Treatment of protein-energy malnutrition in chronic nonmalignant disorders. Am J Clin Nutr. 2001;74:6–24.
Dudrick SJ, Wilmore DW, Vars HM, Rhoads JE. Long-term total parenteral nutrition with growth, development, and positive nitrogen balance. Nutr Hosp. 1968;16:287–92.
United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2019: Data Booklet. 2019. https://population.un.org/wpp/Publications/Files/WPP2019_DataBooklet.pdf
Ministry of Health, Labour and Welfare of Japan. Chart 1-1-1 Transition of a population pyramid (1990 or 2015 or 2025 or 2065)- medium estimation in 2017-|2017 edition public welfare labor white paper - social security and economic growth- (in Japanese). Tokyo: MHLW, 2017. https://www.mhlw.go.jp/wp/hakusyo/kousei/17/backdata/02-01-01-01.html?SLANG=ja&TLANG=en&XMODE=0&XPARAM=q,&XCHARSET=UTF-8&XPORG=,&XJSID=0. Accessed 10 May 2022.
Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent J-P, Nicolis I, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82:777–83.
Hiramatsu M, Momoki C, Kato K, Yasui Y, Oide Y, Kaneishi C, et al. Exploration of nutrition support team outcome predictors for elderly. J Nutr Med Diet Care. 3 (2017).
Hiramatsu M, Momoki C, Oide Y, Kaneishi C, Yasui Y, Shoji K, et al. Association between risk factors and intensive nutritional intervention outcomes in elderly individuals. J Clin Med Res. 2019;11:472–9.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–82.
Gomes F, Schuetz P, Bounoure L, Austin P, Ballesteros-Pomar M, Cederholm T, et al. ESPEN guidelines on nutritional support for polymorbid internal medicine patients. Clin Nutr. 2018;37:336–53.
Ignacio de Ulíbarri J, González-Madroño A, de Villar NGP, González P, González B, Mancha A, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20:38–45.
González-Madroño A, Mancha A, Rodríguez FJ, Culebras J, de Ulibarri JI. Confirming the validity of the CONUT system for early detection and monitoring of clinical undernutrition: comparison with two logistic regression models developed using SGA as the gold standard. Nutr Hosp. 2012;27:564–71.
Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients (in Japanese). Nippon Geka Gakkai Zasshi. 1984;85:1001–5.
Llop-Talaveron J, Badia-Tahull MB, Leiva-Badosa E. An inflammation-based prognostic score, the C-reactive protein/albumin ratio predicts the morbidity and mortality of patients on parenteral nutrition. Clin Nutr. 2018;37:1575–83.
Contreras-Bolívar V, Sánchez-Torralvo FJ, Ruiz-Vico M, González-Almendros I, Barrios M, Padín S, et al. Glim criteria using hand grip strength adequately predict six-month mortality in cancer inpatients. Nutrients 2019;11:2043.
Lainscak M, Farkas J, Frantal S, Singer P, Bauer P, Hiesmayr M, et al. Self-rated health, nutritional intake and mortality in adult hospitalized patients. Eur J Clin Invest. 2014;44:813–24.
Hiesmayr M, Schindler K, Pernicka E, Schuh C, Schoeniger-Hekele A, Bauer P, et al. Decreased food intake is a risk factor for mortality in hospitalised patients: The NutritionDay survey 2006. Clin Nutr. 2009;28:484–91.
Thibault R, Makhlouf A-M, Kossovsky MP, Iavindrasana J, Chikhi M, Meyer R, et al. Healthcare-associated infections are associated with insufficient dietary intake: an observational cross-sectional study. PLoS One. 2015;10:e0123695.
Horn SD, Bender SA, Ferguson ML, Smout RJ, Bergstrom N, Taler G, et al. The National Pressure Ulcer Long-Term Care Study: pressure ulcer development in long-term care residents. J Am Geriatr Soc. 2004;52:359–67.
Lindgren M, Unosson M, Krantz AM, Ek AC. Pressure ulcer risk factors in patients undergoing surgery. J Adv Nurs. 2005;50:605–12.
Iizaka S, Okuwa M, Sugama J, Sanada H. The impact of malnutrition and nutrition-related factors on the development and severity of pressure ulcers in older patients receiving home care. Clin Nutr. 2010;29:47–53.
Worthington P, Balint J, Bechtold M, Bingham A, Chan LN, Durfee S, et al. When is parenteral nutrition appropriate? J Parenter Enter Nutr. 2017;41:324–77.
Heidegger CP, Berger MM, Graf S, Zingg W, Darmon P, Costanza MC, et al. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: A randomised controlled clinical trial. Lancet 2013;381:385–93.
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). J Parenter Enter Nutr 2016;40:159–211.
Caccialanza R, Cereda E, Caraccia M, Klersy C, Nardi M, Cappello S, et al. Early 7-day supplemental parenteral nutrition improves body composition and muscle strength in hypophagic cancer patients at nutritional risk. Support Care Cancer. 2019;27:2497–506.
Acknowledgements
The authors are grateful to the participants and hospital members.
Author information
Authors and Affiliations
Contributions
MH, YY, and DH contributed to study conception and design; MH, YO, and TF contributed to data acquisition; MH and DH contributed to data analysis and interpretation; MH, YY, and DH contributed to the drafting of manuscript and making critical revisions related to important intellectual content of manuscript; All authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hiramatsu, M., Oide, Y., Yasui, Y. et al. Exploration of an objective and simple index as the outcome of nutrition support for elderly patients and identification of risk factors. Eur J Clin Nutr 76, 1727–1732 (2022). https://doi.org/10.1038/s41430-022-01168-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01168-5