Abstract
Background/objectives
We analyzed the nationwide pediatric inflammatory bowel disease (PIBD) registry (1998–2016), to evaluate the nutritional status at the time of diagnosis.
Subjects/methods
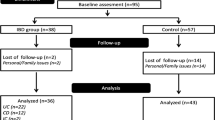
Nine types of nutritional status by the combination of weight-for-length (<2 years)/body mass index (>2 years) and length/height-for-age with three categories (<−2, −2 to 2, and >2 SD) were described. Malnutrition was defined by WHO criteria. Univariate and multivariate regression analysis was used to identify risk factors for malnutrition.
Results
In total, 824 IBD patients (498 Ulcerative colitis (UC); 289 Crohn’s Disease (CD); 37 Indeterminate Colitis (IC); 412 male; the median age 12.5 years) were eligible. The prevalence of eutrophy, wasting/thinness, stunting, overweight, tall stature, concurrent wasting/thinness and stunting, tall stature with overweight, tall stature with wasting/thinness, and short stature with overweight were 67.4%, 14.9%, 6.6%, 3.1%, 3.2%, 3.3%, 1.1%, 0.4%, and 0.1%, respectively. The prevalence of malnutrition was 32.7%, indicating a higher prevalence in CD (p < 0.001). Incidence of overweight was less common in the CD than UC and IC (p < 0.001). Multivariate analysis revealed that age of onset (>10 years), prepubertal stage, severe disease activity, perianal involvement, and high C reactive protein level were independently associated with malnutrition in pediatric IBD.
Conclusion
We showed the frequency of nutritional impairment in PIBD. The percentage of overweight subjects was lower than the other studies. The age of onset, disease activity, CRP level, perianal involvement, and pubertal stage were associated with a higher risk for developing malnutrition. Our results also confirmed that CD patients are particularly vulnerable to nutritional impairment.
Clinical trial number
ClinicalTrials.gov Identifier: NCT04457518.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Raw data the support the findings of this study are available from the corresponding author upon reasonable request. The data that support the findings of this study are available in clinicalTrials.gov at https://clinicaltrials.gov/ct2/show/NCT04457518.
References
Geerling BJ, Badart-Smook A, Stockbrugger RW, Brummer RJ. Comprehensive nutritional status in recently diagnosed patients with inflammatory bowel disease compared with population controls. EJCN. 2000;54:514–21.
Kugathasan S, Nebel J, Skelton JA, Markowitz J, Keljo D, Rosh J, et al. Body mass index in children with newly diagnosed inflammatory bowel disease: observations from two multicenter North American inception cohorts. J Pediatr. 2007;151:523–7.
Pituch-Zdanowska A, Banaszkiewicz A, Dziekiewicz M, Lazowsak-Pzzeorek I, Gawronska A, Kowalska-Duplaga K, et al. Overwight and obesity in children with newly diagnosed inflammatory bowel disease. Adv Med Sci. 2016;61:28–31.
Chandrakumar A, Wang A, Grover K, El-matary W. Obesity is more common in children newly diagnosed with ulcerative colitis as compered to those with Crohn’s disease. JPGN. 2020;70:593–7.
Shim JO. Recent advance in very early-onset inflammatory bowel disease. Intes Res. 2019;17:9–16.
Levine A, Griffiths A, Markowitz J, Wilson DC, Turner D, Russell RK, et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis. 2011;17:1314–21.
Turner D, Otley AR, Mack D, Hyams J, de Bruijne J, Uusoue K, et al. Development and evaluation of a Pediatric ulceratice colitis activity index (PUCAI): a prospective multicenter study. Gastroenterology. 2007;133:423–32.
Turner D, Hyams J, Markowitz J, Lere T, Mack DR, Evans J, et al. Appraisal of the pediatric ulcerative colitis activity index (PUCAI). Inflamm Bowel Dis. 2009;15:1218–23.
Hyams JS, Ferry GD, Mandel FS, Gryboski JD, Kibort PM, Kirschner BS, et al. Development and validation of a pediatric Crohn’s disease activity index. JPGN. 1991;12:439–47.
Turner D, Ruemmele FM, Orlanski-Meyer E, Griffiths AM, De Carpi JM, Bronsky J, et al. Management of paediatric ulcerative colitis, part 1: ambulatory care—an evidence-based guideline from European Crohn’s and Colitis Organization and European Society of Paediatric Gastroenterology, Hepatology and Nutrition. JPGN. 2018;67:257–91.
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. World Health Organization; 2011.
World Health Organization, WHO anthro surwey analizer and other tools. https://www.who.int/childgrowth/software/en/. Accessed 25 Mar 2021.
World Health Organization (WHO), United Nations Children’s Fund (UNICEF): Recommendations for data collection, analysis and reporting on anthropometric indicators in children under 5 years old. Geneve: WHO; UNICEF; 2019. https://www.who.int/nutrition/publications/anthropometry-data-quality-report/en/. Accessed 20 Mar 2021.
WHO. Physical status: the use and interpretation of anthropometry Geneva: WHO, 1995. https://www.who.int/childgrowth/publications/physical_status/en/. Accessed 20 Mar 2021.
da Silva Ferreir H. Anthropometric assesment of children’s nutritional status: a new apprach based on an adaptation of waterlow’s classsification. BMC Pediatr. 2020;20:65.
Tanner JM, Whitehouse RH, Takaishi M. Standards from birth to maturity for height, weight, height velocity, and weight velocity: British children, 1965. II. Arch Dis Child 1966;41:613–35.
Allen LH. Nutritional influences on linear growth: a general review. EJCN. 1994;48:S75–89.
Amaro F, Chiarelli F. Growth and puberty in children with inflammatory bowel diseases. Biomedicines. 2020;8:458.
Miele R, Shamir R, Aloi M, Assa A, Braegger C, Bronsky J, et al. Nutrition in pediatric inflammatory bowel disease: a position paper on behalf of the Porto Inflammatory Bowel Disease Group of the European Society of Pediatric Gastroenterology. Hepatol Nutr JPGN. 2018;66:687–708.
Abraham BP, Mehta S, El-Serag HB. Natural history of pediatric-onset inflammatory bowel disease: a systematic review. J Clin Gastroenterol. 2012;46:581–9.
Kim S, Koh H. Nutritional aspect of pediatric inflammatory bowel disease: its clincal importance. Korean J Pediatr. 2005;58:363–8.
El Mouzan MI, Al Edreesi MH, Al-Hussaini AA, Saadah OI, Al Qourain AA, Al, et al. Nutritional status of children with inflammatory bowel disease in Saudi Arabia. World J Gastroenterol. 2016;22:1854–8.
Vaisman N, Dotan I, Halack A, Niv E. Malabsorption is a major contributor to underweight in Crohn’s disease patients in remission. Nutrition. 2006;22:855–9.
Sawczenko A, Sandhu BK. Presenting features. of inflammatory bowel disease in Great Britain and Ireland. Arch Dis Child. 2003;88:995–1000.
Lee JJ, Escher JC, Shuman MJ, Forbes PW, Delemarre LC, Harr BW, et al. Final adult height of children with inflammatory bowel disease is predicted by parental height and patient minimum height Z-score. Inflamm Bowel Dis. 2010;16:1669–77.
Wiskin AE, Wootton SA, Hunt TM, Cornelius VR, Afzal NA, Jackson AA, et al. Body composition in childhood inflammatory bowel disease. Clin Nutr. 2011;30:112–5.
Pappa HM, Gordon CM, Saslowsky TM, Zholudev A, Horr B, Shih M, et al. Vitamin D status in children and young adults with inflammatory bowel disease. Pediatrics. 2006;118:1950–61.
Jin HY, Lim JS, Lee Y, Choi Y, Oh SH, Kim KM, et al. Growth, puberty, and bone health in children and adolescents with inflammatory bowel disease. BMC Pediatr. 2021;21:35.
Turkey Demographic and Health Survey 2018. http://www.hips.hacettepe.edu.tr/eng/tdhs2018/TDHS_2018_main_report.pdf. Accessed 20 Mar 2021.
Ledder O, Catto-Smith AG, Oliver MR, Alex G, Cameron DJS, Hardikar W. Clinical Patterns and outcome of early-onset inflammtory bowel disease. JPGN. 2014;59:562–4.
Robert ME, Tang L, Hao LM, Mugica-Reyes M. Patterns of inflammation in mucosal biopsies of ulcerative colitis: perceived differences in pediatric popula-tions are limited to children younger than 10 years. Am J Surg Pathol. 2004;28:183–9.
Long MD, Crandall WV, Leibowitz IH, Duffy L, del Rosario F, Kim SC, et al. Prevalence and epidemiology of overweight and obesity in children with inflammatory bowel disease. Inflamm Bowel Dis. 2012;17:2162–8.
Carbonell FRM, Chandan CO. Body mass index at presenttion inflammatory bowel disease in children. PGHN. 2020;23:439–46.
Thayu M, Shults J, Burnham JM, Zemel BS, Baldassano RN, Leonard MB. Gender differences in body compositions deficits at diagnosis in children and adolescents with crohn’s disease. Inflamm Bowel Dis. 2009;13:1121–8.
Bischoff SC, Escher J, Hebuterne X, Stanislaw K, Krznaric Z. et al. ESPEN practical guideline: clinical nutrition in inflammatory bowel disease. Clin Nutr. 2020;39:632–53.
Miele E, Shamir R, Aloi M, Assa A, Braegger C, Bronsky J, et al. Nutrition in pediatric inflammatory bowel disease: a position paper on behalf of the Porto Inflammatory Bowel Disease Group of European Society of Pediatric Gastroenterology, Hepatology and Nutrition. JPGN. 2018;66:686–708.
Cucinotta U, Romano C, Dipasquale V. Diet and nutrition in pediatric inflammatory bowel diseases. Nutrients. 2021;13:655.
Santos GM, Silva LR, Santan GO. Nutritional impact of inflammatory bowel diseases on children and adolescents. Rev Paul Pediatr. 2014;32:403–11.
Wine E, Reif SS, Leshinsky-Silver E, Weiss B, Shaoul RR, Shamir R, et al. Pediatric Crohn’s disease and growth retardation: the role of genotype, phenotype, and disease severity. Pediatrics. 2004;114:1281–6.
Balestrieri P, Ribolsi M, Guarino MPL, Emerenziani S, Altomare M, Cicala M. Nutritional aspect in inflammatory bowel disease. Nutrients. 2020;12:372.
Sulkanen E, Repo M, Huhtala H, Hiltunen P, Kurppa K. Impact of diagnostic delay to the clinical presentation and associated factors in pediatric inflammatory bowel disease: a retrospective study. BMC Gastroenterol. 2021;21:364.
Ricciuto A, Mack DR, Huynh HQ, Jacobson K, Otley AR, DeBruyn J, et al. Diagnostic delay is associated with complicated disease and growth impairment in paediatric Crohn’s disease. J Crohn’s Colitis. 2021;15:419–31.
Schoepfer A, Santos J, Fournier N, Schibli S, Spalinger J, Vavricka S, et al. Systematic analysis of the impact of diagnostic delay on bowel damage in paediatric versus adult onset Crohn’s disease. J Crohn’s Colitis. 2019;13:1334–42.
Gupta N, Bostrom AG, Kirschner BS, Ferry GD, Winter HS, Baldassano RN, et al. Gender differences in presentation and course of disease in pediatric patients with Crohn disease. Pediatrics. 2007;120:e1418–25.
Herzog D, Buehr P, Koller R, Rueger V, Heyland K, Nydegger A, et al. Gender differences in paediatric patients of the swiss ınflammatory bowel disease cohort study. PGHN. 2014;17:147–54.
Lee GJ, Kappelman MD, Boyle B, Colletti RB, King E, Pratt JM, et al. Role of sex in the treatment and clinical outcomes of pediatric patients with inflammatory bowel disease. JPGN. 2012;55:701–6.
Acknowledgements
We thank all our patients and their families for consenting to this study. A sincere thank to James Denison for editing and reviewing this manuscript for English language.
Funding
This research was funded by The Society of Turkish Pediatric Gastroenterology, Hepatology, and Nutrition.
Author information
Authors and Affiliations
Consortia
Contributions
All authors were provided data input as a part of a project of Nationwide Registry for Pediatric Inflammatory Bowel Disease (NRPIBD). The specific contribution of each author is listed below: Kuloglu Z was responsible for the study concept and design, analysis, intrepretation of data and drafting of the manuscript. Çetin F was the project manager for the project of NRPIBD. Kansu A was responsible for critical review of manuscript. ED was responsible for the statistic analysis. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study protocol was approved by Ege University Ethics Committee (October 12, 2011, No: 11-7/2).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kuloglu, Z., Çetin, F., Urgancı, N. et al. Nutritional characteristic of children with inflammatory bowel disease in the nationwide inflammatory bowel disease registry from the Mediterranean region. Eur J Clin Nutr 76, 1289–1296 (2022). https://doi.org/10.1038/s41430-022-01094-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01094-6
This article is cited by
-
Analysis and prediction of nutritional outcome of patients with pediatric inflammatory bowel disease from Bahrain
BMC Pediatrics (2024)
-
Nutritional status of pediatric patients with inflammatory bowel diseases is related to disease duration and clinical picture at diagnosis
Scientific Reports (2023)