Abstract
Objective
Hyperhomocysteinemia (HHcy) and hypertension are associated with cardiovascular events. However, effects of Hcy-lowing interventions on cardiovascular outcome were conflicting. Serum folate level was proposed to be a possible determinant of efficacy of extra folate supplementation on cardiovascular outcome. The aims of the present study were to describe representative information on the levels of serum homocysteine and folate in hypertensive patients, and to explore the major determinants of HHcy.
Methods
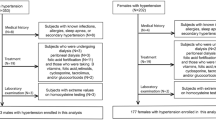
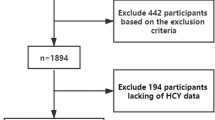
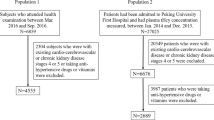
11,007 participants with hypertension were analyzed in this cross-sectional study. Blood pressure and serum levels of biochemical indicators were measured. Multivariate logistic regression model was used to assess the associated factors of HHcy.
Results
Geometric mean of serum total homocysteine was 14.1 (95% CI: 13.9, 14.4) μmol/L and prevalence of HHcy was 36.1 (95% CI: 34.0, 38.1) % in hypertensive patients. HHcy was strongly associated with factors including male sex, older age, elevated serum creatinine (SCr), lower serum folate and vitamin B12, and uncontrolled blood pressure in hypertensive patients. Elevated SCr attributed to HHcy with the etiologic fraction of 0.29. The change of the odds ratio of HHcy associated with folate was significantly higher in patients with elevated SCr compared with that of patients with normal SCr.
Conclusion
The results suggested the protection of female sex and higher levels of folate and vitamin B12 from HHcy and attribution of older age and elevated SCr to HHcy. Restoring renal function deserved attention for hypertensive patients to benefit from Hcy-lowing measures.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data will be available from the corresponding author upon request.
References
Wald DS, Law M, Morris JK. Homocysteine and cardiovascular disease: evidence on causality from a meta-analysis. BMJ. 2002;325:1202.
Homocysteine Studies Collaboration. Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis. JAMA. 2002;288:2015–22.
De Ruijter W, Westendorp RG, Assendelft WJ, den Elzen WP, de Crean AJ, le Cessies S, et al. Use of Framingham risk score and new biomarkers to predict cardiovascular mortality in older people: population based observational cohort study. BMJ. 2009;338:a3083.
Brustolin S, Giugliani R, Felix TM. Genetics of homocysteine metabolism and associated disorders. Braz J Med Biol Res. 2010;43:1–7.
Casas JP, Bautista LE, Smeeth L, Sharma P, Hingorani AD. Homocysteine and stroke: evidence on a causal link from mendelian randomisation. Lancet. 2005;365:224–32.
Martí-Carvajal AJ, Solà I, Lathyris D, Dayer M. Homocysteine-lowering interventions for preventing cardiovascular events. Cochrane Database Syst Rev. 2017;8:CD006612.
Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH) Collaborative Group, Armitage JM, Bowman L, Clarke RJ, Wallendszus K, Bulbulia R, et al. Effects of homocysteine-lowering with folic acid plus vitamin B12 vs placebo on mortality and major morbidity in myocardial infarction survivors: a randomized trial. JAMA. 2010;303:2486–94.
Bønaa KH, Njølstad I, Ueland PM, Schirmer H, Tverdal A, Steigen T, et al. Homocysteine lowering and cardiovascular events after acute myocardial infarction. N Engl J Med. 2006;354:1578–88.
Schnyder G, Roffi M, Flammer Y, Pin R, Hess OM. Effect of homocysteine-lowering therapy with folic acid, vitamin B12, and vitamin B6 on clinical outcome after percutaneous coronary intervention: the Swiss Heart study: a randomized controlled trial. JAMA. 2002;288:973–9.
Hodis HN, Mack WJ, Dustin L, Mahrer PR, Azen SP, Detrano R, et al. High-dose B vitamin supplementation and progression of subclinical atherosclerosis: a randomized controlled trial. Stroke. 2009;40:730–6.
Huo Y, Li J, Qin X, CSPPT Investigators. Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China: the CSPPT randomized clinical trial. JAMA. 2015;313:1325–35.
Selhub J, Jacques PF, Rosenberg IH, Rogers G, Bowman BA, Gunter EW, et al. Serum total homocysteine concentrations in the third National Health and Nutrition Examination Survey (1991-1994): population reference ranges and contribution of vitamin status to high serum concentrations. Ann Intern Med. 1999;131:331–9.
Xu Y, Wang L, He J, Bi Y, Li M, Wang T, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310:948–59.
Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317(Jun):2515–23.
Welch GN, Loscalzo J. Mechanisms of disease: homocysteine and atherothrombosis. N Engl J Med. 1998;338:1042–50.
Stabler SP, Marcell PD, Podell ER, Allen RH, Savage DG, Lindenbaum J. Elevation of total homocysteine in the serum of patients with cobalamin or folate deficiency detected by capillary gas chromatography-mass spectrometry. J Clin Investig. 1988;81:466–74.
Xu X, Qin X, Li Y, Sun D, Wang J, Liang M, et al. Efficacy of folic acid therapy on the progression of chronic kidney disease: the renal substudy of the china stroke primary prevention trial. JAMA Intern Med. 2016;176:1443–50.
Lee YM, Lee MK, Bae SG, Lee SH, Kim SY, Lee DH. Association of homocysteine levels with blood lead levels and micronutrients in the US general population. J Prev Med Public Health. 2012;45:387–93.
Balint B, Jepchumba VK, Guéant JL, Guéant-Rodriguez RM. Mechanisms of homocysteine-induced damage to the endothelial, medial and adventitial layers of the arterial wall. Biochimie. 2020;173:100–6.
Liu LH, Guo Z, Feng M, Wu ZZ, He ZM, Xiong Y. Protection of DDAH2 overexpression against homocysteine-induced impairments of DDAH/ADMA/NOS/NO pathway in endothelial cells. Cell Physiol Biochem. 2012;30:1413–22.
Cheng Z, Jiang X, Pansuria M, Fang P, Mai J, Mallilankaraman K, et al. Hyperhomocysteinemia and hyperglycemia induce and potentiate endothelial dysfunction via mu-calpain activation. Diabetes 2015;64:947–59.
Wu X, Zhang L, Miao Y, Yang J, Wang X, Wang CC, et al. Homocysteine causes vascular endothelial dysfunction by disrupting endoplasmic reticulum redox homeostasis. Redox Biol. 2019;20:46–59.
Sesso HD, Buring JE, Rifai N, Blake GJ, Gaziano JM, Ridker PM. C-reactive protein and the risk of developing hypertension. JAMA 2003;290:2945–51.
Holven KB, Aukrust P, Retterstol K, Hagve TA, Mørkrid L, Ose L, et al. Increased levels of C-reactive proteins and interleukin-6 in hyperhomocysteinemic subjects. Scand J Clin Lab Invest. 2006;66:45–54.
Li T, Chen Y, Li J, Yang X, Zhang H, Qin X, et al. Serum homocysteine concentration is significantly associated with inflammatory/immune factors. PLoS One. 2015;10:e0138099.
Sesso HD, Jiménez MC, Wang L, Ridker PM, Buring JE, Gaziano JM. Plasma inflammatory markers and the risk of developing hypertension in men. J Am Heart Assoc. 2015;4:e001802.
van Dijk SC, Enneman AW, Swart KM, van Wijngaarden JP, Ham AC, de Jonge R, et al. Effect of vitamin B12 and folic acid supplementation on biomarkers of endothelial function and inflammation among elderly individuals with hyperhomocysteinemia. Vasc Med. 2016;21:91–8.
Ruan L, Chen W, Srinivasan SR, Xu J, Toprak A, Berenson GS. Plasma homocysteine is adversely associated with glomerular filtration rate in asymptomatic black and white young adults: the Bogalusa heart study. Eur J Epidemiol. 2009;24:315–9.
Cohen E, Margalit I, Shochat T, Goldberg E, Krause I. Gender differences in homocysteine concentrations, a population-based cross-sectional study. Nutr Metab Cardiovasc Dis. 2019;29:9–14.
Lwin H, Yoshiike N, Yokoyama T, Saito K, Date C, Tanaka H. The relationships between plasma total homocysteine and selected atherosclerotic risk factors according to the C677T methylenetetrahydrofolate reductase gene in Japanese. Eur J Cardiovasc Prev Rehabil. 2005;12:182–4.
Wang Y, Li X, Qin X, Cai Y, He M, Sun L, et al. Prevalence of hyperhomocysteinaemia and its major determinants in rural Chinese hypertensive patients aged 45-75 years. Br J Nutr. 2013;109:1284–93.
Han L, Liu Y, Wang C, Tang L, Feng X, Astell-Burt T, et al. Determinants of hyperhomocysteinemia in healthy and hypertensive subjects: a population-based study and systematic review. Clin Nutr. 2017;36:1215–30.
Ustundag S, Arikan E, Sen S, Esgin H, Ciftci S. The relationship between the levels of plasma total homocysteine and insulin resistance in uncomplicated mild-to-moderate primary hypertension. J Hum Hypertens. 2006;20:379–81.
Han L, Wu Q, Wang C, Hao Y, Zhao J, Zhang L, et al. Homocysteine, ischemic stroke, and coronary heart disease in hypertensive patients: a population-based, prospective cohort study. Stroke 2015;46:1777–86.
Long Y, Nie J. Homocysteine in renal injury. Kidney Dis. 2016;2:80–87.
Schalinske KL, Smazal AL. Homocysteine imbalance: a pathological metabolic marker. Adv Nutr. 2012;3:755–62.
Capelli I, Cianciolo G, Gasperoni L, Zappulo F, Tondolo F, Cappuccilli M, et al. Folic acid and vitamin B12 administration in CKD, why not? Nutrients. 2019;11:383.
Shastry S, Ingram AJ, Scholey JW, James LR. Homocysteine induces mesangial cell apoptosis via activation of p38-mitogen-activated protein kinase. Kidney Int. 2007;71:304–11.
Yi F, Zhang AY, Li N, Muh RW, Fillet M, Renert AF, et al. Inhibition of ceramide-redox signaling pathway blocks glomerular injury in hyperhomocysteinemic rats. Kidney Int. 2006;70:88–96.
Yi F, Li PL. Mechanisms of homocysteine-induced glomerular injury and sclerosis. Am J Nephrol. 2008;28:254–64.
Friedman AN, Bostom AG, Selhub J, Levey AS, Rosenberg IH. The kidney and homocysteine metabolism. J Am Soc Nephrol. 2001;12:2181–9.
Pushpakumar S, Kundu S, Narayanan N, Sen U. DNA hypermethylation in hyperhomocysteinemia contributes to abnormal extracellular matrix metabolism in the kidney. FASEB J. 2015;29:4713–25.
Fischer PA, Dominguez GN, Cuniberti LA, Martinez V, Werba JP, Ramirez AJ, et al. Hyperhomocysteinemia induces renal hemodynamic dysfunction: is nitric oxide involved? J Am Soc Nephrol. 2003;14:653–60.
Ninomiya T, Kiyohara Y, Kubo M, Tanizaki Y, Tanaka K, Okubo K, et al. Hyperhomocysteinemia and the development of chronic kidney disease in a general population: the Hisayama study. Am J Kidney Dis. 2004;44:437–45.
Levi A, Cohen E, Levi M, Goldberg E, Garty M, Krause I. Elevated serum homocysteine is a predictor of accelerated decline in renal function and chronic kidney disease: a historical prospective study. Eur J Intern Med. 2014;25:951–5.
Jamison RL, Hartigan P, Kaufman JS, Goldfarb DS, Warren SR, Guarino PD, et al. Effect of homocysteine lowering on mortality and vascular disease in advanced chronic kidney disease and end-stage renal disease: a randomized controlled trial. JAMA. 2007;298:1163–70.
Mann JF, Sheridan P, McQueen MJ, Held C, Arnold JM, Fodor G, et al. Homocysteine lowering with folic acid and B vitamins in people with chronic kidney disease-results of the renal Hope-2 study. Nephrol Dial Transpl. 2008;23:645–53.
Heinz J, Kropf S, Domröse U, Westphal S, Borucki K, Luley C, et al. B vitamins and the risk of total mortality and cardiovascular disease in end-stage renal disease: results of a randomized controlled trial. Circulation. 2010;121:1432–8.
Acknowledgements
This work was supported by Shanghai Municipal Commission of Health and Family Planning grant 20134129, Shanghai Municipal Health Commission (GWV-7, GWV-10.1-XK05, and GWV-10.1-XK16), and the funding of Innovative research team of high-level local universities in Shanghai and a key laboratory program of the Education Commission of Shanghai Municipality (ZDSYS14005). Shanghai Municipal Center for Disease Control and Prevention also facilitated this research. We greatly appreciate the support of the District Health and Family Planning Commission and the district centers of Disease Control and Prevention.
Author information
Authors and Affiliations
Contributions
MC designed the study. MC and HX wrote the manuscript. XL and QY did the data analysis and interpretation. DZ and YW provided suggestions to the study. YS and CF supervised the study and revised the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheng, M., Xue, H., Li, X. et al. Prevalence of hyperhomocysteinemia (HHcy) and its major determinants among hypertensive patients over 35 years of age. Eur J Clin Nutr 76, 616–623 (2022). https://doi.org/10.1038/s41430-021-00983-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00983-6