Abstract
Objectives
To estimate the association of maternal ADIPOQ gene, dietary habits in early pregnancy, and their interactions with the risk of congenital heart defects (CHDs) in offspring.
Methods
A case-control study of 464 mothers of CHDs children and 504 mothers of healthy children was included. Maternal dietary habits and genetic polymorphisms of ADIPOQ were the main exposure of interest. Their independent effects and interactions in the development of CHDs were analyzed in our study.
Results
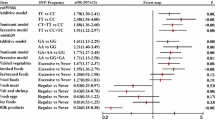
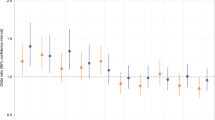
The excessive consumption of pickled vegetables (aOR = 1.58, 95%CI: 1.17–2.12), smoked foods (aOR = 1.84, 95%CI:1.34–2.52), barbecued foods (aOR = 1.62, 95%CI: 1.09–2.39), fish and shrimp (aOR = 0.37, 95%CI: 0.27–50), and milk products (aOR = 0.64, 95%CI: 0.51–80) had a significant association with total CHDs risk. The polymorphisms of ADIPOQ gene at rs1501299 (T/T vs G/G: aOR = 0.27, 95%CI: 0.14–50; G/T vs G/G: aOR = 0.67, 95%CI: 0.46–98) and rs2241766 (G/G vs T/T: aOR = 4.35, 95%CI: 2.23–8.51; T/G vs T/T: aOR = 2.23, 95%CI: 1.51–3.28) showed a significant association with total CHDs risk. Likewise, our results found that maternal dietary habits and ADIPOQ genetic variants also were significantly related to the risk of specific CHDs phenotypes. In addition, gene-diet interaction revealed significant associations between the ADIPOQ gene and maternal dietary habits with total CHDs.
Conclusions
Maternal dietary habits, ADIPOQ gene, and their interactions show a significant association with the risk of CHDs. However, our study has some limitations, thus our findings need to be taken with caution, which highlights that more studies are required to further corroborate our findings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Change history
07 March 2022
The super title has been changed.
References
Triedman JK, Newburger JW. Trends in congenital heart disease the next decade. Circulation. 2016;133:2716–33.
Liu Y, Chen S, Zuhlke L, Black GC, Choy M, Li N, et al. Global birth prevalence of congenital heart defects 1970-2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol. 2019;48:455–63.
Ntiloudi D, Zegkos T, Bazmpani MA, Parcharidou D, Panagiotidis T, Hadjimiltiades S. et al. Pregnancy outcome in women with congenital heart disease: a single-center experience. Hellenic J Cardiol. 2018;59:155–9.
Ntiloudi D, Zegkos T, Koutsakis A, Giannakoulas G, Karvounis H. Pregnancy in Patients with congenital heart disease a contemporary challenge. Cardiol Rev. 2017;25:326–30.
van der Linde D, Konings EEM, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJM, et al. Birth prevalence of congenital heart disease worldwide a systematic review and meta-analysis. J Am Coll Cardiol. 2011;58:2241–7.
Uzark K. Challenges of assessing quality of life in congenital heart disease globally. J Am Coll Cardiol. 2016;67:2246–8.
Zaidi S, Brueckner M. Genetics and genomics of congenital heart disease. Circulation Res. 2017;120:923–40.
van der Bom T, Zomer AC, Zwinderman AH, Meijboom FJ, Bouma BJ, Mulder BJ. The changing epidemiology of congenital heart disease. Nat Rev Cardiol. 2011;8:50–60.
Wang T, Chen L, Yang T, Huang P, Wang L, Zhao L, et al. Congenital heart disease and risk of cardiovascular disease: a meta-analysis of cohort studies. J Am Heart Assoc. 2019;8:e012030.
Gaynor JW, Stopp C, Wypij DB, Andropoulos DB, Atallah J, Atz AM, et al. Neurodevelopmental outcomes after cardiac surgery in infancy. Pediatrics. 2015;135:816–25.
Jenkins KJ, Correa A, Feinstein JA, Botto L, Britt AE, Daniels SR, et al. Noninherited risk factors and congenital cardiovascular defects: current knowledge a scientific statement from the American heart association council on cardiovascular disease in the young. Circulation. 2007;115:2995–3014.
Wesołowska E, Jankowska A, Trafalska E, Kałużny P, Grzesiak M, Dominowska J, et al. Sociodemographic, lifestyle, environmental and pregnancy-related determinants of dietary patterns during pregnancy. Int J Environ Res Public Health. 2019;16:754.
Czeizel A, Dudás I, Vereczkey A, Bánhidy F. Folate deficiency and folic acid supplementation: the prevention of neural-tube defects and congenital heart defects. Nutrients. 2013;5:4760–75.
Smedts HPM, de Vries JH, Rakhshandehroo M, Wildhagen MF, Verkleij-Hagoort AC, Steegers EA, et al. High maternal vitamin E intake by diet or supplements is associated with congenital heart defects in the offspring. Obstetrical Gynecol Surv. 2009;64:301–2.
Verkleij-Hagoort AC, de Vries JHM, Ursem NTC, de Jonge R, Hop WCJ, Steegers-Theunissen RPM. Dietary intake of B-vitamins in mothers born a child with a congenital heart defect. Eur J Nutr. 2006;45:478–86.
Shaw GM, Carmichael SL, Yang W, Lammer EJ. Periconceptional Nutrient intakes and risks of conotruncal heart defects. Birth Defects Res A Clin Mol Teratol. 2010;88:144–51.
Yang J, Kang Y, Cheng Y, Zeng L, Yan H, Dang S. Maternal dietary patterns during pregnancy and congenital heart defects: a case-control study. Int J Environ Res Public Health. 2019;16:2957.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13:3–9.
Ramya K, Ayyappa KA, Ghosh S, Mohan V, Radha V. Genetic association of ADIPOQ gene variants with type 2 diabetes, obesity and serum adiponectin levels in south Indian population. Gene. 2013;532:253–62.
Alfaqih MA, Khader YS, Al-Dwairi AN, Alzoubi A, Al-Shboul O, Hatim A. Lower levels of serum adiponectin and the T allele of rs1501299 of the ADIPOQ gene are protective against polycystic ovarian syndrome in Jordan. Korean J Fam Med. 2018;39:108–13.
Smetnev S, Klimushina M, Kutsenko V, Kiseleva A, Gumanova N, Kots A, et al. Associations of SNPs of the ADIPOQ gene with serum adiponectin levels, unstable angina, and coronary artery disease. Biomolecules. 2019;9:537.
Hivert MF, Manning AK, McAteer JB, Florez JC, Dupuis J, Fox CS, et al. Common variants in the adiponectin gene (ADIPOQ) associated with plasma adiponectin levels, type 2 diabetes, and diabetes-related quantitative traits: the Framingham offspring study. Diabetes. 2008;57:3353–9.
Ong KL, Li M, Tso AW, Xu A, Cherny SS, Sham PC, et al. Association of genetic variants in the adiponectin gene with adiponectin level and hypertension in Hong Kong Chinese. Eur J Endocrinol. 2010;163:251–7.
Chu H, Wang M, Zhong D, Shi D, Ma L, Tong N, et al. AdipoQ polymorphisms are associated with type 2 diabetes mellitus: a meta-analysis study. Diabetes Metab Res Rev. 2013;29:532–45.
Du J, Ye X, Li Q, Yu X, Cheng J, Ma J, et al. Genetic variants in the ADIPOQ gene and the risk of metabolic syndrome: a case-control study of a Chinese Han population. Ann Hum Genet. 2012;76:101–9.
Du W, Li Q, Lu Y, Yu X, Ye X, Gao Y, et al. Genetic variants in ADIPOQ gene and the risk of type 2 diabetes: a case-control study of Chinese Han population. Endocrine. 2011;40:413–22.
Chen L, Yang T, Chen L, Wang L, Wang T, Zhao L, et al. Risk of congenital heart defects in offspring exposed to maternal diabetes mellitus: an updated systematic review and meta-analysis. Arch Gynecol Obstet. 2019;300:1491–506.
Feng Y, Jiang CD, Chang AM, Shi Y, Gao J, Zhu L, et al. Interactions among insulin resistance, inflammation factors, obesity-related gene polymorphisms, environmental risk factors, and diet in the development of gestational diabetes mellitus. J Matern Fetal Neonatal Med. 2019;32:339–47.
Dietrich S, Jacobs S, Zheng JS, Meidtner K, Schwingshackl L, Schulze MB. Gene-lifestyle interaction on risk of type 2 diabetes: a systematic review. Obes Rev. 2019;20:1557–71.
Retamoso VR, Maurer P, Feijoo LB, Tavares G, Manfredini V, Piccoli J. ADIPOQ + 45T>/=G polymorphism, food ingestion, and metabolic syndrome in elderly persons. J Am Coll Nutr. 2018;37:209–14.
Cheng Y, Yan H, Dibley MJ, Shen Y, Li Q, Zeng L. Validity and reproducibility of a semi-quantitative food frequency questionnaire for use among pregnant women in rural China. Asia Pac J Clin Nutr. 2008;17:166–77.
Sotres-Alvarez D, Siega-Riz AM, Herring AH, Carmichael SL, Feldkamp ML, Hobbs CA, et al. Maternal dietary patterns are associated with risk of neural tube and congenital heart defects. Am J Epidemiol. 2013;177:1279–88.
Kalaycioglu Z, Erim FB. Nitrate and nitrites in foods: worldwide regional distribution in view of their risks and benefits. J Agric Food Chem. 2019;67:7205–22.
Machha A, Schechter AN. Dietary nitrite and nitrate: a review of potential mechanisms of cardiovascular benefits. Eur J Nutr. 2011;50:293–303.
Bondonno CP, Croft KD, Hodgson JM. Dietary nitrate, nitric oxide, and cardiovascular health. Crit Rev Food Sci Nutr. 2016;56:2036–52.
Li J, Jia W, Zhao Q. Excessive nitrite affects zebrafish valvulogenesis through yielding too much NO signaling. PLoS ONE. 2014;9:e92728.
Alpert M, Diamond F, Friedhoff AJ. Tremographic studies in Tardive Dyskinesia. Psychopharmacol Bull. 1976;12:5–7.
Jedrychowski W, Perera FP, Tang D, Stigter L, Mroz E, Flak E, et al. Impact of barbecued meat consumed in pregnancy on birth outcomes accounting for personal prenatal exposure to airborne polycyclic aromatic hydrocarbons: birth cohort study in Poland. Nutrition. 2012;28:372–7.
Jules GE, Pratap S, Ramesh A, Hood DB. In utero exposure to benzo(A)pyrene predisposes offspring to cardiovascular dysfunction in later-life. Toxicology 2012;295:56–67.
Huang L, Wang C, Zhang Y, Li J, Zhong Y, Zhou Y, et al. Benzo[a]pyrene exposure influences the cardiac development and the expression of cardiovascular relative genes in Zebrafish (Danio Rerio) Embryos. Chemosphere 2012;87:369–75.
Lupo PJ, Symanski E, Langlois PH, Lawson CC, Malik S, Gilboa SM, et al. Maternal occupational exposure to polycyclic aromatic hydrocarbons and congenital heart defects among offspring in the national birth defects prevention study. Birth Defects Res. 2012;94:875–81.
Li N, Mu Y, Liu Z, Deng Y, Guo Y, Zhang X, et al. Assessment of interaction between maternal polycyclic aromatic hydrocarbons exposure and genetic polymorphisms on the risk of congenital heart diseases. Sci Rep. 2018;8:3075.
Huang M, Jiao J, Wang J, Xia Z, Zhang Y. Characterization of acrylamide-induced oxidative stress and cardiovascular toxicity in zebrafish embryos. J Hazard Mater. 2018;347:451–60.
Mousavi Khaneghah A, Fakhri Y, Nematollahi A, Seilani F, Vasseghian Y. The concentration of acrylamide in different food products: a global systematic review, meta-analysis, and meta-regression. Food Rev. Int. 2020. https://doi.org/10.1080/87559129.2020.1791175.
Olatunji OS, Opeolu BO, Fatoki OS, Ximba BJ. Concentration profile of selected polycyclic aromatic hydrocarbon (PAH) fractions in some processed meat and meat products. J Food Meas Charact. 2013;7:122–8.
Zhang S, Wang L, Yang T, Chen L, Zhao L, Wang T, et al. Parental alcohol consumption and the risk of congenital heart diseases in offspring: an updated systematic review and meta-analysis. Eur J Prev Cardiol. 2020;27:410–21.
Zhao L, Chen L, Yang T, Wang L, Wang T, Zhang S, et al. Parental smoking and the risk of congenital heart defects in offspring: an updated meta-analysis of observational studies. Eur J Prev Cardiol. 2020;27:1284–93.
Pan X, Marklund M, Wu JH. Fish consumption for cardiovascular health: benefits from long-chain omega-3 fatty acids versus potential harms due to mercury. Heart. 2019;105:1384–5.
Chrysant SG, Chrysant GS. An update on the cardiovascular pleiotropic effects of milk and milk products. J Clin Hypertens. 2013;15:503–10.
Woo JG, Dolan LM, Deka R, Kaushal RD, Shen Y, Pal P, et al. Interactions between noncontiguous haplotypes in the adiponectin gene ACDC are associated with plasma adiponectin. Diabetes. 2006;55:523–9.
Yuan HP, Sun L, Li XH, Che FG, Zhu XQ, Yang F, et al. Association of adiponectin polymorphism with metabolic syndrome risk and adiponectin level with stroke. Risk. 2016;6:31945.
Bunin GR, Gyllstrom ME, Brown JE, Kahn EB, Kushi LH. Recall of diet during a past pregnancy. Am J Epidemiol. 2001;154:1136–42.
Acknowledgements
The authors would like to thank the colleagues working in the research group, all subjects who participated in our study, as well as the editors and reviewers who provide us with valuable comments.
Funding
This research was funded by Project Funded by National Natural Science Foundation Program of China (81803313, 81973137, and 82073653), Hunan Provincial Key Research and Development Program (2018SK2063 and 2018SK2062), China Postdoctoral Science Foundation (2020M682644), Hunan Provincial Science and Technology Talent Support Project (2020TJ-N07), Open Project from NHC Key Laboratory of Birth Defect for Research and Prevention (KF2020006), Natural Science Foundation of Hunan Province (2018JJ2551), and Science and Technology Planning Project of Guangdong Province (2020A1414010152).
Author information
Authors and Affiliations
Contributions
Conceptualization, SMZ, XYL, TBY, and JBQ; Formal analysis, SMZ, XYL, TTW, and TBY; Funding acquisition, LZC and JBQ; investigation and methodology, SMZ and TTW; writing-original draft, SMZ, LZC, and JBQ; Writing- review and editing, SMZ, XYL, LZC, and JBQ. All authors have read and approved the final version of the manuscript to be published.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhang, S., Liu, X., Yang, T. et al. Association of maternal dietary habits and ADIPOQ gene polymorphisms with the risk of congenital heart defects in offspring: a hospital-based case-control study. Eur J Clin Nutr 76, 373–381 (2022). https://doi.org/10.1038/s41430-021-00969-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00969-4
This article is cited by
-
Association of polymorphisms of FOLR1 gene and FOLR2 gene and maternal folic acid supplementation with risk of ventricular septal defect: a case-control study
European Journal of Clinical Nutrition (2022)