Abstract
Background
Wholegrains contribute a range of beneficial nutrients, such as dietary fiber and several minerals and vitamins, that are beneficial to depressive symptoms. However, there are a few studies aimed at exploring whether a wholegrain diet is related to depressive symptoms. We conducted this study to investigate the relationship between wholegrains consumption and depressive symptoms.
Methods
This cross-sectional study included a total of 24,776 (mean age: 39.9 years, age range: 18.1–91.3 years; males, 54.1%) inhabitants living in Tianjin, China. Wholegrains consumption was assessed using a valid self-administered food frequency questionnaire. Depressive symptoms were evaluated using the Chinese version of Zung Self-Rating Depression Scale (SDS) and the cutoff point was set at 45. Multiple logistic regression analysis was used to estimate the relationship between wholegrains consumption and depressive symptoms.
Results
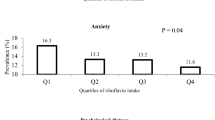
The prevalence of depressive symptoms was 19.1% and 22.4% in males and females, respectively. After adjustments for potential confounding factors, the odds ratios (95% confidence intervals) of depressive symptoms across wholegrains consumption were 0.77 (0.65–0.91) for <1 time/week, 0.73 (0.62–0.86) for 1 time/week and 0.68 (0.59–0.79) for ≥2 time/week in males compared with the control group (almost never). In females, the odds ratios (95% confidence intervals) were 0.86 (0.71–1.04) for <1 time/week, 0.94 (0.78–1.13) for 1 time/week, and 0.76 (0.65–0.91) for ≥2 time/week. Similar results were observed when we use other cut-offs (SDS ≥ 40 and 50) to define depressive symptoms.
Conclusion
This study first demonstrated that the higher consumption of wholegrains might have effects on the prevention and improvement of depressive symptoms. Prospective or intervention studies are needed to confirm these findings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10:e1001547 https://doi.org/10.1371/journal.pmed.1001547. e-pub ahead of print 2013/11/14
Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64:1123–31. https://doi.org/10.1001/archpsyc.64.10.1123. e-pub ahead of print 2007/10/03
Phillips MR, Zhang J, Shi Q, Song Z, Ding Z, Pang S, et al. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001-05: an epidemiological survey. Lancet. 2009;373:2041–53. https://doi.org/10.1016/s0140-6736(09)60660-7. e-pub ahead of print 2009/06/16
Richards DA, Ekers D, McMillan D, Taylor RS, Byford S, Warren FC, et al. Cost and outcome of behavioural activation versus cognitive behavioural therapy for depression (COBRA): a randomised, controlled, non-inferiority trial. Lancet. 2016;388:871–80. https://doi.org/10.1016/S0140-6736(16)31140-0. e-pub ahead of print 2016/07/28
Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3:171–8. https://doi.org/10.1016/S2215-0366(15)00505-2. e-pub ahead of print 2016/02/07
Seal CJ, Nugent AP, Tee ES, Thielecke F. Whole-grain dietary recommendations: the need for a unified global approach. Br J Nutr. 2016;115:2031–8. https://doi.org/10.1017/S0007114516001161. e-pub ahead of print 2016/04/16
AACCI. Whole grain definition. AACCI (American Association of Cereal Chemists International); 1999.
Egeberg R, Frederiksen K, Olsen A, Johnsen NF, Loft S, Overvad K, et al. Intake of wholegrain products is associated with dietary, lifestyle, anthropometric and socio-economic factors in Denmark. Public Health Nutr. 2009;12:1519–30. https://doi.org/10.1017/s1368980008004576. e-pub ahead of print 2009/02/07
Mlyniec K, Nowak G. Zinc deficiency induces behavioral alterations in the tail suspension test in mice. Effect of antidepressants. Pharm Rep. 2012;64:249–55. https://doi.org/10.1016/s1734-1140(12)70762-4. e-pub ahead of print 2012/06/05
Wang J, Um P, Dickerman BA, Liu J Zinc. Magnesium, selenium and depression: a review of the evidence, potential mechanisms and implications. Nutrients. 2018; 10. e-pub ahead of print 2018/05/12; https://doi.org/10.3390/nu10050584
Young LM, Pipingas A, White DJ, Gauci S, Scholey A. A systematic review and meta-analysis of B vitamin supplementation on depressive symptoms, anxiety, and stress: effects on healthy and ‘At-Risk’ individuals. Nutrients. 2019; 11. e-pub ahead of print 2019/09/19; https://doi.org/10.3390/nu11092232
Swann OG, Kilpatrick M, Breslin M, Oddy WH. Dietary fiber and its associations with depression and inflammation. Nutr Rev. 2020;78:394–411. https://doi.org/10.1093/nutrit/nuz072. e-pub ahead of print 2019/11/22
Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. https://doi.org/10.1001/archpsyc.1965.01720310065008. e-pub ahead of print 1965/01/01
Lee HC, Chiu HF, Wing YK, Leung CM, Kwong PK, Chung DW. The Zung self-rating depression scale: screening for depression among the Hong Kong Chinese elderly. J Geriatr Psychiatry Neurol. 1994;7:216–20. https://doi.org/10.1177/089198879400700404. e-pub ahead of print 1994/10/01
Yang YWG, Pan X. China food composition. Beijing: Peking University Medical Press; 2009.
Zhang S, Fu J, Zhang Q, Liu L, Meng G, Yao Z, et al. Association between nut consumption and non-alcoholic fatty liver disease in adults. Liver Int. 2019;39:1732–41. https://doi.org/10.1111/liv.14164. e-pub ahead of print 2019/06/05
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95. https://doi.org/10.1249/01.MSS.0000078924.61453.FB. e-pub ahead of print 2003/08/06
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–72. https://doi.org/10.1001/jama.289.19.2560. e-pub ahead of print 2003/05/16
Recchia D, Baghdadli A, Lassale C, Brunner E, Verdier JM, Kivimaki M, et al. Associations between long-term adherence to healthy diet and recurrent depressive symptoms in Whitehall II Study. Eur J Nutr. 2020;59:1031–41. https://doi.org/10.1007/s00394-019-01964-z. e-pub ahead of print 2019/04/15
Psaltopoulou T, Sergentanis TN, Panagiotakos DB, Sergentanis IN, Kosti R, Scarmeas N. Mediterranean diet, stroke, cognitive impairment, and depression: a meta-analysis. Ann Neurol. 2013;74:580–91. https://doi.org/10.1002/ana.23944. e-pub ahead of print 2013/05/31
Truswell AS. Cereal grains and coronary heart disease. Eur J Clin Nutr. 2002;56:1–14. https://doi.org/10.1038/sj.ejcn.1601283. e-pub ahead of print 2002/02/13
Costabile A, Klinder A, Fava F, Napolitano A, Fogliano V, Leonard C, et al. Whole-grain wheat breakfast cereal has a prebiotic effect on the human gut microbiota: a double-blind, placebo-controlled, crossover study. Br J Nutr. 2008;99:110–20. https://doi.org/10.1017/S0007114507793923. e-pub ahead of print 2007/09/01
Ge X, Pan J, Liu Y, Wang H, Zhou W, Wang X. Intestinal crosstalk between microbiota and serotonin and its impact on gut motility. Curr Pharm Biotechnol. 2018;19:190–5. https://doi.org/10.2174/1389201019666180528094202. e-pub ahead of print 2018/05/29
Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65:732–41. https://doi.org/10.1016/j.biopsych.2008.11.029. e-pub ahead of print 2009/01/20
Cryan JF, O’Riordan KJ, Cowan CSM, Sandhu KV, Bastiaanssen TFS, Boehme M, et al. The microbiota-gut-brain axis. Physiol Rev. 2019;99:1877–2013. https://doi.org/10.1152/physrev.00018.2018. e-pub ahead of print 2019/08/29
Szewczyk B, Kubera M, Nowak G. The role of zinc in neurodegenerative inflammatory pathways in depression. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:693–701. https://doi.org/10.1016/j.pnpbp.2010.02.010. e-pub ahead of print 2010/02/17
Yary T, Aazami S. Dietary intake of zinc was inversely associated with depression. Biol Trace Elem Res. 2012;145:286–90. https://doi.org/10.1007/s12011-011-9202-y. e-pub ahead of print 2011/09/21
Siwek M, Dudek D, Paul IA, Sowa-Kucma M, Zieba A, Popik P, et al. Zinc supplementation augments efficacy of imipramine in treatment resistant patients: a double blind, placebo-controlled study. J Affect Disord. 2009;118:187–95. https://doi.org/10.1016/j.jad.2009.02.014. e-pub ahead of print 2009/03/13
Cardinali DP, Srinivasan V, Brzezinski A, Brown GM. Melatonin and its analogs in insomnia and depression. J Pineal Res. 2012;52:365–75. https://doi.org/10.1111/j.1600-079X.2011.00962.x. e-pub ahead of print 2011/09/29
Mayberg HS. Limbic-cortical dysregulation: a proposed model of depression. J Neuropsychiatry Clin Neurosci. 1997;9:471–81. https://doi.org/10.1176/jnp.9.3.471. e-pub ahead of print 1997/07/01
Mlyniec K. Zinc in the glutamatergic theory of depression. Curr Neuropharmacol. 2015;13:505–13. https://doi.org/10.2174/1570159x13666150115220617. e-pub ahead of print 2015/09/29
Cameron N, Godino JG, Skipper T, Dillon L, Waalen J, Hill L, et al. Associations between reliable changes in depression and changes in BMI, total body fatness and visceral adiposity during a 12-month weight loss trial. Int J Obes (Lond). 2019;43:1859–62. https://doi.org/10.1038/s41366-018-0272-1. e-pub ahead of print 2018/12/13
Uljarevic M, Hedley D, Rose-Foley K, Magiati I, Cai RY, Dissanayake C, et al. Anxiety and depression from adolescence to old age in autism spectrum disorder. J Autism Dev Disord. 2020;50:3155–65. https://doi.org/10.1007/s10803-019-04084-z. e-pub ahead of print 2019/06/14
Chireh B, Li M, D’Arcy C. Diabetes increases the risk of depression: a systematic review, meta-analysis and estimates of population attributable fractions based on prospective studies. Prev Med Rep. 2019;14:100822 https://doi.org/10.1016/j.pmedr.2019.100822. e-pub ahead of print 2019/03/01
Chan R, Chan D, Woo J. A prospective cohort study to examine the association between dietary patterns and depressive symptoms in older Chinese people in Hong Kong. PLoS ONE. 2014;9:e105760 https://doi.org/10.1371/journal.pone.0105760. e-pub ahead of print 2014/08/26
Acknowledgements
The authors gratefully acknowledge all the people that have made this study.
Funding
This study was supported by grants from China Cohort Consortium (No. CCC2020003) and the National Natural Science Foundation of China (No. 81872611, 81673166), China.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, H., Zhang, S., Meng, G. et al. The consumption of wholegrain is related to depressive symptoms among Chinese adults: a cross-sectional study. Eur J Clin Nutr 76, 126–133 (2022). https://doi.org/10.1038/s41430-021-00917-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00917-2
This article is cited by
-
Relationship between dietary pattern and depressive symptoms: an international multicohort study
International Journal of Behavioral Nutrition and Physical Activity (2023)