Abstract
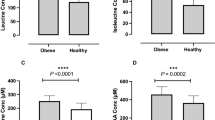
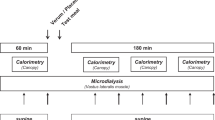
Long-term exposure to high dietary acid load has been associated with insulin resistance and type 2 diabetes in epidemiological studies. However, it remains unclear whether the acid load of the diet translates to mild metabolic acidosis and whether it is responsible for the impairment in glucose regulation in humans. Previously, in a cross-sectional study we have reported that dietary acid load was not different between healthy individuals with normal weight and those with overweight/obesity, irrespective of insulin sensitivity. However, 4-week high acid load diet increased plasma lactate (a small component of the anion gap) and increased insulin resistance in healthy participants. The change in plasma lactate correlated significantly with the change in insulin resistance. Because cause-and-effect could not be evaluated in these settings, we sought to directly test the effect of an alkalizing treatment preload on postprandial glucose regulation. In a randomized placebo-controlled study with a crossover design, we administered sodium bicarbonate (NaHCO3, 1.68 g) prior to high acid load meal to healthy individuals. We found that while the bicarbonate preload attenuated the post meal decrease in pH observed with placebo, no effect on postprandial glucose regulation (glucose, insulin, and C-peptide) was observed. Following 3-month treatment of nondiabetic individuals with bicarbonate, others have reported no change in insulin resistance markers, consistent with our findings. Together, studies in human suggest that insulin resistance associated with longstanding obesogenic diet may be mediated by mild metabolic acidosis. However, buffering the Western diet with bicarbonate and increasing body pH does not change glucose homeostasis in nondiabetic individuals. Further studies are required to shed light on the role of body acid–base balance and glucose homeostasis in health and disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27. https://doi.org/10.1056/NEJMoa1614362.
Pearson-Stuttard J, Zhou B, Kontis V, Bentham J, Gunter MJ, Ezzati M. Worldwide burden of cancer attributable to diabetes and high body-mass index: a comparative risk assessment. Lancet Diabetes Endocrinol. 2018;6:e6–15. https://doi.org/10.1016/S2213-8587(18)30150-5.
Johannsen DL, Tchoukalova Y, Tam CS, Covington JD, Xie W, Schwarz JM, et al. Effect of 8 weeks of overfeeding on ectopic fat deposition and insulin sensitivity: testing the “adipose tissue expandability” hypothesis. Diabetes Care. 2014;37:2789–97. https://doi.org/10.2337/dc14-0761.
Samocha-Bonet D, Campbell LV, Viardot A, Freund J, Tam CS, Greenfield JR, et al. A family history of type 2 diabetes increases risk factors associated with overfeeding. Diabetologia. 2010;53:1700–8. https://doi.org/10.1007/s00125-010-1768-y.
Magkos F, Fraterrigo G, Yoshino J, Luecking C, Kirbach K, Kelly SC, et al. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab. 2016;23:591–601. https://doi.org/10.1016/j.cmet.2016.02.005.
Adeva MM, Souto G. Diet-induced metabolic acidosis. Clin Nutr. 2011;30:416–21. https://doi.org/10.1016/j.clnu.2011.03.008.
Kiefte-de Jong JC, Li Y, Chen M, Curhan GC, Mattei J, Malik VS, et al. Diet-dependent acid load and type 2 diabetes: pooled results from three prospective cohort studies. Diabetologia. 2017;60:270–9. https://doi.org/10.1007/s00125-016-4153-7.
Williams RS, Kozan P, Samocha-Bonet D. The role of dietary acid load and mild metabolic acidosis in insulin resistance in humans. Biochimie. 2016;124:171–7. https://doi.org/10.1016/j.biochi.2015.09.012.
Remer T, Dimitriou T, Manz F. Dietary potential renal acid load and renal net acid excretion in healthy, free-living children and adolescents. Am J Clin Nutr. 2003;77:1255–60. https://doi.org/10.1093/ajcn/77.5.1255.
Archer E, Hand GA, Blair SN. Validity of U.S. nutritional surveillance: National Health and Nutrition Examination Survey caloric energy intake data, 1971–2010. PLoS ONE. 2013;8:e76632. https://doi.org/10.1371/journal.pone.0076632.
DeFronzo RA, Beckles AD. Glucose intolerance following chronic metabolic acidosis in man. Am J Physiol. 1979;236:E328–34. https://doi.org/10.1152/ajpendo.1979.236.4.E328.
Reaich D, Graham KA, Channon SM, Hetherington C, Scrimgeour CM, Wilkinson R, et al. Insulin-mediated changes in PD and glucose uptake after correction of acidosis in humans with CRF. Am J Physiol. 1995;268:E121–6. https://doi.org/10.1152/ajpendo.1995.268.1.E121.
Mandel EI, Curhan GC, Hu FB, Taylor EN. Plasma bicarbonate and risk of type 2 diabetes mellitus. CMAJ. 2012;184:E719–25. https://doi.org/10.1503/cmaj.120438.
Lovejoy J, Newby FD, Gebhart SSP, DiGirolamo M. Insulin resistance in obesity is associated with elevated basal lactate levels and diminished lactate appearance following intravenous glucose and insulin. Metabolism. 1992;41:22–7.
Crawford SO, Hoogeveen RC, Brancati FL, Astor BC, Ballantyne CM, Schmidt MI, et al. Association of blood lactate with type 2 diabetes: the atherosclerosis risk in Communities Carotid MRI Study. Int J Epidemiol. 2010;39:1647–55. https://doi.org/10.1093/ije/dyq126.
Juraschek SP, Selvin E, Miller ER, Brancati FL, Young JH. Plasma lactate and diabetes risk in 8045 participants of the atherosclerosis risk in communities study. Ann Epidemiol. 2013;23:791–6.e794. https://doi.org/10.1016/j.annepidem.2013.09.005.
Farwell WR, Taylor EN. Serum bicarbonate, anion gap and insulin resistance in the National Health and Nutrition Examination Survey. Diabet Med. 2008;25:798–804. https://doi.org/10.1111/j.1464-5491.2008.02471.x.
Samocha-Bonet D, Dixit VD, Kahn CR, Leibel RL, Lin X, Nieuwdorp M, et al. Metabolically healthy and unhealthy obese-the 2013 Stock Conference report. Obes Rev. 2014;15:697–708. https://doi.org/10.1111/obr.12199.
Williams RS, Heilbronn LK, Chen DL, Coster AC, Greenfield JR, Samocha-Bonet D, et al. Dietary acid load, metabolic acidosis and insulin resistance—lessons from cross-sectional and overfeeding studies in humans. Clin Nutr. 2016;35:1084–90. https://doi.org/10.1016/j.clnu.2015.08.002.
Tam CS, Viardot A, Clement K, Tordjman J, Tonks K, Greenfield JR, et al. Short-term overfeeding may induce peripheral insulin resistance without altering subcutaneous adipose tissue macrophages in humans. Diabetes. 2010;59:2164–70. https://doi.org/10.2337/db10-0162.
Samocha-Bonet D, Campbell LV, Mori TA, Croft KD, Greenfield JR, Turner N, et al. Overfeeding reduces insulin sensitivity and increases oxidative stress, without altering markers of mitochondrial content and function in humans. PLoS ONE. 2012;7:e36320. https://doi.org/10.1371/journal.pone.0036320.
Brons C, Jensen CB, Storgaard H, Hiscock NJ, White A, Appel JS, et al. Impact of short-term high-fat feeding on glucose and insulin metabolism in young healthy men. J Physiol. 2009;587(Pt 10):2387–97. https://doi.org/10.1113/jphysiol.2009.169078.
Erdmann J, Kallabis B, Oppel U, Sypchenko O, Wagenpfeil S, Schusdziarra V. Development of hyperinsulinemia and insulin resistance during the early stage of weight gain. Am J Physiol Endocrinol Metab. 2008;294:E568–75. https://doi.org/10.1152/ajpendo.00560.2007.
Souto G, Donapetry C, Calvino J, Adeva MM. Metabolic acidosis-induced insulin resistance and cardiovascular risk. Metab Syndr Relat Disord. 2011;9:247–53. https://doi.org/10.1089/met.2010.0108.
Berkemeyer S. Acid-base balance and weight gain: are there crucial links via protein and organic acids in understanding obesity? Med Hypotheses. 2009;73:347–56. https://doi.org/10.1016/j.mehy.2008.09.059.
Fenton TR, Huang T. Systematic review of the association between dietary acid load, alkaline water and cancer. BMJ Open. 2016;6:e010438. https://doi.org/10.1136/bmjopen-2015-010438.
Kozan P, Blythe JC, Greenfield JR, Samocha-Bonet D. The effect of buffering high acid load meal with sodium bicarbonate on postprandial glucose metabolism in humans—a randomized placebo-controlled study. Nutrients. 2017;9. https://doi.org/10.3390/nu9080861.
Harris SS, Dawson-Hughes B. No effect of bicarbonate treatment on insulin sensitivity and glucose control in non-diabetic older adults. Endocrine. 2010;38:221–6. https://doi.org/10.1007/s12020-010-9377-6.
Acknowledgements
We thank our study participants and the members of the Clinical Insulin Resistance group at the Garvan Institute of Medical Research.
Funding
The clinical studies performed in Samocha-Bonet’s laboratory were funded by Diabetes Australia Research Program and the Garvan Research Foundation, Sydney, Australia. This article is published as part of a supplement sponsored by NuOmix-Research k.s. The conference was financially supported by Protina Pharmazeutische GmbH, Germany and Sirius Pharma, Germany, and organized by NuOmix-Research k.s. Neither company had any role in writing of the paper.
Author information
Authors and Affiliations
Contributions
DS-B conceived some of the clinical studies reported in the review, presented the findings at the 3rd International Acid–Base Symposium, and wrote the report. EC contributed to writing and reviewed the report.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chalmers, E., Samocha-Bonet, D. The effect of body acid–base state and manipulations on body glucose regulation in human. Eur J Clin Nutr 74 (Suppl 1), 20–26 (2020). https://doi.org/10.1038/s41430-020-0692-6
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-0692-6