Abstract
Background/objectives
The impact of gastrointestinal surgery on the profile of the human gut microbiome is not fully understood. This review aimed to identify whether there is a change to the profile of the gut microbiome as a result of gastrointestinal surgery.
Subjects/methods
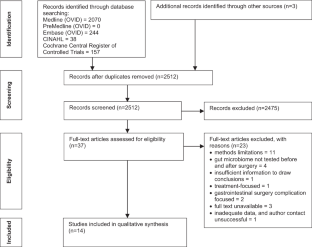
In August 2018, a systematic literature search was conducted in Medline, PreMedline, Embase, CINAHL and The Cochrane Register of Clinical Trials, identifying and critically appraising studies which investigated changes to gut microbiome pre- and post-gastrointestinal surgery.
Results
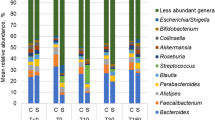
Of 2512 results, 14 studies were included for analysis. All studies reported post-surgical change to the microbiome. In 9 of the 14 studies, prevalence of specific bacteria had significantly changed after surgery. Improved outcome was associated with higher levels of beneficial bacteria and greater microbiome diversity post-surgery.
Conclusion
There were methodological limitations in the included studies leading to uncertainty regarding the impact of gastrointestinal surgery alone on the microbiome profile. An ideal future model for research should encompass case-controlled or cohort design with longer term follow-up in a homogeneous patient group. Future research should seek to clarify the gold standard testing method and standardised timing for post-surgical microbiome sample collection. It is imperative that controls for confounders be put in place to attempt to identify the true association between gastrointestinal surgery and changes to gut microbiome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Whelan K. Modification of the gastrointestinal microbiota and its application to clinical nutrition. J Hum Nutr Diet. 2012;25:297–9.
Peat CM, Kleiman SC, Bulik CM, Carroll IM. The intestinal microbiome in bariatric surgery patients. Eur Eat Disord Rev. 2015;23:496–503.
Singh RK, Chang H-W, Yan D, Lee KM, Ucmak D, Wong K, et al. Influence of diet on the gut microbiome and implications for human health. J Transl Med. 2017;15:73.
Sidhu M, van der Poorten D. The gut microbiome. Aust Fam Physician 2017;46:206–11.
Bäckhed F, Fraser Claire M, Ringel Y, Sanders ME, Sartor RB, Sherman PM, et al. Defining a healthy human gut microbiome: current concepts, future directions, and clinical applications. Cell Host Microbe 2012;12:611–22.
Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486:207–14.
Hollister EB, Gao C, Versalovic J. Compositional and functional features of the gastrointestinal microbiome and their effects on human health. Gastroenterology. 2014;146:1449–58.
Zheng S, Shao S, Qiao Z, Chen X, Piao C, Yu Y, et al. Clinical parameters and gut microbiome changes before and after surgery in thoracic aortic dissection in patients with gastrointestinal complications. Sci Rep. 2017;7:15228.
Zhang Y-J, Li S, Gan R-Y, Zhou T, Xu D-P, Li H-B. Impacts of gut bacteria on human health and diseases. Int J Mol Sci. 2015;16:7493–519.
McIlroy J, Ianiro G, Mukhopadhya I, Hansen R, Hold GL. Review article: the gut microbiome in inflammatory bowel disease—avenues for microbial management. Aliment Pharmacol Ther. 2018;47:26–42.
Wexler HM. Bacteroides: the good, the bad, and the nitty-gritty. Clin Microbiol Rev. 2007;20:593–621.
Duvallet C, Gibbons SM, Gurry T, Irizarry RA, Alm EJ. Meta-analysis of gut microbiome studies identifies disease-specific and shared responses. Nat Commun. 2017;8:1784.
Guyton K, Alverdy JC. The gut microbiota and gastrointestinal surgery. Nat Rev Gastroenterol Hepatol. 2016;14:43–54.
Scotti E, Boué S, Lo Sasso G, Zanetti F, Belcastro V, Poussin C, et al. Exploring the microbiome in health and disease: implications for toxicology. Toxicol Res Appl. 2017;1:1–37.
Galperin MY. Genome diversity of spore-forming firmicutes. Microbiol Spectr. 2013; 1: TBS-0015-2012. https://doi.org/10.1128/microbiolspectrum.TBS-0015-2012.
Mizuta M, Endo I, Yamamoto S, Inokawa H, Kubo M, Udaka T, et al. Perioperative supplementation with bifidobacteria improves postoperative nutritional recovery, inflammatory response, and fecal microbiota in patients undergoing colorectal surgery: a prospective, randomized clinical trial. Biosci Microbiota Food Health. 2016;35:77–87.
Neut C, Guillemot F, Colombel JF. Nitrate-reducing bacteria in diversion colitis: a clue to inflammation? Dig Dis Sci. 1997;42:2577–80.
Ventura M, Canchaya C, Tauch A, Chandra G, Fitzgerald GF, Chater KF, et al. Genomics of actinobacteria: tracing the evolutionary history of an ancient phylum. Microbiol Mol Biol Rev. 2007;71:495–548.
Barka EA, Vatsa P, Sanchez L, Gaveau-Vaillant N, Jacquard C, Klenk HP, et al. Taxonomy, physiology, and natural products of actinobacteria. Microbiol Mol Biol Rev. 2015;80:1–43.
Stavrou G, Kotzampassi K. Gut microbiome, surgical complications and probiotics. Ann Gastroenterol. 2017;30:45–53.
Chen YPL. Bioinformatics for whole-genome shotgun sequencing of microbial communities. PLoS Comput Biol. 2005;1:e24.
Morgan XC, Huttenhower C. Meta’omic analytic techniques for studying the intestinal microbiome. Gastroenterology. 2014;146:1437–48.e1.
Valdes AM, Walter J, Segal E, Spector TD. Role of the gut microbiota in nutrition and health. Br J Med. 2018;361(Supp 1):36–44.
Joanna Briggs Institute. Critical appraisal tools. 2018. http://joannabriggs.org/research/critical-appraisal-tools.html. Accessed 2 Oct 2018.
Joanna Briggs Institute. The JBI approach. 2018. http://joannabriggs.org/jbi-approach.html#tabbed-nav=Levels-of-Evidence. Accessed 2 Oct 2018.
Almeida MG, Kiss DR, Zilberstein B, Quintanilha AG, Teixeira MG, Habr-Gama A. Intestinal mucosa-associated microflora in ulcerative colitis patients before and after restorative proctocolectomy with an ileoanal pouch. Dis Colon Rectum. 2008;51:1113–9.
Neut C, Bulois P, Desreumaux P, Membre JM, Lederman E, Gambiez L, et al. Changes in the bacterial flora of the neoterminal ileum after ileocolonic resection for Crohn’s disease. Am J Gastroenterol. 2002;97:939–46.
Sokol H, Pigneur B, Watterlot L, Lakhdari O, Bermúdez-Humarán LG, Gratadoux JJ, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci USA. 2008;105:16731–6.
Marteau P, Lémann M, Seksik P, Laharie D, Colombel JF, Bouhnik Y, et al. Ineffectiveness of Lactobacillus johnsonii LA1 for prophylaxis of postoperative recurrence in Crohn’s disease: a randomised, double blind, placebo controlled GETAID trial. Gut. 2006;55:842–7.
De Cruz P, Kang S, Wagner J, Buckley M, Sim WH, Prideaux L, et al. Association between specific mucosa-associated microbiota in Crohn’s disease at the time of resection and subsequent disease recurrence: a pilot study. J Gastroenterol Hepatol. 2015;30:268–78.
Dey N, Soergel DA, Repo S, Brenner SE. Association of gut microbiota with postoperative clinical course in Crohn’s disease. BMC Gastroenterol. 2013;13:131.
Laffin M, Perry T, Park H, Gillevet P, Sikaroodi M, Kaplan GG, et al. Endospore-forming bacteria are associated with maintenance of remission following intestinal resection in Crohn’s disease. Gastroenterology. 2017;152:S192–3.
Wright EK, Kamm MA, Wagner J, Teo SM, De Cruz P, Hamilton AL, et al. Microbial factors associated with postoperative Crohn’s disease recurrence. J Crohns Colitis. 2017;11:191–203.
Mondot S, Lepage P, Seksik P, Allez M, Tréton X, Bouhnik Y, et al. The GETAID group. Structural robustness of the gut mucosal microbiota is associated with Crohn’s disease remission after surgery. Gut. 2016;65:954–6.
Feng X, Su Y, Jiang J, Ning L, Weiwei D, Zhiming W, et al. Changes in fecal and colonic mucosal microbiota of patients with refractory constipation after a subtotal colectomy. Am J Surg. 2015;81:198–206.
Ohigashi S, Sudo K, Kobayashi D, Takahashi T, Nomoto K, Onodera H. Significant changes in the intestinal environment after surgery in patients with colorectal cancer. J Gastrointest Surg. 2013;17:1657–64.
Mangell P, Thorlacius H, Syk I, Ahrne S, Molin G, Olsson C, et al. Lactobacillus plantarum 299v does not reduce enteric bacteria or bacterial translocation in patients undergoing colon resection. Dig Dis Sci. 2012;57:1915–24.
Guimaraes Quintanilha AG, Azevedo dos Santos MA, Avila-Campos MJ, Saad WA, Pinotti HW, Zilberstein B. Chagasic megacolon and proximal jejunum microbiota. Scandanivian J Gastroenterol. 2000;35:632–6.
Mariat D, Firmesse O, Levenez F, Guimaraes VD, Sokol H, Dore J, et al. The Firmicutes/Bacteroidetes ratio of the human microbiota changes with age. BMC Microbiol. 2009;9:123.
Kabeerdoss J, Sankaran V, Pugazhendhi S, Ramakrishna BS. Clostridium leptum group bacteria abundance and diversity in the fecal microbiota of patients with inflammatory bowel disease: a case-control study in India. BMC Gastroenterol. 2013;13:20
Toprak NU, Gulluoglu BM, Cakici O, Akin LM, Demirkalem P, Celenk T, et al. Do antimicrobial susceptibility patterns of colonic isolates of Bacteroides species change after antibiotic prophylaxis with cefoxitine during elective abdominal surgery? World J Surg. 2005;29:1311–5.
Okazaki M, Matsukuma S, Suto R, Miyazaki K, Hidaka M, Matsuo M, et al. Perioperative synbiotic therapy in elderly patients undergoing gastroenterological surgery: a prospective, randomized control trial. Nutrition. 2013;29:1224–30.
Vaughn BP, Moss AC. Prevention of post-operative recurrence of Crohn’s disease. World J Gastroenterol. 2014;20:1147–54.
Vuik FER, Dicksved J, Lam SY, Fuhler GM, van der Laan LJW, van de Winkel A, et al. Composition of the mucosa-associated microbiota along the entire gastrointestinal tract of human individuals. United Eur Gastroenterol J. 2019;7:897–907.
Conlon MA, Bird AR. The impact of diet and lifestyle on gut microbiota and human health. Nutrients. 2014;7:17–44.
Vandeputte D, Tito RY, Vanleeuwen R, Falony G, Raes J. Practical considerations for large-scale gut microbiome studies. FEMS Microbiol Rev. 2017;41(Supp 1):S154–67.
Wu GD, Lewis JD, Hoffmann C, Chen YY, Knight R, Bittinger K, et al. Sampling and pyrosequencing methods for characterizing bacterial communities in the human gut using 16S sequence tags. BMC Microbiol. 2010;10:206.
Bahl MI, Bergström A, Licht TR. Freezing fecal samples prior to DNA extraction affects the Firmicutes to Bacteroidetes ratio determined by downstream quantitative PCR analysis. FEMS Microbiol Lett. 2012;329:193–7.
Cowan ST. SK. Manual for idenfication of medical bacteria 2nd ed. New York: Cambridge University Press; 1974.
Sutter VLCD, Finegold SM. Wadsworth anaerobic bacteriology manual. 3rd ed. St. Louis: Mosby; 1980.
Holdeman LVCE, Moore WE. Anaerobic laboratory manual. 4th ed. Blacksburg: Virginia Polytechnics Institute and State University; 1977.
Kang S, Denman SE, Morrison M, Yu Z, McSweeney C. An efficient RNA extraction method for estimating gut microbial diversity by polymerase chain reaction. Current Microbiology. 2009;58:464–71.
Zoetendal EG, Akkermans AD, De Vos WM. Temperature gradient gel electrophoresis analysis of 16S rRNA from human fecal samples reveals stable and host-specific communities of active bacteria. Appl Environ Microbiol. 1998;64:3854–9.
Quednau M, Ahrne S, Petersson AC, Molin G. Identification of clinically important species of Enterococcus within 1 day with randomly amplified polymorphic DNA (RAPD). Curr Microbiol. 1998;36:332–6.
Podschun R, Ullmann U. Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin Microbiol Rev. 1998;11:589–603.
Wagner J, Short K, Catto-Smith AG, et al. Identification and characterisation of Pseudomonas 16S ribosomal DNA from ileal biopsies of children with Crohn’s disease. PLoS ONE. 2008;3:e3578.
Hudault S, Guignot J, Servin AL. Escherichia coli strains colonising the gastrointestinal tract protect germfree mice against Salmonella typhimurium infection. Gut.2001;49:47–55.
Yoshida N, Emoto T, Yamashita T, Watanabe H, Hayashi T, Tabata T, et al. Bacteroides vulgatus and Bacteroides dorei reduce gut microbial lipopolysaccharide production and inhibit atherosclerosis. Circulation. 2018;138:2486–98.
Hehemann JH, Kelly AG, Pudlo NA, Martens EC, Borastona AB. Bacteria of the human gut microbiome catabolize red seaweed glycans with carbohydrate-active enzyme updates from extrinsic microbes. Proc Natl Acad Sci USA. 2012;109:19786–91.
Slattery C, Cotter PD, O’Toole PW. Analysis of health benefits conferred by Lactobacillus species from kefir. Nutrients. 2019;11:1252–76.
Cools P, Melin P. Group B Streptococcus and perinatal mortality. Res Microbiol. 2017;168:793–801.
NB Corrêa, LA Filho Péret, Penna FJ, Lima FM, Nicoli JR. A randomized formula controlled trial of Bifidobacterium lactis and Streptococcus thermophilus for prevention of antibiotic-associated diarrhea in infants. J Clin Gastroenterol. 2005;39:385–9.
Eberhard J, Stumpp N, Winkel A, Schrimpf C, Bisdas T, Orzak P, et al. Streptococcus mitis and Gemella haemolysans were simultaneously found in atherosclerotic and oral plaques of elderly without periodontitis-a pilot study. Clin Oral Investig. 2017;21:447–52.
Adam EL, Siciliano RF, Gualandro DM, Calderaro D, Issa VS, Rossi F, et al. Case series of infective endocarditis caused by Granulicatella species. Int J Infect Dis. 2015;31:56–58.
Cuiv PO, Klaassens ES, Durkin AS, Harkins DM, Foster L, McCorrison J, et al. Draft genome sequence of Turicibacter sanguinis PC909, isolated from human feces. J Bacteriol. 2011;193:1288–9.
Bibbò S, Riccardo Lopetuso L, Ianiro G, Di Rienzo T, Gasbarrini A, et al. Role of microbiota and innate immunity in recurrent Clostridium difficile infection. J Immunol Research. 2014;2014:462740.
Kanauchi O, Matsumoto Y, Matsumura M, Fukuoka M, Bamba T. The beneficial effects of microflora, especially obligate anaerobes, and their products on the colonic environment in inflammatory bowel disease. Curr Pharm Des. 2005;11:1047–53.
de la Cuesta-Zuluaga J, Mueller NT, Corrales-Agudelo V, Velásquez-Mejía EP, Carmona JA, Abad JM, et al. Metformin is associated with higher relative abundance of mucin-degrading Akkermansia muciniphila and several short-chain fatty acid–producing microbiota in the gut. Diabetes Care. 2017;40:54–62.
Workneh M, Wang F, Romagnoli M, Simner PJ, Carroll K. Bypass graft infection and bacteremia caused by Anaerostipes caccae: First report of human infection caused by a recently described gut anaerobe. Anaerobe. 2016;42:98–100.
Schwiertz A, Hold GL, Duncan SH, Gruhl B, Collins MD, Lawson PA, et al. Anaerostipes caccae gen. nov., sp. nov., a new saccharolytic, acetate-utilising, butyrate-producing bacterium from human faeces. Syst Appl Microbiol. 2002;25:46–51.
Ahn J, Sinha R, Pei Z, Dominianni C, Wu J, Shi J, et al. Human gut microbiome and risk for colorectal cancer. J Natl Cancer Inst. 2013;105:1907–11.
Linares DM, Ross P, Stanton C. Beneficial microbes: the pharmacy in the gut. Bioengineered. 2015;7:11–20.
Buchanan M. Sizing up bacteria. Nat Phys. 2014;10:788.
Author information
Authors and Affiliations
Contributions
SC was responsible for conceptualisation of the study. AW, SF and SC were responsible for designing study. SC, SF and AW conducted the search, quality assessments and analysis of results. BW, SF and CT were responsible for reviewing the analysis. SF led the interpretation of results with all authors having involvement. AW and SF drafted the paper and all authors contributed to reviewing the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ferrie, S., Webster, A., Wu, B. et al. Gastrointestinal surgery and the gut microbiome: a systematic literature review. Eur J Clin Nutr 75, 12–25 (2021). https://doi.org/10.1038/s41430-020-0681-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-0681-9