Abstract
Background
Children in China with Autism Spectrum Disorders (ASD) are prone to vitamin A deficiency (VAD). The present study compared two vitamin A supplements (VAS) in two groups of children with ASD and VAD to explore a better VAS program for children with ASD.
Method
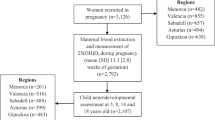
A total of 138 3–8-year-old children with ASD (118 males and 20 females) were enrolled in this 6-month study. Of these 138 children, 82 who had VAD (ASD-VAD) were divided into two VAS groups that received the recommended VAS program (RNI-VAS) or a weekly dose of VAS (WD-VAS). The 56 children who had normal vitamin A levels (ASD-VAN) served as a control group. The Social Responsiveness Scale (SRS) was used to assess the severity of social impairment before and after the interventions. Their serum retinol (VA) and oxytocin (OXT) concentrations, the mRNA expression of retinoic acid receptors (RARs), and CD38 gene in peripheral blood was measured before and after the 6-month intervention.
Results
The WD-VAS program increased VA levels better than the RNI-VAS program did (P < 0.01), and it significantly decreased SRS scores (P < 0.05). In addition, the change in VA was positively correlated with the change in mRNA levels in RARβ (r = 0.2441, P = 0.0092), the CD38 in PBMC (r = 0.2729, P = 0.0033), and the change in OXT concentration in serum (r = 0.3735, P < 0.0001). VA was also negatively correlated with changes in SRS scores across the three groups (r = −0.2615, P = 0.0026).
Conclusion
The WD-VAS might be more suitable for children with ASD and VAD than other interventions to improve both VA and social functioning, which may be mediated through the RARβ-CD38-OXT axis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Lord C, Elsabbagh M, Baird G, Veenstra-Vanderweele J. Autism spectrum disorder. Lancet. 2018;392:508–20.
Sun X, Allison C, Wei L, Matthews FE, Auyeung B, Wu YY, et al. Autism prevalence in China is comparable to Western prevalence. Mol Autism. 2019;10:7.
Moody L, Chen H, Pan YX. Early-life nutritional programming of cognition—the fundamental role of epigenetic mechanisms in mediating the relation between early-life environment and learning and memory process. Adv Nutr (Bethesda, Md). 2017;8:337–50.
WHO. Vitamin A Supplements: a guide to their use in the treatment and prevention of vitamin A deficiency and xerophthalmia. 2nd ed. WHO; 1997.
WHO. Global prevalence of vitamin A deficiency in populations at risk 1995–2005. WHO; 2009.
Sun C, Xia W, Zhao Y, Li N, Zhao D, Wu L. Nutritional status survey of children with autism and typically developing children aged 4-6 years in Heilongjiang Province, China. J Nutr Sci. 2013;2:e16-e.
Liu X, Liu J, Xiong X, Yang T, Hou N, Liang X, et al. Correlation between nutrition and symptoms: nutritional survey of children with autism spectrum disorder in Chongqing, China. Nutrients. 2016;8:294.
Shearer KD, Stoney PN, Morgan PJ, McCaffery PJ. A vitamin for the brain. Trends Neurosci. 2012;35:733–41.
Blomhoff R, Green MH, Berg T, Norum KR. Transport and storage of vitamin A. Science. 1990;250:399–404.
Carmona-Mora P, Walz K. Retinoic acid induced 1, RAI1: a dosage sensitive gene related to neurobehavioral alterations including autistic behavior. Curr Genomics. 2010;11:607–17.
Hao Z, Wu Q, Li Z, Li Y, Li Q, Lai X, et al. Maternal exposure to triclosan constitutes a yet unrecognized risk factor for autism spectrum disorders. Cell Res. 2019;29:866–9.
Pavăl D, Rad F, Rusu R, Niculae A-Ş, Colosi HA, Dobrescu I, et al. Low retinal dehydrogenase 1 (RALDH1) level in prepubertal boys with autism spectrum disorder: a possible link to dopamine dysfunction? Clin Psychopharmacol Neurosci. 2017;15:229–36.
Xu X, Li C, Gao X, Xia K, Guo H, Li Y, et al. Excessive UBE3A dosage impairs retinoic acid signaling and synaptic plasticity in autism spectrum disorders. Cell Res. 2018;28:48–68.
Zhou W, Li S. Decreased levels of serum retinoic acid in chinese children with autism spectrum disorder. Psychiatry Res. 2018;269:469–73.
Y A, EM B, M D, WA A, L V, A A, et al. Beta-carotene as a novel therapy for the treatment of “Autistic like behavior” in animal models of Autism. Behav Brain Res. 2019;364:469–79.
Riebold M, Mankuta D, Lerer E, Israel S, Zhong S, Nemanov L, et al. All-trans retinoic acid upregulates reduced CD38 transcription in lymphoblastoid cell lines from Autism spectrum disorder. Mol Med. 2011;17:799–806.
Lai X, Wu X, Hou N, Liu S, Li Q, Yang T, et al. Vitamin A deficiency induces autistic-like behaviors in rats by regulating the RARβ-CD38-oxytocin axis in the hypothalamus. Mol Nutr Food Res. 2018. https://doi.org/10.1002/mnfr.201700754.
Mason J, Greiner T, Shrimpton R, Sanders D, Yukich J. Vitamin A policies need rethinking. Int J Epidemiol. 2015;44:283–92.
Bento C, Matos AC, Cordeiro A, Ramalho A. Vitamin A deficiency is associated with body mass index and body adiposity in women with recommended intake of vitamin A. Nutricion Hosp. 2018;35:1072–8.
Ribeiro-Silva Rde C, Nunes IL, Assis AM. Prevalence and factors associated with vitamin A deficiency in children and adolescents. J Pediatr. 2014;90:486–92.
Bandini LG, Curtin C, Phillips S, Anderson SE, Maslin M, Must A. Changes in food selectivity in children with autism spectrum disorder. J Autism Dev Disord. 2017;47:439–46.
Chinese Nutrition Society, Dietary Guidelines for Chinese (People’s Medical Publishing House, China; 2016).
Bölte S, Poustka F, Constantino JN. Assessing autistic traits: cross-cultural validation of the social responsiveness scale (SRS). Autism Res. 2008;1:354–63.
Chan W, Smith LE, Hong J, Greenberg JS, Mailick MR. Validating the social responsiveness scale for adults with autism. Autism Res. 2017;10:1663–71.
Liu J, Liu X, Xiong XQ, Yang T, Cui T, Hou NL, et al. Effect of vitamin A supplementation on gut microbiota in children with autism spectrum disorders—a pilot study. BMC Microbiol. 2017;17:204.
Fregeau B, Kim BJ, Hernández-García A, Jordan VK, Cho MT, Schnur RE, et al. De novo mutations of RERE cause a genetic syndrome with features that overlap those associated with proximal 1p36 deletions. Am J Hum Genet. 2016;98:963–70.
Funding
This research was funded by the National Nature Science of Foundation of China (81770526, 81771223), the Key Project of Guangdong Province (2018B030335001) and Guangzhou City (202007030002), and the Scientific research innovation program for graduate students of Chongqing (CYB 17107).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lai, X., Zhang, Q., Zhu, J. et al. A weekly vitamin A supplementary program alleviates social impairment in Chinese children with autism spectrum disorders and vitamin A deficiency. Eur J Clin Nutr 75, 1118–1125 (2021). https://doi.org/10.1038/s41430-020-00827-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00827-9
This article is cited by
-
WDR62-deficiency Causes Autism-like Behaviors Independent of Microcephaly in Mice
Neuroscience Bulletin (2023)