Abstract
Objective
The aim of this study was to evaluate the effects of long-term excessive iodine intake on blood lipids in adults.
Methods
Three counties from Dezhou city and Liaocheng city in the Shandong province of China were selected as survey locations. Three to five villages were selected from each county and then categorized by the iodine concentration detected in the groundwater into Low (<10 µg/L), Medium (10–150 µg/L), High (150–300 µg/L), and Excessive (>300 µg/L) groups. A self-reported questionnaire was completed by each subject to provide demographic characteristics. Body height, weight, and blood pressure were recorded by trained staff. Blood lipids were measured.
Results
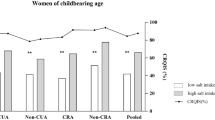
A total of 2156 subjects were recruited for the final analysis. The serum triglyceride (TRIG) was significantly higher in the Excessive group than in the other three groups (P < 0.05). Total cholesterol (TCHOL) and low-density lipoprotein-cholesterol (LDL-C) showed downward trends with the increases in the water iodine concentration. A statistical significance of the crude correlation coefficient was detected between the water iodine concentration and the TRIG, TCHOL, or LDL-C (P < 0.05). A significant correlation was also noted between the water iodine concentration and TCHOL or LDL-C after adjustment for covariates. High iodine concentration was a significant protective factor for TCHOL and LDL-C in adults, whereas elevated BMI and advancing age were risk factors for both variables.
Conclusion
An association was identified between iodine excess and low TCHOL or LDL-C. In areas with excessive iodine, iodine intake should be considered in studies examining the factors that influence blood lipids.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Chen W, Zhang Y, Hao Y, Wang W, Tan L, Bian J, et al. Adverse effects on thyroid of Chinese children exposed to long-term iodine excess: optimal and safe tolerable upper intake levels of iodine for 7- to 14-y-old children. Am J Clin Nutr. 2018;107:780–8. https://doi.org/10.1093/ajcn/nqy011.
Guo Y, Zynat J, Xu Z, Wang X, Osiman R, Zhao H, et al. Iodine nutrition status and thyroid disorders: a cross-sectional study from the Xinjiang autonomous region of China. Eur J Clin Nutr. 2016;70:1332–6. https://doi.org/10.1038/ejcn.2016.82.
Shen H, Liu S, Sun D, Zhang S, Su X, Shen Y, et al. Geographical distribution of drinking-water with high iodine level and association between high iodine level in drinking-water and goitre: a Chinese national investigation. Br J Nutr. 2011;106:243–7. https://doi.org/10.1017/S0007114511000055.
National health Commission of the People’s Republic of China. National Drinking Water Iodine Survey Report. 2019. http://www.nhc.gov.cn/jkj/s5874/201905/bb1da1f5e47040e8820b9378e6db4bd3.shtml. Accessed 7 May 2019.
Wang Y, Cui Y, Chen C, Duan Y, Wu Y, Li W, et al. Stopping the supply of iodized salt alone is not enough to make iodine nutrition suitable for children in higher water iodine areas: a cross-sectional study in northern China. Ecotoxicol Environ Saf. 2020;188:109930 https://doi.org/10.1016/j.ecoenv.2019.109930.
Pearce EN. Iodine deficiency in children. Endocr Dev. 2014;26:130–8. https://doi.org/10.1159/000363160.
Cui Y, Zhang Z, Zhang B, Zhao L, Hou C, Zeng Q, et al. Excessive apoptosis and disordered autophagy flux contribute to the neurotoxicity induced by high iodine in Sprague-Dawley rat. Toxicol Lett. 2018;297:24–33. https://doi.org/10.1016/j.toxlet.2018.08.020.
Katagiri R, Yuan X, Kobayashi S, Sasaki S. Effect of excess iodine intake on thyroid diseases in different populations: a systematic review and meta-analyses including observational studies. PLoS ONE. 2017;12:e0173722. https://doi.org/10.1371/journal.pone.0173722.
Teng W, Shan Z, Teng X, Guan H, Li Y, Teng D, et al. Effect of iodine intake on thyroid diseases in China. N Engl J Med. 2006;354:2783–93. https://doi.org/10.1056/NEJMoa054022.
Sang Z, Chen W, Shen J, Tan L, Zhao N, Liu H, et al. Long-term exposure to excessive iodine from water is associated with thyroid dysfunction in children. J Nutr. 2013;143:2038–43. https://doi.org/10.3945/jn.113.179135.
Aakre I, Strand T, Bjøro T, Norheim I, Barikmo I, Ares S, et al. Thyroid function among breastfed children with chronically excessive iodine intakes. Nutrients. 2016;8:2–12. https://doi.org/10.3390/nu8070398.
Bürgi H. Iodine excess. Best Pract Res Clin Endocrinol Metab. 2010;24:107–15. https://doi.org/10.1016/j.beem.2009.08.010.
Chen R, Li Q, Cui W, Wang X, Gao Q, Zhong C, et al. Maternal iodine insufficiency and excess are associated with adverse effects on fetal growth: a prospective cohort study in Wuhan, China. J Nutr. 2018;148:1814–20. https://doi.org/10.1093/jn/nxy182.
Liu J, Liu L, Jia Q, Zhang X, Jin X, Shen H. Effects of excessive iodine intake on blood glucose, blood pressure, and blood lipids in adults. Biol Trace Elem Res. 2019;192:136–44. https://doi.org/10.1007/s12011-019-01668-9.
Zhou BF. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases–report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed Environ Sci. 2002;15:245–52.
Tran HV, Erskine NA, Kiefe CI, Barton BA, Lapane KL, Do VTH, et al. Is low iodine a risk factor for cardiovascular disease in Americans without thyroid dysfunction? Findings from NHANES. Nutr Metab Cardiovasc Dis. 2017;27:651–6. https://doi.org/10.1016/j.numecd.2017.06.001.
Mancini FR, Rajaobelina K, Dow C, Habbal T, Affret A, Balkau B, et al. High iodine dietary intake is associated with type 2 diabetes among women of the E3N-EPIC cohort study. Clin Nutr. 2019;38:1651–6. https://doi.org/10.1016/j.clnu.2018.08.015.
Zhao SJ, Ye Y, Sun FJ, Tian EJ, Chen ZP. The impact of dietary iodine intake on lipid metabolism in mice. Biol Trace Elem Res. 2011;142:581–8. https://doi.org/10.1007/s12011-010-8767-1.
Zhang Y. Effects of different dose of potassium iodide and iodate on antioxidant ability of the blood plasma, lipid metabolism of the blood and thyroid function in rats. The Dissertation of China Center for Disease Control and Prevention. 2013.
Liu M, Li SM, Li XW, Li SH, Wang PH, Liang P. Exploratory research of epidemiological association between iodine excess intake and abnormal blood pressure. Chin J Control Endemic Disenaces. 2009;24:408–10.
Herter-Aeberli I, Cherkaoui M, El Ansari N, Rohner R, Stinca S, Chabaa L, et al. Iodine supplementation decreases hypercholesterolemia in iodine-deficient, overweight women: a randomized controlled trial. J Nutr. 2015;145:2067–75. https://doi.org/10.3945/jn.115.213439.
Zimmermann MB, Aeberli I, Melse-Boonstra A, Grimci L, Bridson J, Chaouki N, et al. Iodine treatment in children with subclinical hypothyroidism due to chronic iodine deficiency decreases thyrotropin and C-peptide concentrations and improves the lipid profile. Thyroid. 2009;19:1099–104. https://doi.org/10.1089/thy.2009.0001.
Danese MD, Ladenson PW, Meinert CL, Powe NR. Effect of thyroxine therapy on serum lipoproteins in patients with mild thyroid failure: a quantitative review of the literature. J Clin Endocrinol Metab. 2000;85:2993–3001. https://doi.org/10.1210/jcem.85.9.6841.
Villar HCCE, Saconato H, Valente O, Atallah AN. Thyroid hormone replacement for subclinical hypothyroidism. Cochrane Database Syst Rev. 2007;3:CD003419. https://doi.org/10.1002/14651858.CD003419.pub2.
Sasaki S, Kawai K, Honjo Y, Nakamura H. Thyroid hormones and lipid metabolism. Nippon Rinsho. 2006;64:2323–9.
Kang MJ, Hwang IT, Chung HR. Excessive iodine intake and subclinical hypothyroidism in children and adolescents aged 6–19 years: results of the sixth Korean National Health and Nutrition Examination Survey, 2013–2015. Thyroid. 2018;28:773–9. https://doi.org/10.1089/thy.2017.0507.
Han H, Xin P, Zhao L, Xu J, Xia Y, Yang X, et al. Excess iodine and high-fat diet combination modulates lipid profile, thyroid hormone, and hepatic LDLr expression values in mice. Biol Trace Elem Res. 2012;147:233–9. https://doi.org/10.1007/s12011-011-9300-x.
Hertelyova Z, Salaj R, Chmelarova A, Dombrovsky P, Dvorakova MC, Kruzliak P. The association between lipid parameters and obesity in university students. J Endocrinol Investig. 2016;39:769–78. https://doi.org/10.1007/s40618-015-0240-8.
Koukkou EG, Roupas ND, Markou KB. Effect of excess iodine intake on thyroid on human health. Minerva Med. 2017;108:136–46. https://doi.org/10.23736/S0026-4806.17.04923-0.
Funding
Supported by the Chinese National Natural Science Foundation (No. 81273016).
Author information
Authors and Affiliations
Contributions
JB and XL designed the research. JG, MZ, XW, BZ, MW, WJ, and JB conducted the research. JG and XL analyzed the data and wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gao, J., Zhang, M., Wang, X. et al. Effects of long-term excessive iodine intake on blood lipids in Chinese adults: a cross-sectional study. Eur J Clin Nutr 75, 708–714 (2021). https://doi.org/10.1038/s41430-020-00773-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00773-6