Abstract
Objective
To investigate the extent to which (1) secular changes in mid-adulthood WC are independent of BMI and (2) secular changes in low HDL-C are dependent on WC in each sex.
Methods
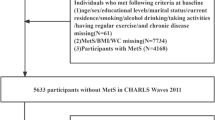
The sample comprised 19,406 adults (aged 43–47 years) from three birth cohort studies with BMI and WC measured in 1990, 2003, or 2018; 13,239 participants additionally had HDL-C measured in 2003 or 2018. Quantile regression was used to model differences between 1990–2003 and 2003–2018 in (1) BMI and WC internal Z-scores and (2) WC in cm before and after adjustment for BMI. Binary logistic regression was used to model differences between 2003 and 2018 in low HDL-C, before and after adjustment for BMI or WC.
Results
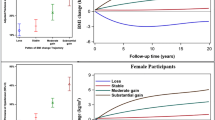
Secular increases in BMI and WC were larger between 1990 and 2003 than 2003 and 2018 and at the upper ends of the distributions. At the 85th quantile, effect sizes were larger for WC than BMI Z-scores in females but not males. Adjustment for BMI attenuated estimates of secular increases in WC in cm more in males than females. Odds ratios for low HDL-C in 2018 compared to 2003 were 1.73 (95% CI 1.32, 2.28) in males and 1.34 (1.01, 1.78) in females. Adjustment for WC did not substantially change the estimate in males but attenuated the estimate for females to 1.09 (0.81, 1.47).
Conclusions
In women much more so than in men, secular increases in mid-adulthood WC appear to have occurred independently of BMI and largely explain the observed rise in low HDL-C prevalence between 2003 and 2018.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Code availability
Available from the first author upon request.
References
NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387:1377–96.
NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes. 2008;32:959–66.
Prentice AM, Jebb SA. Beyond body mass index. Obes Rev. 2001;2:141–7.
Despres JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, et al. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008;28:1039–49.
Despres JP. Is visceral obesity the cause of the metabolic syndrome? Ann Med. 2006;38:52–63.
Camhi SM, Bray GA, Bouchard C, Greenway FL, Johnson WD, Newton RL. et al. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obesity. 2011;19:402–8.
Janssen I, Heymsfield SB, Allison DB, Kotler DP, Ross R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am J Clin Nutr. 2002;75:683–8.
Carmienke S, Freitag MH, Pischon T, Schlattmann P, Fankhaenel T, Goebel H, et al. General and abdominal obesity parameters and their combination in relation to mortality: a systematic review and meta-regression analysis. Eur J Clin Nutr. 2013;67:573–85.
de Hollander EL, Bemelmans WJ, Boshuizen HC, Friedrich N, Wallaschofski H, Guallar-Castillon P, et al. The association between waist circumference and risk of mortality considering body mass index in 65- to 74-year-olds: a meta-analysis of 29 cohorts involving more than 58 000 elderly persons. Int J Epidemiol. 2012;41:805–17.
Decoda Study G, Nyamdorj R, Qiao Q, Lam TH, Tuomilehto J, Ho SY. et al. BMI compared with central obesity indicators in relation to diabetes and hypertension in Asians. Obesity. 2018;16:1622–35.
Hamer M, O’Donovan G, Stensel D, Stamatakis E. Normal-weight central obesity and risk for mortality. Ann Intern Med. 2017;166:917–8.
Kodama S, Horikawa C, Fujihara K, Heianza Y, Hirasawa R, Yachi Y, et al. Comparisons of the strength of associations with future type 2 diabetes risk among anthropometric obesity indicators, including waist-to-height ratio: a meta-analysis. Am J Epidemiol. 2012;176:959–69.
Flegal KM, Shepherd JA, Looker AC, Graubard BI, Borrud LG, Ogden CL, et al. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am J Clin Nutr. 2009;89:500–8.
Albrecht SS, Gordon-Larsen P, Stern D, Popkin BM. Is waist circumference per body mass index rising differentially across the United States, England, China and Mexico? Eur J Clin Nutr. 2015;69:1306–12.
Elobeid MA, Desmond RA, Thomas O, Keith SW, Allison DB. Waist circumference values are increasing beyond those expected from BMI increases. Obesity. 2007;15:2380–3.
Ford ES, Mokdad AH, Giles WH. Trends in waist circumference among U.S. adults. Obes Res. 2003;11:1223–31.
Freedman DS, Ford ES. Are the recent secular increases in the waist circumference of adults independent of changes in BMI? Am J Clin Nutr. 2015;101:425–31.
Visscher TL, Heitmann BL, Rissanen A, Lahti-Koski M, Lissner L. A break in the obesity epidemic? Explained by biases or misinterpretation of the data? Int J Obes. 2015;39:189–98.
Walls HL, Stevenson CE, Mannan HR, Abdullah A, Reid CM, McNeil JJ, et al. Comparing trends in BMI and waist circumference. Obesity. 2011;19:216–9.
Rashid S, Genest J. Effect of obesity on high-density lipoprotein metabolism. Obesity. 2007;15:2875–88.
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med. 1977;62:707–14.
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. Diabetes, blood lipids, and the role of obesity in coronary heart disease risk for women. The Framingham study. Ann Intern Med. 1977;87:393–7.
Brenner DR, Tepylo K, Eny KM, Cahill LE, El-Sohemy A. Comparison of body mass index and waist circumference as predictors of cardiometabolic health in a population of young Canadian adults. Diabetol Metab Syndr. 2010;2:28.
Shen W, Punyanitya M, Chen J, Gallagher D, Albu J, Pi-Sunyer X, et al. Waist circumference correlates with metabolic syndrome indicators better than percentage fat. Obesity. 2006;14:727–36.
Schreiner PJ, Jacobs DR, Wong ND, Kiefe CI. Twenty-five year secular trends in lipids and modifiable risk factors in a population-based biracial cohort: the coronary artery risk development in young adults (CARDIA) Study, 1985–2011. J Am Heart Assoc. 2016;5:e003384.
Johnson W, Li L, Kuh D, Hardy R. How has the age-related process of overweight or obesity development changed over time? Co-ordinated analyses of individual participant data from five United Kingdom birth cohorts. PLoS Med. 2015;12:e1001828.
Kuh D, Pierce M, Adams J, Deanfield J, Ekelund U, Friberg P, et al. Cohort profile: updating the cohort profile for the MRC National Survey of Health and Development: a new clinic-based data collection for ageing research. Int J Epidemiol. 2011;40:e1–9.
Wadsworth M, Kuh D, Richards M, Hardy R. Cohort profile: The 1946 National Birth Cohort (MRC National Survey of Health and Development). Int J Epidemiol. 2006;35:49–54.
Power C, Elliott J. Cohort profile: 1958 British birth cohort (National Child Development Study). Int J Epidemiol. 2006;35:34–41.
Elliott J, Shepherd P. Cohort profile: 1970 British Birth Cohort (BCS70). Int J Epidemiol. 2006;35:836–43.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52.
Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97.
Bann D, Fitzsimons E, Johnson W. Determinants of the population health distribution: an illustration examining body mass index. Int J Epidemiol. 2020;49:731–7.
Royston P, Ambler G, Sauerbrei W. The use of fractional polynomials to model continuous risk variables in epidemiology. Int J Epidemiol. 1999;28:964–74.
Craig WY, Palomaki GE, Haddow JE. Cigarette smoking and serum lipid and lipoprotein concentrations: an analysis of published data. BMJ. 1989;298:784–8.
Freeman DJ, Griffin BA, Murray E, Lindsay GM, Gaffney D, Packard CJ, et al. Smoking and plasma lipoproteins in man: effects on low density lipoprotein cholesterol levels and high density lipoprotein subfraction distribution. Eur J Clin Investig. 1993;23:630–40.
Giskes K, Kunst AE, Benach J, Borrell C, Costa G, Dahl E, et al. Trends in smoking behaviour between 1985 and 2000 in nine European countries by education. J Epidemiol Community Health. 2005;59:395–401.
Ng M, Freeman MK, Fleming TD, Robinson M, Dwyer-Lindgren L, Thomson B, et al. Smoking prevalence and cigarette consumption in 187 countries, 1980-2012. JAMA. 2014;311:183–92.
Freedman DS, Zemel BS, Ogden CL. Secular trends for skinfolds differ from those for BMI and waist circumference among adults examined in NHANES from 1988-1994 through 2009-2010. Am J Clin Nutr. 2017;105:169–76.
Primatesta P, Poulter NR. Levels of dyslipidaemia and improvement in its management in England: results from the Health Survey for England 2003. Clin Endocrinol. 2006;64:292–8.
The Scottish Government. The Scottish Health Survey. Edinburgh: The Scottish Government; 2003.
Mindell J, Aresu M, Zaninotto P, Falaschetti E, Poulter N. Improving lipid profiles and increasing use of lipid-lowering therapy in England: results from a national cross-sectional survey—2006. Clin Endocrinol. 2011;75:621–7.
NCD Risk Factor Collaboration. Repositioning of the global epicentre of non-optimal cholesterol. Nature. 2020;582:73–7.
Kissebah AH, Vydelingum N, Murray R, Evans DJ, Hartz AJ, Kalkhoff RK, et al. Relation of body fat distribution to metabolic complications of obesity. J Clin Endocrinol Metab. 1982;54:254–60.
Kissebah AH, Alfarsi S, Adams PW. Integrated regulation of very low density lipoprotein triglyceride and apolipoprotein-B kinetics in man: normolipemic subjects, familial hypertriglyceridemia and familial combined hyperlipidemia. Metabolism. 1981;30:856–68.
Peiris AN, Sothmann MS, Hoffmann RG, Hennes MI, Wilson CR, Gustafson AB, et al. Adiposity, fat distribution, and cardiovascular risk. Ann Intern Med. 1989;110:867–72.
Munafo MR, Tilling K, Taylor AE, Evans DM, Davey Smith G. Collider scope: when selection bias can substantially influence observed associations. Int J Epidemiol. 2018;47:226–35.
Acknowledgements
This work was funded by the UK Medical Research Council (WJ New Investigator Research Grant: MR/P023347/1). WJ acknowledges support from the National Institute for Health Research (NIHR) Leicester Biomedical Research Centre, which is a partnership between University Hospitals of Leicester NHS Trust, Loughborough University, and the University of Leicester. The UK Medical Research Council provides core funding for the MRC National Survey of Health and Development. WJ conceptualised the study, carried out the analyses, and drafted the initial paper. All authors made substantial contributions to the interpretation of the data, revised the paper critically for important intellectual content, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
All of the studies have received ethical approval and obtained informed parental and/ or participant consent; this information is available from the study websites and/ or cohort profiles.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Johnson, W., Norris, T. & Hamer, M. Secular changes in mid-adulthood body mass index, waist circumference, and low HDL cholesterol between 1990, 2003, and 2018 in Great Britain. Eur J Clin Nutr 75, 539–545 (2021). https://doi.org/10.1038/s41430-020-00758-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00758-5
This article is cited by
-
Change in waist circumference and lifestyle habit factors as a predictor of metabolic risk among middle-aged and elderly Japanese people: population-based retrospective 10-year follow-up study from 2008 to 2017
Archives of Public Health (2022)
-
The impact of sex on blood pressure and anthropometry trajectories from early adulthood in a Nigerian population: insights into women’s cardiovascular disease risk across the lifespan
BMC Women's Health (2022)