Abstract
Objectives
Many developing countries currently face a double burden of malnutrition (DBM) at the household level, defined by the World Health Organization, as when a mother may be overweight or anemic, and a child or grandparent is underweight, in the same household. For the present study, we defined it as the coexistence of overweight or obesity in the mother, and at least one child under the age of 5 undernourished, within the same household. Although underweight has long been considered a major issue in South and Southeast Asia, overweight and obesity have also been identified as a growing problem. The main aim of this study was to assess the DBM at the household level and its major determinants in South and Southeast Asia.
Methods
We used population-representative cross-sectional data from the Demographic and Health Survey, conducted between 2007 and 2017, for eight South and Southeast Asian countries: Bangladesh, India, Nepal, Pakistan, Myanmar, Timor, Maldives, and Cambodia. Multivariate logistic regression was performed to identify the sociodemographic factors associated with DBM.
Results
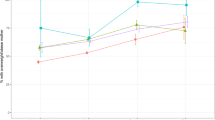
A total of 798,961 households were included in this study. The pooled prevalence of overweight or obesity for the mother and stunted child was 10.0% (95% CI: 8.0.0–12.0), for OBM and wasted child, it was 7.0% (95% confidence interval (CI): 6.0–8.0), and for overweight or obese mother (OBM) and underweight child, it was 7.0% (95% CI: 6.0–8.0). The prevalence of any of these DBM coexistences was 12.0% (95% CI: 10.0–13.0) in all households. Statistically significant positive associations (p < 0.05) were found for each of these coexistences, and a higher age of the mother, mothers with a lower education, the richest household quintile, and households with more than four members.
Conclusion
It is imperative that “double duty” action policies are developed that tackle the DBM, rather than targeting undernutrition or overnutrition separately. The findings from this study suggest that the promotion of education for women may aid in tackling the double burden on a household level.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Hoque ME, Hasan MT, Rahman M, Long KZ, Al Mamun A. Double burden of underweight and overweight among Bangladeshi adults differs between men and women: evidence from a nationally representative survey. JPHN. 2017;20:2183–91.
Doak CM, Adair LS, Monteiro C, Popkin BM. Overweight and underweight coexist within households in Brazil, China and Russia. J Nutr. 2000;130:2965–71.
Hanandita W, Tampubolon G. The double burden of malnutrition in Indonesia: social determinants and geographical variations. SSM-Popul Health. 2015;1:16–25.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. The Lancet. 2013;382:427–51.
Bloom D, Cafiero E, Jané-Llopis E, Abrahams-Gessel S, Bloom L, Fathima S, et al. The global economic burden of noncommunicable diseases. Geneva: Program on the Global Demography of Aging; 2012.
Robert KW, Parris TM, Leiserowitz AA. What is sustainable development? Goals, Indicators, Values, and Practice. 2005;47:8–21.
Dieffenbach SD. Are stunted child/overweight mother pairs a distinct entity or a statistical artifact? Demographic and Health Surveys, 1991–2009. Stein: Emory University; 2012.
NIPORT M, Macro O. Bangladesh demographic and health survey 2004. Dhaka: National Institute of Population Research and Training, Mitra and Associates, and ORC Macro; 2005.
NIPORT M. Bangladesh demographic and health survey BDHS 2014: key indicators. Dhaka and Calverton, Maryland: National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ICF International; 2014.
Biswas T, Uddin MJ, Al Mamun A, Pervin S, Garnett SP. Increasing prevalence of overweight and obesity in Bangladeshi women of reproductive age: findings from 2004 to 2014. PloS ONE. 2017;12:e0181080.
Swinburn BA, Kraak VI, Allender S, Atkins VJ, Baker PI, Bogard JR, et al. The global syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. Lancet. 2019;393:791–846.
Perez-Escamilla R, Bermudez O, Buccini GS, Kumanyika S, Lutter CK, Monsivais P, et al. Nutrition disparities and the global burden of malnutrition. BMJ. 2018;361:k2252.
Das S, Shah MF, Islam MS, Biswas T, Mahfuz M, Ahmed T. Prevalence and sociodemographic determinants of household-level double burden of malnutrition in Bangladesh. JPHN. 2019;22:1425–32.
Jehn M, Brewis AJE, Biology H. Paradoxical malnutrition in mother–child pairs: untangling the phenomenon of over- and under-nutrition in underdeveloped economies. Econ Hum Biol. 2009;7:28–35.
Oddo VM, Rah JH, Semba RD, Sun K, Akhter N, Sari M, et al. Predictors of maternal and child double burden of malnutrition in rural Indonesia and Bangladesh. The Am J Clin Nutr. 2012;95:951–8.
Schott W, Aurino E, Penny ME, Behrman JR. The double burden of malnutrition among youth: trajectories and inequalities in four emerging economies. Econ Hum Biol. 2019;34:80–91.
Kimani-Murage EW, Muthuri SK, Oti SO, Mutua MK, van de Vijver S, Kyobutungi C. Evidence of a double burden of malnutrition in urban poor settings in Nairobi, Kenya. PloS ONE. 2015;10:e0129943.
Kosaka S, Umezaki M. A systematic review of the prevalence and predictors of the double burden of malnutrition within households. Br J Nutr. 2017;117:1118–27.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157.
Pi-Sunyer X. Clinical guidelines on the identification, evaluation and treatment of overweight and obesity in adults-the evidence report. Obes Res. 1998;6:51S–210S.
Biswas T, Islam MS, Linton N, Rawal LB. Socio-economic inequality of chronic non-communicable diseases in Bangladesh. PloS ONE. 2016;11:e0167140.
Hasan MT, Soares Magalhaes RJ, Williams GM, Mamun AAJM. The role of maternal education in the 15‐year trajectory of malnutrition in children under 5 years of age in Bangladesh. 2016;12:929–39.
Jehn M, Brewis A. Paradoxical malnutrition in mother–child pairs: untangling the phenomenon of over-and under-nutrition in underdeveloped economies. Econ Hum Biol. 2009;7:28–35.
Sekiyama M, Jiang HW, Gunawan B, Dewanti L, Honda R, Shimizu-Furusawa H, et al. Double burden of malnutrition in rural West Java: household-level analysis for father-child and mother-child pairs and the association with dietary intake. Nutrients. 2015;7:8376–91.
Wong C, Zalilah M, Chua E, Norhasmah S, Chin Y, Nur’Asyura AS. Double-burden of malnutrition among the indigenous peoples (Orang Asli) of Peninsular Malaysia. BMC Public Health. 2015;15:680.
Biswas T, Townsend N, Magalhaes RS, Islam MS, Hasan MM, Mamun A. Current progress and future directions in the double burden of malnutrition among women in South and Southeast Asian countries. Curr Dev Nutr. 2019;3:nzz026.
World Health Organization. Double-duty actions for nutrition: policy brief. Geneva: World Health Organization; 2017.
Acknowledgements
We thank the MEASURE DHS Data Archive, ICF International, for providing access to the South and Southeast Asian Demographic and Health Surveys data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Biswas, T., Townsend, N., Magalhaes, R.J.S. et al. Patterns and determinants of the double burden of malnutrition at the household level in South and Southeast Asia. Eur J Clin Nutr 75, 385–391 (2021). https://doi.org/10.1038/s41430-020-00726-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00726-z
This article is cited by
-
Genetic biofortification: advancing crop nutrition to tackle hidden hunger
Functional & Integrative Genomics (2024)
-
How does mode of delivery associate with double burden of malnutrition among mother–child dyads?: a trend analysis using Bangladesh demographic health surveys
BMC Public Health (2022)
-
Dietary diversity and micronutrient adequacy among women of reproductive age: a cross-sectional study in Southern Thailand
BMC Nutrition (2022)