Abstract
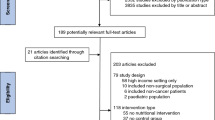
Postoperative malnutrition is a major issue among gastrointestinal cancer patients. Because n-3 polyunsaturated fatty acids (n-3 PUFAs) have immunological benefits, n-3 PUFAs are widely used in oral nutritional supplements (ONS). However, n-3 PUFAs in ONS reduced patients’ compliance with ONS and affected the role of ONS in maintaining the postoperative nutritional status of patients. The aim of this study was to systematically explore the benefits of enteral nutrition rich in n-3 PUFAs in maintaining the nutritional status of patients after gastrointestinal surgery. Databases including PubMed, Web of Science, Embase, Cochrane Library, China National Knowledge Infrastructure, Wanfang, and VIP databases were searched through March 16, 2019. The references of related reviews and studies were assessed up to March 16, 2019. The effect sizes from individual studies were calculated as the standardized mean difference (SMD), mean difference (MD), and risk ratio (RR) with 95% confidence intervals (95% CIs). A total of 11 studies (n = 977) were included. In this systematic review and meta-analysis, we observed that enteral supplementation of n-3 PUFAs had no significant effect on weight (MD, 1.09; 95% CI, −0.90, 3.08), body mass index (MD, 0.55; 95% CI, −1.45, 2.54), albumin (SMD, 0.39; 95% CI, −0.10, 0.87), wound infections (RR, 0.87, 95% CI, 0.57, 1.33), or pneumonia (RR, 0.98; 95% CI, 0.60, 1.59) in gastrointestinal cancer patients. Thus, compared with enteral nutritional without n-3 PUFAs, enteral nutritional rich in n-3 PUFAs has no significant effects on nutritional status, incidence of pneumonia, or wound infections among gastrointestinal cancer patients during postoperative convalescence.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003;22:235–9.
Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, et al. Diagnostic criteria for malnutrition - an ESPEN Consensus Statement. Clin Nutr. 2015;34:335–40.
Mosquera C, Koutlas NJ, Edwards KC, Strickland A, Vohra NA, Zervos EE, et al. Impact of malnutrition on gastrointestinal surgical patients. J Surg Res. 2016;205:95–101.
Young LS, Huong PT, Lam NT, Thu NN, Van HT, Hanh NL, et al. Nutritional status and feeding practices in gastrointestinal surgery patients at Bach Mai Hospital, Hanoi,Vietnam. Asia Pac J Clin Nutr. 2016;25:513–20.
Chunlai C, Hui L. Patients with gastrointestinal cancer chemotherapy nutritional status assessment and its impact on immune function. J Mod Oncol. 2015;23:1412–6.
Bozzetti F, Gianotti L, Braga M, Di Carlo V, Mariani L. Postoperative complications in gastrointestinal cancer patients: the joint role of the nutritional status and the nutritional support. Clin Nutr. 2007;26:698–709.
Aguirre A, Fischer JE, Welch CE. The role of surgery and hyperalimentation in therapy of gastrointestinal-cutaneous fistulae. Ann Surg. 1974;180:393–401.
Goiburu ME, Goiburu MM, Bianco H, Diaz JR, Alderete F, Palacios MC, et al. The impact of malnutrition on morbidity, mortality and length of hospital stay in trauma patients. Nutricion Hospitalaria. 2006;21:604–10.
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36:11–48.
Hatao F, Chen KY, Wu JM, Wang MY, Aikou S, Onoyama H, et al. Randomized controlled clinical trial assessing the effects of oral nutritional supplements in postoperative gastric cancer patients. Langenbeck’s Arch Surg. 2017;402:203–11.
Beattie AH, Prach AT, Baxter JP, Pennington CR. A randomised controlled trial evaluating the use of enteral nutritional supplements postoperatively in malnourished surgical patients. Gut. 2000;46:813–8.
Grass F, Bertrand PC, Schafer M, Ballabeni P, Cerantola Y, Demartines N, et al. Compliance with preoperative oral nutritional supplements in patients at nutritional risk-only a question of will? Eur J Clin Nutr. 2015;69:525–9.
Bolton J, Abbott R, Kiely M. Comparison of three oral sip-feed supplements in patients with cancer. J Hum Nutr Dietetics. 2010;5:79–84.
Tian M, Suco E, Gosses A. MON-PP089: a double-blind study comparing taste, preference and compliance of 3 oral nutrition supplements frequently consumed by oncology Patient. Clin Nut. 2015;34:S160–1.
Fearon KC, Barber MD, Moses AG, Ahmedzai SH, Taylor GS, Tisdale MJ, et al.Double-blind placebo-controlled, randomized study of eicosapentaenoic acid diester in patients with cancer cachexia. J Clin Oncol. 2006;24:3401–7.
Read JA, Beale PJ, Volker DH, Smith N, Childs A, Clarke SJ. Nutrition intervention using an eicosapentaenoic acid (EPA)-containing supplement in patients with advanced colorectal cancer. Effects on nutritional and inflammatory status: a phase II trial. Supportive Care Cancer. 2007;15:301–7.
Fearon KC, Von Meyenfeldt MF, Moses AG, Van Geenen R, Roy A, Gouma DJ, et al. Effect of a protein and energy dense N-3 fatty acid enriched oral supplement on loss of weight and lean tissue in cancer cachexia: a randomised double blind trial. Gut. 2003;52:1479–86.
Bruera E, Strasser F, Palmer JL, Willey J, Calder K, Amyotte G, et al. Effect of fish oil on appetite and other symptoms in patients with advanced cancer and anorexia/cachexia: a double-blind, placebo-controlled study. J Clin Oncol. 2003;21:129–34.
Fetterman JW Jr., Zdanowicz MM. Therapeutic potential of n-3 polyunsaturated fatty acids in disease. Am J Health-Syst Pharm. 2009;66:1169–79.
Lane KE, Derbyshire EJ. Omega-3 fatty acids - a review of existing and innovative delivery methods. Crit Rev food Sci Nutr. 2018;58:62–9.
Hamilton E, Ravikumar R, Bartlett D, Hepburn E, Hwang MJ, Mirza N, et al. Dexamethasone reduces emesis after major gastrointestinal surgery (DREAMS). Trials. 2013;14:249.
Kris-Etherton PM, Harris WS, Appel LJ. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation. 2002;106:2747–57.
Sacks FM, Stone PH, Gibson CM, Silverman DI, Rosner B, Pasternak RC. Controlled trial of fish oil for regression of human coronary atherosclerosis. HARP Research Group. J Am Coll Cardiol. 1995;25:1492–8.
Wallace JM, McCabe AJ, Robson PJ, Keogh MK, Murray CA, Kelly PM, et al. Bioavailability of n-3 polyunsaturated fatty acids (PUFA) in foods enriched with microencapsulated fish oil. Ann Nutr Metab. 2000;44:157–62.
Sultan J, Griffin SM, Di Franco F, Kirby JA, Shenton BK, Seal CJ, et al. Randomized clinical trial of omega-3 fatty acid-supplemented enteral nutrition versus standard enteral nutrition in patients undergoing oesophagogastric cancer surgery. Br J Surg. 2012;99:346–55.
Ryan AM, Reynolds JV, Healy L, Byrne M, Moore J, Brannelly N, et al. Enteral nutrition enriched with eicosapentaenoic acid (EPA) preserves lean body mass following esophageal cancer surgery: results of a double-blinded randomized controlled trial. Ann Surg. 2009;249:355–63.
Shuster JJ. Review: Cochrane handbook for systematic reviews for interventions, version 5.1.0, published 3/2011. Julian P.T. Higgins and Sally Green, Editors. Res Synth Methods. 2011;2:126–30.
Matsuda Y, Habu D, Lee S, Kishida S, Osugi H. Enteral diet enriched with omega-3 fatty acid improves oxygenation after thoracic esophagectomy for cancer: a randomized controlled trial. World J Surg. 2017;41:1584–94.
Healy LA, Ryan A, Doyle SL, Ni Bhuachalla EB, Cushen S, Segurado R, et al. Does prolonged enteral feeding with supplemental omega-3 fatty acids impact on recovery post-esophagectomy: results of a randomized double-blind trial. Ann Surg. 2017;266:720–8.
Ida S, Hiki N, Cho H, Sakamaki K, Ito S, Fujitani K, et al. Randomized clinical trial comparing standard diet with perioperative oral immunonutrition in total gastrectomy for gastric cancer. Br J Surg. 2017;104:377–83.
Silva Jde A, Trindade EB, Fabre ME, Menegotto VM, Gevaerd S, Buss Zda S, et al. Fish oil supplement alters markers of inflammatory and nutritional status in colorectal cancer patients. Nutr Cancer. 2012;64:267–73.
Mocellin MC, Pastore e Silva Jde A, Camargo Cde Q, Fabre ME, Gevaerd S, Naliwaiko K, et al. Fish oil decreases C-reactive protein/albumin ratio improving nutritional prognosis and plasma fatty acid profile in colorectal cancer patients. Lipids. 2013;48:879–88.
Sorensen LS, Thorlacius-Ussing O, Schmidt EB, Rasmussen HH, Lundbye-Christensen S, Calder PC, et al. Randomized clinical trial of perioperative omega-3 fatty acid supplements in elective colorectal cancer surgery. Br J Surg. 2014;101:33–42.
Zhuang ST, Li QZ, Cai YJ, Wu SH, Chen B, Zheng K. Effects of early postoperative enteral immune nutrition on immune function and inflammatory response in patients with colorectal cancer. Chin J Clin. 2013;7:117–9.
WU YX, Xia L, Wang Y. Clinical effect of preoperative administration of enteral nutrition enriched ω-3 fatty acids for gastric cancer. Chin J Bases Clin General Surg. 2015;22:312–6.
Emori TG, Gaynes RP. An overview of nosocomial infections, including the role of the microbiology laboratory. Clin Microbiol Rev. 1993;6:428–42.
Ephgrave KS, Kleiman-Wexler R, Pfaller M, Booth B, Werkmeister L, Young S. Postoperative pneumonia: a prospective study of risk factors and morbidity. Surgery. 1993;114:815–9. discussion 9-21
Sagawa M, Yokomizo H, Yoshimatsu K, Yano Y, Okayama S, Sakuma A, et al. Relationship between surgical site infection(ssi)incidence and prognosis in colorectal cancer surgery. Gan Kagaku Ryoho Cancer Chemother. 2017;44:921–3.
Kiuchi J, Komatsu S, Ichikawa D, Kosuga T, Okamoto K, Konishi H, et al. Putative risk factors for postoperative pneumonia which affects poor prognosis in patients with gastric cancer. Int J Clin Oncol. 2016;21:920–6.
Guo ZQ, Yu JM, Li W, Fu ZM, Lin Y, Shi YY, et al. Survey and analysis of the nutritional status in hospitalized patients with malignant gastric tumors and its influence on the quality of life. Support Care Cancer. 2019; https://doi.org/10.1007/s00520-019-04803-3 (E-pub ahead of print 3 May 2019).
Onishi S, Shiraki M, Nishimura K, Hanai T, Moriwaki H, Shimizu M. Prevalence of sarcopenia and its relationship with nutritional state and quality of life in patients with digestive diseases. J Nutr Sci Vitaminol. 2018;64:445–53.
Sakurai K, Ohira M, Tamura T, Toyokawa T, Amano R, Kubo N, et al. Predictive potential of preoperative nutritional status in long-term outcome projections for patients with gastric cancer. Ann Surg Oncol. 2016;23:525–33.
Aoyama T, Sato T, Maezawa Y, Kano K, Hayashi T, Yamada T, et al. Postoperative weight loss leads to poor survival through poor S-1 efficacy in patients with stage II/III gastric cancer. Int J Clin Oncol. 2017;22:476–83.
He Y, Wang J, Bian H, Deng X, Wang Z. BMI as a predictor for perioperative outcome of laparoscopic colorectal surgery: a pooled analysis of comparative studies. Dis Colon Rectum. 2017;60:433–45.
Aoyama T, Kawabe T, Fujikawa H, Hayashi T, Yamada T, Tsuchida K, et al. Loss of lean body mass as an independent risk factor for continuation of S-1 adjuvant chemotherapy for gastric cancer. Ann Surg Oncol. 2015;22:2560–6.
Aoyama T, Sato T, Segami K, Maezawa Y, Kano K, Kawabe T, et al. Risk factors for the loss of lean body mass after gastrectomy for gastric cancer. Ann Surg Oncol. 2016;23:1963–70.
Ma YJ, Liu L, Xiao J, Cao BW. Perioperative omega-3 polyunsaturated fatty acid nutritional support in gastrointestinal cancer surgical patients: a systematic evaluation. Nutr Cancer. 2016;68:568–76.
Matsunaga T, Miyata H, Sugimura K, Motoori M, Asukai K, Yanagimoto Y, et al. Prognostic significance of sarcopenia and systemic inflammatory response in patients with esophageal cancer. Anticancer Res. 2019;39:449–58.
Fritsche K. Fatty acids as modulators of the immune response. Annu Rev Nutr. 2006;26:45–73.
Yu J, Liu L, Zhang Y, Wei J, Yang F. Effects of omega-3 fatty acids on patients undergoing surgery for gastrointestinal malignancy: a systematic review and meta-analysis. BMC Cancer. 2017;17:271.
Tan A, Sullenbarger B, Prakash R, McDaniel JC. Supplementation with eicosapentaenoic acid and docosahexaenoic acid reduces high levels of circulating proinflammatory cytokines in aging adults: a randomized, controlled study. Prostaglandins, Leukotrienes, Essent Fat Acids. 2018;132:23–9.
Berger MM, Delodder F, Liaudet L, Tozzi P, Schlaepfer J, Chiolero RL, et al. Three short perioperative infusions of n-3 PUFAs reduce systemic inflammation induced by cardiopulmonary bypass surgery: a randomized controlled trial. Am J Clin Nutr. 2013;97:246–54.
van Norren K, Kegler D, Argiles JM, Luiking Y, Gorselink M, Laviano A, et al. Dietary supplementation with a specific combination of high protein, leucine, and fish oil improves muscle function and daily activity in tumour-bearing cachectic mice. Br J cancer. 2009;100:713–22.
Hayashi N, Tashiro T, Yamamori H, Takagi K, Morishima Y, Otsubo Y, et al. Effect of intravenous omega-6 and omega-3 fat emulsions on nitrogen retention and protein kinetics in burned rats. Nutrition. 1999;15:135–9.
Aoyama T, Yoshikawa T, Ida S, Cho H, Sakamaki K, Ito Y, et al. Effects of perioperative eicosapentaenoic acid-enriched oral nutritional supplement on lean body mass after total gastrectomy for gastric cancer. J Cancer. 2019;10:1070–6.
Noguchi Y, Tsuburaya A, Makino T, et al. Metabolic alteration in totally gastrectomised patients—caloric intake and energy con-sumption. Asian J Surg. 1992;15:97–102.
Giger-Pabst U, Lange J, Maurer C, Bucher C, Schreiber V, Schlumpf R, et al. Short-term preoperative supplementation of an immunoenriched diet does not improve clinical outcome in well-nourished patients undergoing abdominal cancer surgery. Nutrition. 2013;29:724–9.
Acknowledgements
This work was supported by grants from the National natural science foundation of China [31800895] to X-yZ and Youth Science and Technology Backbone Project [2017Q026] of Health Science and Technology of Jilin Province to X-yZ.
Funding
This work was supported by the National natural science foundation of China [31800895], and Youth Science and Technology Backbone Project [2017Q026] of Health Science and Technology of Jilin Province.
Author information
Authors and Affiliations
Contributions
G-yW contributed to the performance of the study, analysis and interpretation the data, and drafted the manuscript; L-yZ contributed to the supervision of the study and interpreted the data; HY contributed to the analysis and interpretation the data; H-qL contributed to the performance of the study and revised the manuscript; and X-yZ and HX contributed to the conception of the study, performed the study, interpreted the data, and significantly revised the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wan, Gy., Zheng, Ly., Li, Hq. et al. Effects of enteral nutritional rich in n-3 polyunsaturated fatty acids on the nutritional status of gastrointestinal cancer patients: a systematic review and meta-analysis. Eur J Clin Nutr 74, 220–230 (2020). https://doi.org/10.1038/s41430-019-0527-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-019-0527-5