Abstract
Background/objectives
There is scarce evidence of how certain eating behaviours compromise the compliance with dietary guidelines and weight status in school-aged children. This study aims to evaluate the association of children’s problematic eating behaviours with food quality and body mass index at 7 years of age.
Subjects/methods
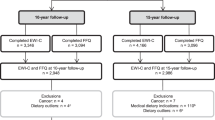
Participants were children aged 7 years old from a population-based cohort study from Porto, Portugal-Generation XXI. Children’s quantity and speed of ingestion, food refusal at the table and food rewards requesting were evaluated by caregiver’s perception. Food consumption was evaluated by a food frequency questionnaire and compared with age-appropriate guidelines. Children’s weight status was assessed by objective measurements and parent’s perceptions. Associations were estimated by logistic regressions (odds ratio (OR), 95% confidence intervals (95% CI)) adjusted for maternal age, education, smoking during pregnancy, birth type, child’s sex, weight-for-gestational age and sports (n = 3801).
Results
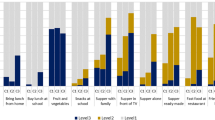
Children eating small amounts of food, refusing to eat at the table with the rest of the family during meals and asking for food rewards showed a higher consumption of energy-dense foods (OR = 1.51; 95% CI:1.23–1.86; OR = 1.58; 95% CI:1.16–2.16; OR = 1.56; 95% CI:1.14–2.12) and presented higher odds of consuming fruit and vegetables below recommendations (OR = 1.41; 95% CI:1.22–1.64; OR = 1.20; 95% CI:1.00–1.45; OR = 1.28; 95% CI:1.05–1.55). Children displaying these eating behaviours were less likely to be overweight/obese, hence their parents were less likely to show concern with their weight. Including food quality as covariate in the final models with obesity status did not change the associations.
Conclusions
Problematic eating behaviours were associated with poorer food quality (more energy-dense foods and low fruit and vegetables), but food quality does not seem to explain the association with obesity status. Parents were less likely to be concerned about their child’s weight if the child ate slowly or poorly, and accordingly the odds of them being overweight or obese were lower.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Oliveira A, Jones L, de Lauzon-Guillain B, Emmett P, Moreira P, Charles MA, et al. Early problematic eating behaviours are associated with lower fruit and vegetable intake and less dietary variety at 4-5 years of age. A prospective analysis of three European birth cohorts. Br J Nutr. 2015;114:763–71.
Aldridge VK, Dovey TM, Martin CI, Meyer C. Identifying clinically relevant feeding problems and disorders. J Child Health Care. 2010;14:261–70.
Dovey TMSP, Gibson EL, Halford JC. Food neophobia and ‘picky/fussy’ eating in children: a review. Appetite. 2008;50:181–93.
van Dijk M, Bruinsma E, Hauser MP. The relation between child feeding problems as measured by parental report and mealtime behavior observation: a pilot study. Appetite. 2016;99:262–67.
Jacobi C, Agras WS, Bryson S, Hammer LD. Behavioral validation, precursors, and concomitants of picky eating in childhood. J Am Acad Child Adolesc Psychiatry. 2003;42:76–84.
Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101:539–49.
Mascola AJ, Bryson SW, Agras WS. Picky eating during childhood: a longitudinal study to age 11 years. Eat Behav. 2010;11:253–7.
Dubois L, Farmer AP, Girard M, Peterson K. Preschool children’s eating behaviours are related to dietary adequacy and body weight. Eur J Clin Nutr. 2007;61:846–55.
Dovey TM, Staples PA, Gibson EL, Halford JCG. Food neophobia and ‘picky/fussy’ eating in children: a review. Appetite. 2008;50:181–93.
Galloway AT, Fiorito L, Lee Y, Birch LL. Parental pressure, dietary patterns, and weight status among girls who are “picky eaters”. J Am Diet Assoc. 2005;105:541–8.
Galloway AT, Lee Y, Birch LL. Predictors and consequences of food neophobia and pickiness in young girls. J Am Diet Assoc. 2003;103:692–8.
Carruth BR, Ziegler PJ, Gordon A, Barr SI. Prevalence of picky eaters among infants and toddlers and their caregivers’ decisions about offering a new food. J Am Diet Assoc. 2004;104:s57–64.
de Lauzon-Guillain B, Jones L, Oliveira A, Moschonis G, Betoko A, Lopes C, et al. The influence of early feeding practices on fruit and vegetable intake among preschool children in 4 European birth cohorts. Am J Clin Nutr. 2013;98:804–12.
de Barse LM, Tiemeier H, Leermakers ET, Voortman T, Jaddoe VW, Edelson LR, et al. Longitudinal association between preschool fussy eating and body composition at 6 years of age: the Generation R Study. Int J Behav Nutr Phys Act. 2015;12:153.
Fildes A, Mallan KM, Cooke L, van Jaarsveld CH, Llewellyn CH, Fisher A, et al. The relationship between appetite and food preferences in British and Australian children. Int J Behav Nutr Phys Act. 2015;12:116.
Taylor CM, Northstone K, Wernimont SM, Emmett PM. Macro- and micronutrient intakes in picky eaters: a cause for concern? Am J Clin Nutr. 2016;104:1647–56.
van der Horst K, Deming DM, Lesniauskas R, Carr BT, Reidy KC. Picky eating: associations with child eating characteristics and food intake. Appetite. 2016;103:286–93.
Cooke LJ, Wardle J. Age and gender differences in children’s food preferences. Br J Nutr. 2005;93:741–6.
Russell CG, Worsley A. Do children’s food preferences align with dietary recommendations? Public Health Nutr. 2007;10:1223–33.
Webber L, Hill C, Saxton J, Van Jaarsveld CH, Wardle J. Eating behaviour and weight in children. Int J Obes (Lond). 2009;33:21–8.
Viana V, Sinde S, Saxton JC. Children’s Eating Behaviour Questionnaire: associations with BMI in Portuguese children. Br J Nutr. 2008;100:445–50.
Vallejo M, Cortes-Rodriguez BA, Colin-Ramirez E. Maternal underestimation of child’s weight status and health behaviors as risk factors for overweight in children. J Pediatr Nurs. 2015;30:e29–33.
Rodgers RF, Paxton SJ, Massey R, Campbell KJ, Wertheim EH, Skouteris H, et al. Maternal feeding practices predict weight gain and obesogenic eating behaviors in young children: a prospective study. Int J Behav Nutr Phys Act. 2013;10:24.
Gregory JE, Paxton SJ, Brozovic AM. Maternal feeding practices, child eating behaviour and body mass index in preschool-aged children: a prospective analysis. Int J Behav Nutr Phys Act. 2010;7:55.
Cooke L. The importance of exposure for healthy eating in childhood: a review. J Hum Nutr Diet. 2007;20:294–301.
Shloim N, Edelson LR, Martin N, Hetherington MM. Parenting styles, feeding styles, feeding practices, and weight status in 4-12 year-old children: a systematic review of the literature. Front Psychol. 2015;6:1849
Larsen PS, Kamper-Jorgensen M, Adamson A, Barros H, Bonde JP, Brescianini S, et al. Pregnancy and birth cohort resources in Europe: a large opportunity for aetiological child health research. Paediatr Perinat Epidemiol. 2013;27:393–414.
Husted JA, Cook RJ, Farewell VT, Gladman DD. Methods for assessing responsiveness: a critical review and recommendations. J Clin Epidemiol. 2000;53:459–68.
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics. 2001;108:E35.
Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the Children’s Eating Behaviour Questionnaire. J Child Psychol Psychiatry. 2001;42:963–70.
Carnell S, Wardle J. Measuring behavioural susceptibility to obesity: validation of the child eating behaviour questionnaire. Appetite. 2007;48:104–13.
Svensson V, Lundborg L, Cao Y, Nowicka P, Marcus C, Sobko T. Obesity related eating behaviour patterns in Swedish preschool children and association with age, gender, relative weight and parental weight--factorial validation of the Children’s Eating Behaviour Questionnaire. Int J Behav Nutr Phys Act. 2011;8:134.
Ashcroft J, Semmler C, Carnell S, van Jaarsveld CH, Wardle J. Continuity and stability of eating behaviour traits in children. Eur J Clin Nutr. 2008;62:985–90.
Albuquerque G, Severo M, Oliveira A. Early life characteristics associated with appetite-related eating behaviors in 7-year-old children. J Pediatr. 2017;180:e2.
Durão C, Andreozzi V, Oliveira A, Moreira P, Guerra A, Barros H, et al. Maternal child-feeding practices and dietary inadequacy of 4-year-old children. Appetite. 2015;92:15–23.
Stewart A, Marfell-Jones M, Olds T, de Ridder H. International Standards for Anthropometric Assessment. New Zeland: The International Society for the Advancement of Kinanthropometry; 2011.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
Real H, Oliveira A, Severo M, Moreira P, Lopes C. Combination and adaptation of two tools to assess parental feeding practices in pre-school children. Eat Behav. 2014;15:383–7.
Swinburn B, Sacks G, Ravussin E. Increased food energy supply is more than sufficient to explain the US epidemic of obesity. Am J Clin Nutr. 2009;90:1453–6.
Powell F, Farrow C, Meyer C, Haycraft E. The importance of mealtime structure for reducing child food fussiness. Matern Child Nutr. 2017;13..
Jacobi C, Schmitz G, Agras WS. Is picky eating an eating disorder? Int J Eat Disord. 2008;41:626–34.
Sleddens E, Kremers S, Thijs C. The Children’s Eating Behaviour Questionnaire: factorial validity and association with Body Mass Index in Dutch children aged 6–7. Int J Behav Nutr Phys Act. 2008;5:49.
Rietmeijer-Mentink M, Paulis WD, van Middelkoop M, Bindels PJ, van der Wouden JC. Difference between parental perception and actual weight status of children: a systematic review. Matern Child Nutr. 2013;9:3–22.
Brown CL, Pesch MH, Perrin EM, Appugliese DP, Miller AL, Rosenblum K, et al. Maternal concern for child undereating. Acad Pediatr. 2016;16:777–82.
Guevara-Cruz M, Serralde-Zuniga AE, Frigolet Vazquez-Vela ME, Blancas Galicia L, Islas-Ortega L. Association between maternal perceptions and actual nutritional status for children in a study group in Mexico. Nutr Hosp. 2012;27:209–12.
Moore LC, Harris CV, Bradlyn AS. Exploring the relationship between parental concern and the management of childhood obesity. Matern Child Health J. 2012;16:902–8.
Warschburger P, Kroller K. “Childhood overweight and obesity: maternal perceptions of the time for engaging in child weight management”. BMC Public Health. 2012;12:295.
Gerards SM, Gubbels JS, Dagnelie PC, Kremers SP, Stafleu A, de Vries NK, et al. Parental perception of child’s weight status and subsequent BMI z change: the KOALA birth cohort study. BMC Public Health. 2014;14:291.
Bjelland M, Brantsaeter AL, Haugen M, Meltzer HM, Nystad W, Andersen LF. Changes and tracking of fruit, vegetables and sugar-sweetened beverages intake from 18 months to 7 years in the Norwegian Mother and Child Cohort Study. BMC Public Health. 2013;13:793.
Northstone K, Emmett PM. Are dietary patterns stable throughout early and mid-childhood? A birth cohort study. Br J Nutr. 2008;100:1069–76.
Biro FM, Wien M. Childhood obesity and adult morbidities. Am J Nutr. 2010;91:1499s–505s.
Cornette R. The emotional impact of obesity on children. World Evid Based Nurs. 2008;5:136–41.
Acknowledgements
We are indebted to all participants for providing the data used in the Generation XXI birth cohort, as well as to all members of the research team and its coordinators (Henrique Barros and Ana Cristina Santos). The authors acknowledge the support from the Epidemiology Research Unit (EPIUnit: UID-DTP/04750/2013).
Funding
Generation XXI was funded by the Health Operational Programme—Saúde XXI, Community Support Framework III and the Regional Department of Ministry of Health. This study was supported through FEDER from the Operational Programme Factors of Competitiveness (COMPETE) and through national funding from the Foundation for Science and Technology (FCT; Portuguese Ministry of Education and Science) under the project PTDC/SAU-EPI/121532/2010 (FCOMP-01-0124-FEDER-021177) and through the Investigator Programme (IF/01350/2015–Andreia Oliveira and IF/01060/2015–Ana Cristina Santos). It also had support from the Calouste Gulbenkian Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Costa, S., Pinto, A., Santos, A.C. et al. The association of problematic eating behaviours with food quality and body mass index at 7 years of age. Eur J Clin Nutr 73, 549–557 (2019). https://doi.org/10.1038/s41430-018-0169-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-018-0169-z