Abstract
Background/Objectives
With technological advances, there has been a resurgence in ultrasound as a method to measure subcutaneous fat thickness. Despite the increased interest in this methodology, research comparing A-mode and B-mode ultrasound devices is lacking. Subcutaneous fat thickness measured by a low resolution (2.5 MHz) A-mode ultrasound and a high resolution (12 MHz) B-mode ultrasound were compared to the actual fat thickness in dissected cadavers.
Subjects/Methods
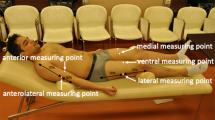
Subcutaneous fat thickness of six cadavers was measured at the abdomen, thigh, triceps, and calf (plus chest for males and suprailiac for females) with both ultrasound devices before the cadavers were dissected and site-specific thickness was measured.
Results
Correlations between both ultrasounds and the dissected measurement exceeded 0.90 at all sites with a few exceptions. At the abdomen, the relationship between the ultrasounds was 0.76, and the B-mode and dissected measurement was also 0.76. The correlation between dissection and A-mode was 0.75 for the suprailiac site, but it was not possible to discern the separation of tissue at this site when using the B-mode device. There were no significant differences (P > 0.05) between the devices and the dissected measurement at any of the six sites. The mean difference in fat thickness between A-mode and B-mode was <0.7 mm at all sites except the calf (1.2 mm)
Conclusion
With the exception of the suprailiac site, both A-mode and B-mode ultrasound are equally capable of providing measurements of subcutaneous fat thickness with an accuracy of <1 mm at most sites.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Wagner DR, Cain DL, Clark NM. Validity and reliability of A-mode ultrasound for body composition assessment of NCAA division I athletes. PLoS ONE. 2016;11:e0153146.
Wagner DR. Ultrasound as a tool to assess body fat. J Obes. 2013;2013:280713.
Booth RAD, Goddard BA, Paton A. Measurement of fat thickness in man: a comparison of ultrasound, Harpenden calipers and electrical conductivity. Br J Nutr. 1966;20:719–25.
Loenneke JP, Barnes JT, Wagganer JD, Wilson JM, Lowery RP, Green CE, et al. Validity and reliability of an ultrasound system for estimating adipose tissue. Clin Physiol Funct Imaging. 2014;34:159–62.
Ulbricht L, Neves EB, Ripka WL, Romaneli EFR. Comparison between body fat measurements obtained by portable ultrasound and caliper in young adults. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:1952–5.
Utter AC, Hager ME. Evaluation of ultrasound in assessing body composition of high school wrestlers. Med Sci Sports Exerc. 2008;40:943–9.
Johnson KE, Naccarato IA, Corder MA, Repovich W. Validation of three body composition techniques with a comparison of ultrasound abdominal fat depths against an octopolar bioelectrical impedance device. Int J Exerc Sci. 2012;5:205–13.
Schoenfeld BJ, Aragon AA, Moon J, Krieger JW, Tiryaki-Sonmez G. Comparison of amplitude-mode ultrasound versus air displacement plethysmography for assessing body composition changes following participation in a structured weight-loss programme in women. Clin Physiol Funct Imaging. 2016. https://doi.org/10.1111/cpf.12355.
Baranauskas MN, Johnson KE, Juvancic-Heltzel JA, Kappler RM, Richardson L, Jamieson S, et al. Seven-site versus three-site method of body composition using BodyMetrix ultrasound compared to dual-energy X-ray absorptiometry. Clin Physiol Funct Imaging. 2015;37:317–21.
Johnson KE, Miller B, Juvancic-Heltzel JA, Agnor SE, Kiger DL, Kappler RM, et al. Agreement between ultrasound and dual-energy X-ray absorptiometry in assessing percentage body fat in college-aged adults. Clin Physiol Funct Imaging. 2014;34:493–6.
Loenneke JP, Barnes JT, Wagganer JD, Pujol TJ. Validity of a portable computer-based ultrasound system for estimating adipose tissue in female gymnasts. Clin Physiol Funct Imaging. 2014;34:410–2.
Ripka WL, Ulbricht L, Menghin L, Gewehr PM. Portable A-mode ultrasound for body composition assessment in adolescents. J Ultrasound Med. 2016;35:755–60.
Smith-Ryan AE, Fultz SN, Melvin MN, Wingfield HL, Woessner MN. Reproducibility and validity of A-mode ultrasound for body composition measurement and classification in overweight and obese men and women. PLoS ONE. 2014;9:e91750 https://doi.org/10.1371/journal.pone.0091750
Jackson AS, Pollock ML. Generalized equations for predicting body density of men. Br J Nutr. 1978;40:487–504.
Jackson AS, Pollock ML, Ward A. Generalized equations for predicting body density of women. Med Sci Sports Exerc. 1980;12:175–82.
Heyward VH, Wagner DR. Applied Body Composition Assessment. 2nd ed. Champaign, IL: Human Kinetics; 2004. pp. 51-59.
Müller W, Lohman TG, Stewart AD, Maughan RJ, Meyer NL, Sardinha LB, et al. Subcutaneous fat patterning in athletes: selection of appropriate sites and standardization of a novel ultrasound measurement technique: ad hoc working group on body composition, health and performance, under auspices of the IOC Medical Commission. Br J Sports Med. 2016;50:45–54.
Jones PRM, Davies PSW, Norgan NG. Ultrasonic measurements of subcutaneous adipose tissue thickness in man. Am J Phys Anthropol. 1986;71:359–63.
Weiss LW, Clark FC. Three protocols for measuring subcutaneous fat thickness on the upper extremities. Eur J Appl Physiol. 1987;56:217–21.
Weiss LW, Clark FC. Subcutaneous fat measurements of the leg using three protocols. J Sports Med Phys Fit. 1987;27:437–42.
Müller W, Horn M, Fürhapter-Rieger A, Kainz P, Kröpfl, Maughan RJ, et al. Body composition in sport: a comparison of a novel ultrasound imaging technique to measure subcutaneous fat tissue compared with skinfold measurement. Br J Sports Med. 2013;47:1028–35.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Wagner, D.R., Thompson, B.J., Anderson, D.A. et al. A-mode and B-mode ultrasound measurement of fat thickness: a cadaver validation study. Eur J Clin Nutr 73, 518–523 (2019). https://doi.org/10.1038/s41430-018-0085-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-018-0085-2
This article is cited by
-
The role of age in the physiological adaptations and psychological responses in bikini-physique competitor contest preparation: a case series
Journal of the International Society of Sports Nutrition (2021)
-
Reliability of body composition assessment using A-mode ultrasound in a heterogeneous sample
European Journal of Clinical Nutrition (2021)
-
Microstrip sensor for product quality monitoring
Journal of Computational Electronics (2020)