Abstract
Background/objectives
Recently, the role of a low-carbohydrate diet in diabetes management has generated interest with claims being made regarding its superiority over the traditional high-carbohydrate, low-fat dietary approach. This systematic review and meta-analysis evaluated the interpretation and effect of a low-carbohydrate diet in the management of type 2 diabetes.
Subjects/methods
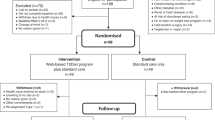
Randomised controlled trials were searched for which included adults with type 2 diabetes aged 18 years or more. The intervention was a low-carbohydrate diet as defined by the author compared to a control group of usual care. MEDLINE, EMBASE, CINAHL, Cochrane Central Register of Controlled Trials, ISRCTN, ProQuest and opengrey.eu were searched. Independent experts were contacted and reference lists of selected papers were checked. Results were analysed descriptively and meta-analyses were completed to include trials that presented data at 1 year.
Results
Eighteen studies (n = 2204) were eligible for inclusion within the systematic review. The definition of a low-carbohydrate diet varied. At trial end, the descriptive analysis suggested that the low-carbohydrate intervention arm (LCIA) may promote favourable outcomes in terms of HbA1c, triglycerides and HDL cholesterol. The LCIA demonstrated reduced requirements for diabetes medication, which may have reduced the observed benefit of dietary carbohydrate restriction on HbA1c. Seven studies provided data to be included in the meta-analyses at 1 year. The meta-analyses showed statistical significance in favour of the LCIA for HbA1c (estimated effect = −0.28%, 95% CI −0.53 to −0.02, p = 0.03; χ 2 = 13.15, df = 6, p = 0.03; I 2 = 54%), HDL cholesterol (estimated effect = 0.06 mmol/L, 95% CI 0.04–0.09, p < 0.00001; χ 2 = 6.05, df = 6, p = 0.42; I 2 = 1%), triglycerides (estimated effect = −0.24 mmol/L, 95% CI −0.35 to −0.13, p < 0.0001; χ 2 = 1.88, df = 6, p = 0.93; I 2 = 0%) and systolic blood pressure (estimated effect = −2.74 mmHg, 95% CI −5.27 to −0.20, p = 0.03; χ 2 = 10.54, df = 6, p = 0.10; I 2 = 43%). Meta-analyses for weight, total cholesterol, LDL cholesterol and diastolic blood pressure did not demonstrate a statistically significant difference between interventions.
Dietary adherence was an issue in most studies. A very low-carbohydrate diet (<50 g/day) seems unrealistic in this population, however, a low-carbohydrate diet (<130 g/day) appears to be achievable. Improved clinical outcomes were observed in some studies as a result of achieving a low- or moderate-carbohydrate diet.
Fifteen out of 18 studies were considered high risk of bias, with performance bias being a common issue.
Conclusions
Reducing dietary carbohydrate may produce clinical improvements in the management of type 2 diabetes. Further research is needed to understand the true effect of dietary carbohydrate restriction on HbA1c independent of medication reduction and to address known issues with adherence to this dietary intervention. Clarity is needed regarding appropriate classification of a low-carbohydrate diet.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
World Health Organization. Global status report on noncommunicable diseases. Geneva: World Health Organization; 2014.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442.
Diabetes UK. Diabetes: facts and stats. https://www.diabetes.org.uk/Documents/Position%20statements/Facts%20and%20stats%20June%202015.pdf. Accessed 10 Jan 2016.
Dyson P. Low carbohydrate diets and type 2 diabetes: what is the latest evidence? Diabetes Ther. 2015;6:411–24.
Diabetes UK. Evidence-based nutrition guidelines for the prevention and management of diabetes. London: Diabetes UK; 2011.
Evert AB, Boucher JL, Cypress M, Dunbar SA, Franz EJ, Neumiller JJ, et al. Position statement: nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care. 2013;36:3821–42.
Scientific Advisory Committee on Nutrition. (2015) Carbohydrates and Health. TSO, London, https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/445503/SACN_Carbohydrates_and_Health.pdf
Feinman RD, Pogozelskim WK, Astrip A, Bernstein RK, Fine EJ, Westman EC, et al. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutr. 2015;31:1–13.
Castañeda-Gonzales LM, Bacardi Gascon M, Jimenez Cruz A. Effects of low carbohydrate diets on weight and glycemic control among type 2 diabetes individuals: a systematic review of RCT greater than 12 weeks. Nutr Hosp. 2011;26:1270–6.
Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928
Thomas JG, Bond DS, Phelan S, Hill JO, Wing RR. Weight-loss maintenance for 10 years in the National Weight Control Registry. Am J Prev Med. 2014;46:17–23.
Little RR, Rohlfing CL, Sacks DB, National Glycohemoglobin Standardization Program(NGSP) Steering Committee Status of haemoglobin A1c measurement and goals for improvement: from chaos to order for improving diabetes care. Clin Chem. 2011;57:205–14
NHS Diabetes. (2009) Self-monitoring of blood glucose in non-insulin treated type 2 diabetes. Aberdeen Health Technology Assessment Group, Aberdeen, http://webarchive.nationalarchives.gov.uk/20130513172055/http:/www.diabetes.nhs.uk/document.php?o=238
Khaw KT, Wareham N, Luben R, Bingham S, Oakes S, Welch A, et al. Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of European prospective investigation of cancer and nutrition (EPIC-Norfolk). Br Med J. 2001;322:15–18.
Elbourne DR, Altman DG, Higgins JPT, Curtin F, Worthingtond HV, Vail A, Meta-analyses involving cross-over trials: methodological issues. Int J Epidemiol. 2002;31:140–9
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Chichester: Wiley; 2009.
Higgins JPT, Green S on behalf of The Cochrane Collaboration. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 (updated March 2011). http://www.cochrane-handbook.org. Accessed 9 Jan 2016.
Elhayany A, Lustman A, Abel R, Attal-Singer J, Vinker S. A low carbohydrate Mediterranean diet improves cardiovascular risk factors and diabetes control among overweight patients with type 2 diabetes mellitus: a 1-year prospective randomized intervention study. Diabetes Obes Metab. 2010;12:204–9.
Rock CL, Flatt SW, Pakiz B, Taylor KS, Leone AF, Brelje K, et al. Weight loss, glycemic control, and cardiovascular disease risk factors in response to differential diet composition in a weight loss program in type 2 diabetes: a randomized controlled trial. Diabetes Care. 2014;37:1573–80.
Wolever TM, Gibbs AL, Mehling C, Chiasson JL, Connelly PW, Josse RG, et al. The Canadian Trial of Carbohydrates in Diabetes (CCD), a 1-y controlled trial of low-glycemic-index dietary carbohydrate in type 2 diabetes: no effect on glycated haemoglobin but reduction in C-reactive protein. Am J Clin Nutr. 2008;87:114–25.
Pohl M, Mayr P, Mertl-Roetzer M, Lauster F, Lerch M, Eriksen J, et al. Glycaemic control in type II diabetic tube-fed patients with a new enteral formula low in carbohydrates and high in monounsaturated fatty acids: a randomised controlled trial. Eur J Clin Nutr. 2005;59:1221–32.
Pohl M, Mayr P, Mertl-Roetzer M, Lauster F, Haslbeck M, Hipper B, et al. Glycemic control in patients with type 2 diabetes mellitus with a disease-specific enteral formula: stage II of a randomized, controlled multicenter trial. JPEN J Pareneter Enter Nutr. 2009;33:37–49.
Daly ME, Paisey R, Paisey R, Milward BA, Eccles C, Williams K, et al. Short-term effects of severe dietary carbohydrate-restriction advice in type 2 diabetes – a randomised controlled trial. Diabet Med. 2006;23:15–20.
Shirai K, Saiki A, Oikawa S, Teramoto T, Yamada N, Ishibashi S, et al. The effects of partial use of formula diet on weight reduction and metabolic variables in obese type 2 diabetic patients – multicenter trial. Obes Res Clin Pract. 2013;7:e43–54.
Tay J, Luscombe-Marsh ND, Thompson CH, Noakes M, Buckley JD, Wittert GA, et al. A very low-carbohydrate, low-saturated fat diet for type 2 diabetes management: a randomized trial. Diabetes Care. 2014;37:2909–18.
Westman EC, Yancy WS, Mayropoulos JC, Marquart M, McDuffie JR. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr Metab. 2008;5:36.
Jonasson L, Guldbrand H, Lundberg AK, Nystrom FH. Advice to follow a low-carbohydrate diet has favourable impact on low-grade inflammation in type 2 diabetes compared with advice to follow a low-fat diet. Ann Med. 2014;46:182–7.
Yamada Y, Uchida J, Izumi H, Tsukamoto Y, Inoue G, Watanabe Y, et al. A non-calorie-restricted low-carbohydrate diet is effective as an alternative therapy for patients with type 2 diabetes. Intern Med. 2013;53:13–19.
Mayer SB, Jeffreys AS, Olsen MK, McDuffie JR, Feinglos MN, Yancy WS. Two diets with different haemoglobin A1c and antiglycaemic medication effects despite similar weight loss in type 2 diabetes. Diabetes Obes Metab. 2014;16:90–93.
Davis NJ, Tomuta N, Schechter C, Isasi CR, Segal-Isaacson CJ, Stein D, et al. Comparative study of the effects of a 1-year dietary intervention of a low-carbohydrate diet versus a low-fat diet on weight and glycemic control in type 2 diabetes. Diabetes Care. 2009;32:1147–52.
Goldstein T, Kark JD, Berry EM, Adler B, Ziv E, Raz I. The effect of a low carbohydrate energy-unrestricted diet on weight loss in obese type 2 diabetes patients – a randomized controlled trial. E Spen Eur E J Clin Nutr Metab. 2011;6:e178–86.
Larsen RN, Mann NJ, Maclean E, Shaw JE. The effect of high-protein, low-carbohydrate diets in the treatment of type 2 diabetes: a 12 month randomised controlled trial. Diabetologia. 2011;54:731–40.
Tay J, Luscombe-Marsh ND, Thompson CH, Noakes M, Buckley JD, Wittert GA, et al. Comparison of low- and high-carbohydrate diets for type 2 diabetes management: a randomized trial. Am J Clin Nutr. 2015;102:780–90.
Guldbrand H, Dizdar B, Bunjaku B, Lindstrom T, Bachrach-Lindström M, Fredrikson M, et al. In type 2 diabetes, randomisation to advice to follow a low-carbohydrate diet transiently improves glycaemic control compared with advice to follow a low-fat diet producing a similar weight loss. Diabetologia. 2012;55:2118–27.
Esposito K, Maiorino MI, Ciotola M, Di Palo C, Scognamiglio P, Gicchino M, et al. Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann Intern Med. 2009;151:306–14.
Kirk JK, Graves DE, Craven TE, Lipkin EW, Austin M, Margolis KL. Restricted-carbohydrate diets in patients with type 2 diabetes: a meta-analysis. J Am Diet Assoc. 2008;108:91–100.
Van Wyke HJ, Davis RE, Davis JS. A critical review of low-carbohydrate diets in people with type 2 diabetes. Diabet Med. 2015. https://doi.org/10.1111/dme.12964
National Institute of Health and Care Excellence. Type 2 diabetes in adults: management. NG28. London: NICE; 2015.
Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Sato M, et al. Influence of fat and carbohydrate proportions on the metabolic profile in patients with type 2 diabetes: a meta-analysis. Diabetes Care. 2009;32:959–65.
Hu T, Bazzano LA. The low-carbohydrate diet and cardiovascular risk factors: evidence from epidemiologic studies. Nutr Metab Cardiovasc Dis. 2014;24:337–43.
De Souza RJ, Mente A, Maroleanu A, Cozma AI, Ha V, Kishibe T, et al. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. Br Med J. 2015;351:h3978.
Hooper L, Marin N, Abdelhamid A, Davey Smith G. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst Rev. 2015;10:CD011737.
National Institute of Health and Care Excellence. Cardiovascular disease: risk assessment and reduction, including lipid modification. CG181. London: NICE; 2016.
American Diabetes Association. Standards of medical care in diabetes – 2016 Abridged for primary care providers. Clin Diabetes. 2016;34:3–21.
Pogozelski W, Arpaia N, Priore S. The metabolic effects of low-carbohydrate diets and incorporation into a biochemistry course. Biochem Mol Biol Educ. 2005;33:91–100.
Spritzler F. A low-carbohydrate, whole-foods approach to managing diabetes and prediabetes. Diabetes Spectr. 2015;25:238–43.
Paddon-Jones D, Westman E, Mattes RD, Wolfe RR, Astrup A, Westerterp-Plantenga M. Protein weight management, and satiety. Am J Clin Nutr. 2008;87:1558S–61S.
National Institutes of Health. US Renal Data System, USRDS 2010. Annual data report: atlas of chronic kidney disease and end-stage renal disease in the United States. United States: National Institute of Diabetes and Digestive and Kidney Diseases; 2010.
Cuenca-Sánchez M, Navas-Carrillo D, Orenes-Piñero E. Controversies surrounding high-protein diet intake: satiating effect and kidney and bone health. Adv Nutr. 2015;16:260–6.
Bowman SA, Spence JT. A comparison of low-carbohydrate vs. high-carbohydrate diets: energy restriction, nutrient quality and correlation to body mass index. J Am Coll Nutr. 2002;21:268–74.
Calton JB. Prevalence of micronutrient deficiency in popular diet plans. J Int Soc Sports Nutr. 2010;7:24.
Crowe TC. Safety of low-carbohydrate diets. Obes Rev. 2005;6:235–45.
Diabetes UK. Low-carbohydrate diets for people with type 2 diabetes. London: Diabetes UK; 2011.
Acknowledgements
R.H. would like to thank the Nutrition and Dietetic Department at Bradford Teaching Hospitals NHS Foundation Trust for their support of this project. R.H. would also like to pass on thanks to the Division of Nursing, Midwifery and Social Work at University of Manchester and the National Institute of Health Research for offering support throughout the project. Special thanks also go to Dr B. Phillips from the University of York for his expert advice offered to the authors to assist with their meta-analyses. This review was completed within a NIHR-funded Masters in Clinical Research.
Author contributions
R.H. was responsible for database searching, study selection, risk of bias assessment, data extraction, data analysis, meta-analysis and compiling the report. M.C. contributed to data extraction and meta-analyses. C.B. reviewed the database searching, study selection, risk of bias assessment and data extraction. All authors commented on drafts of the paper and agreed on the final version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Huntriss, R., Campbell, M. & Bedwell, C. The interpretation and effect of a low-carbohydrate diet in the management of type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. Eur J Clin Nutr 72, 311–325 (2018). https://doi.org/10.1038/s41430-017-0019-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-017-0019-4
This article is cited by
-
The effects of Mediterranean diet on cardiovascular risk factors, glycemic control and weight loss in patients with type 2 diabetes: a meta-analysis
BMC Nutrition (2024)
-
A web-based low carbohydrate diet intervention significantly improves glycaemic control in adults with type 2 diabetes: results of the T2Diet Study randomised controlled trial
Nutrition & Diabetes (2023)
-
Embracing complexity: making sense of diet, nutrition, obesity and type 2 diabetes
Diabetologia (2023)
-
Dietary carbohydrate restriction augments weight loss-induced improvements in glycaemic control and liver fat in individuals with type 2 diabetes: a randomised controlled trial
Diabetologia (2022)
-
Benefits of Low Carbohydrate Diets: a Settled Question or Still Controversial?
Current Obesity Reports (2021)