Abstract
Background/objectives
Poorer motor development is reported in infants with iron deficiency (ID). The role of timing, duration and severity is unclear. We assessed relations between ID timing, duration, and severity and gross motor scores, neurological integrity, and motor behavior quality at 9 months.
Subjects/methods
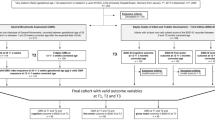
Iron status was determined at birth and 9 months in otherwise healthy term Chinese infants. The 9-month motor evaluation included the Peabody Developmental Motor Scale (PDMS-2), Infant Neurological International Battery (INFANIB), and motor quality factor. Motor outcomes were analyzed by ID timing (fetal–neonatal, infancy), duration, and severity. For severity, we also considered maternal iron status.
Results
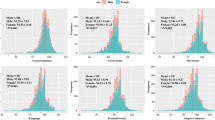
The data were available for 1194 infants. Iron status was classified as fetal–neonatal and infancy ID (n = 253), fetal–neonatal ID (n = 256), infancy ID (n = 288), and not ID (n = 397). Compared with not ID, infants with fetal–neonatal or infancy ID had lower locomotion scores (effect size ds = 0.19, 0.18) and those with ID in both periods (longer duration) had lower locomotion and overall PDMS-2 gross motor scores (ds = 0.20, 0.18); ID groups did not differ. More severe ID in late pregnancy was associated with lower INFANIB Vestibular function (p = 0.01), and total score (p = 0.03). More severe ID in infancy was associated with lower scores for locomotion (p = 0.03), overall gross motor (p = 0.05).
Conclusions
Fetal–neonatal and/or infancy ID was associated with lower overall gross motor development and locomotion test scores at 9 months. Associations with ID severity varied by ID timing: more severe ID in late pregnancy, poorer neurological integrity; more severe ID in infancy, poorer gross motor development.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Angulo-Barroso RM, Li M, Santos DCC, Bian Y, Sturza J, Jiang Y, et al. Iron supplementation in pregnancy or infancy and motor development: a randomized controlled trial. Pediatrics. 2016;137():e20153547.
Murray GK, Veijola J, Moilanen K, Miettunen J, Glahn DC, Cannon TD, et al. Infant motor development is associated with adult cognitive categorisation in a longitudinal birth cohort study. J Child Psychol Psychiatry. 2006;47:25–29.
Clearfield MW, Learning to walk changes infants’ social interactions. Infant Beh Dev. 2011;34:15–25
Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995-2011: A systematic analysis of population-representative data. Lancet Glob Health. 2013;1:e16–e25
Lozoff B, Beard J, Connor J, Felt B, Georgieff M, Schallert T, Long-lasting neural and behavioral effects of iron deficiency in infancy. Nutr Rev. 2006;64:S34–S43
Georgieff MK, Brunette KE, Tran PV. Early life nutrition and neural plasticity. Dev Psychopathol. 2015;27:411–23.
Chang S, Zeng L, Brouwer ID, Kok FJ, Yan H. Effect of iron deficiency anemia in pregnancy on child mental development in rural China. Pediatrics. 2013;131:e755–e63.
Tran TD, Tran T, Simpson JA, Tran HT, Nguyen TT, Hanieh S, et al. Infant motor development in rural Vietnam and intrauterine exposures to anaemia, iron deficiency and common mental disorders: a prospective community-based study. BMC Pregnancy Childbirth. 2014;14:8.
Hernandez-Martinez C, Canals J, Aranda N, Ribot B, Escribano J, Arija V. Effects of iron deficiency on neonatal behavior at different stages of pregnancy. Early Hum Dev. 2011;87:165–169.
Lozoff B, Jimenez E, Hagen J, Mollen E, Wolf AW. Poorer behavioral and developmental outcome more than 10 years after treatment for iron deficiency in infancy. Pediatrics. 2000;105:E51.
Gunnarsson BS, Thorsdottir I, Palsson G, Gretarsson SJ. Iron status at 1 and 6 years versus developmental scores at 6 years in a well-nourished affluent population. Acta Paediatr. 2007;96:391–395.
Shafir T, Angulo-Barroso R, Calatroni A, Jimenez E, Lozoff B. Effects of iron deficiency on patterns of motor development over time. Hum Mov Sci. 2006;25:821–838.
Lozoff B, Jiang Y, Li X, Zhou M, Richards B, Xu G, et al. Low-dose iron supplementation in infancy modestly increases infant iron status at 9 months without decreasing growth or increasing illness in a randomized clinical trial in rural China. J Nutr. 2016;146:612–621.
Zhao G, Xu G, Zhou M, Jiang Y, Richards B, Clark KM, et al. Prenatal iron supplementation reduces maternal anemia, iron deficiency, and iron deficiency anemia in a randomized clinical trial in rural China, but iron deficiency remains widespread in mothers and neonates. J Nutr. 2015;145:1916–1923.
Cook JD, Flowers CH, Skikne BS. The quantitative assessment of body iron. Blood. 2003;101:3359–3364.
WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System. Geneva: World Health Organization (WHO/NMH/NHD/MNM/11.1); 2011.
Folio MK, Fewell R. Peabody Developmental Motor Scales: Examiner’s Manual. 2nd ed. Austin, TX: PRO-ED, Inc.; 2000.
Zhao G, Bian Y, Li M. Impact of passing items above the ceiling on the assessment results of Peabody developmental motor scales. Beijing Da Xue Xue Bao. 2013;45:928–932.
Ellison PH, Horn JL, Browning CA. Construction of an Infant Neurological International Battery (INFANIB) for the assessment of neurological integrity in infancy. Phys Ther. 1985;65:1326–1331.
Bayley N. Bayley Scales of Infant Development. 2nd ed. San Antonio: The Psychological Corporation; 1993.
Sanhe City People’s Government. Sanhe City People’s Government on the issuance of “Sanhe 2013 annual public housing security plan”. Available at: http://www.he.xinhuanet.com/zfwq/sanhe/zhengwu/zhengwu/2013-10/21/c_117803056.htm 2013; (cited 1 June 2015).
Liao W, Wen EY, Li C, Chang Q, Lv KL, Yang W, He ZM, Zhao CM. Predicting neurodevelopmental outcomes for at-risk infants: reliability and predictive validity using a Chinese version of the INFANIB at 3, 7 and 10 months. BMC Pediatr. 2012;12:72 https://doi.org/10.1186/1471-2431-12-72
Blayney AW. Vestibular disorders. In: Adams DA, Cinnamond MJ eds. Paediatric Otolaryngology 6th ed. Scott-Brown’s Otolaryngology: Vol. 6. (Chapter 12). CRC Press: Butterworth Heinemann, Oxford; 1997: 1-29.
O’Reilly R, Grindle C, Zwicky EF, Morlet T, Development of the vestibular system and balance function: differential diagnosis in the pediatric population. Otolaryngol Clin North Am. 2011;44:251–271
Beraneck M, Lambert FM, Sadeghi SG. Functional development of the vestibular system: Sensorimotor pathways for stabilization of gaze and posture. In: Valera Nieto R, Romani eds. Development of Auditory and Vestibular Systems. Academic Press: San Diego; 2014: 449-487.
Rothwell J. Control of Human Voluntary Movement. London: Chapman & Hall; 1994.
Konner M. Universals of behavioral development in relation to brain myelination. In: Gibson KR, Petersen AC, eds.. Brain Maturation and Cognitive Development. New York: Aidine De Gruyter; 1991. p. 181–223.
Pollitt E, Gorman K. Long-term developmental implications of motor maturation and physical activity in infancy in a nutritionally at risk population. Activity, energy expenditure and energy requirements of infants and children: Proceedings of International Dietary Energy Consultancy Group 1990. Lausanne, Switzerland; 1990: 279-296.
Adolph KE, Eppler MA, Gibson EJ. Development of perception of affordances. Adv Infant Res. 1993;8:51–98.
Campos JJ, Kermoian R, Zumbahlen MR. Socioemotional transformation in the family system following infant crawling onset. In: Eisenberg N, Fabes R, eds. Emotion and Its Regulation in Early Development. San Francisco, CA: Josey Bass; 1992. p. 110.
Lozoff B, Klein NK, Nelson EC, McClish DK, Manuel M, Chacon ME, Behavior of infants with iron deficiency anemia. Child Dev. 1998;69:24–36
Perez EM, Hendricks MK, Beard JL, Murray-Kolb LE, Berg A, Tomlinson M, et al. Mother-infant interaction and infant development are altered by maternal iron deficiency anemia. J Nutr. 2005;135:850–855.
Armony-Sivan R, Kaplan-Estrin M, Jacobson SW, Lozoff B. Iron-deficiency anemia in infancy and mother-infant interaction during feeding. J Dev Behav Pediatr. 2010;31:526–532.
Corapci F, Radan AE, Lozoff B. Iron deficiency in infancy and mother-child interaction at 5 years. J Behav Dev Pediatr. 2006;27:371–378.
Acknowledgements
This work was funded by a grant from the US National Institutes of Health (R01 HD052069), which included funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the Office of Dietary Supplements, provided support for the infancy study and laboratory measures of iron status for mothers and infants, Betsy Lozoff, Principal Investigator. Vifor Pharma, Ltd. provided financial support for the pregnancy study. São Paulo Research Foundation – FAPESP/Brazil (2014/00018-0) and Methodist University of Piracicaba – UNIMEP/Brazil provided financial support for Denise CC Santos. The content is solely the responsibility of the authors and does not necessarily represent the official views of funding sources. Authors had full control of primary data and did not have an agreement with the funders that limited their ability to complete the research as planned.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Betsy Lozoff was an unpaid speaker at 2 seminars supported by Lee’s Pharmaceutical Holdings Limited. The topic was iron deficiency and child development (Shanghai, 11 April 2010, and Beijing, 15 May 2011). The company covered hotel accommodations and, for the 2011 seminar, internal airfare between Hangzhou and Beijing. The authors declare that they have no other competing interests.
Additional information
Denise C. C. Santos, Rosa M. Angulo-Barroso and Ming Li contributed equally to this work.
Rights and permissions
About this article
Cite this article
Santos, D.C.C., Angulo-Barroso, R.M., Li, M. et al. Timing, duration, and severity of iron deficiency in early development and motor outcomes at 9 months. Eur J Clin Nutr 72, 332–341 (2018). https://doi.org/10.1038/s41430-017-0015-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-017-0015-8
This article is cited by
-
Differentiation between fetal and postnatal iron deficiency in altering brain substrates of cognitive control in pre-adolescence
BMC Medicine (2023)
-
Effects of delayed cord clamping on neonatal jaundice, phototherapy and early hematological status in term cesarean section
Italian Journal of Pediatrics (2021)