Abstract
Adipose-derived stem cells (AdSCs), a type of mesenchymal stem cell, are expected to be applicable to regenerative medicine and cellular delivery systems. The maintenance of cell multipotency and control of the differentiation direction are important for these applications. However, the differentiation direction of these cells is widely believed to depend on the physical properties of their scaffold. In this study, we explored whether the multipotency of AdSCs, that is, their ability to differentiate into multiple cells, is maintained when they are removed from injectable polymer (IP) hydrogels with various degrees of cross-linking and induced to differentiate into osteoblasts and adipocytes. We confirmed that AdSCs cultured in IP hydrogels maintained an undifferentiated state. However, their differentiation into osteoblasts and adipocytes cannot be ensured; specifically, the multipotency of AdSCs may decrease when they are cultured in IP hydrogels. When cultured in an IP hydrogel with extreme softness and poor cell adhesion properties, the AdSCs remained in an undifferentiated state, but their multipotency was reduced. These results provide important insights into stem cell delivery systems using IP hydrogels.
Similar content being viewed by others
Introduction
Embryonic stem (ES) and induced pluripotent stem (iPS) cells exhibit pluripotency and can differentiate into cells that make up various organs [1, 2]. These stem cells are widely believed to be useful for treating previously incurable injuries and diseases. However, the practical applications of iPS and ES cells have raised concerns about ethics, safety, procurement, and cost. Adipose-derived stem cells (AdSCs), a type of somatic stem cells, have attracted attention as an easily available stem cell source. Zuk et al. described AdSCs as mesenchymal stem cells (MSCs) isolated from adipose tissue [3]. AdSCs have been reported to be able to differentiate only into cells belonging to the mesoderm, such as osteoblasts, adipocytes, and myoblasts, and their differentiation direction is generally considered to be limited. However, in recent years, differentiation into endoderm- and ectoderm-derived cells (e.g., nerve cells, etc.) has been confirmed [4,5,6,7]. In addition, AdSCs promote cell proliferation, anti-inflammation, and angiogenesis by secreting cytokines [8,9,10,11]; thus, these cells show promising applications in cellular therapy. For example, the treatment of ischemic heart disease by AdSC administration has been reported [12,13,14,15,16]. The recovery of cardiac function in a mouse myocardial infarction model following infusion with AdSCs has also been described. The injection of AdSCs with a hydrogel scaffold has also been investigated to achieve effective recovery from myocardial infarctions [17, 18].
Injectable polymers (IPs) [19,20,21] are materials that exist in a sol state outside the body but form gels in situ when the aqueous polymer solution is injected into the body. In particular, temperature-responsive IPs that form a hydrogel upon injection into the body have attracted attention [22,23,24,25]. Such IPs may potentially be applied as biomedical materials in regenerative medicine (as cellular delivery systems and tissue regeneration scaffolds) [26, 27], drug delivery systems [28, 29], and other applications [30,31,32,33,34]. However, because most temperature-responsive IP hydrogels are physically cross-linked systems, they are limited by their relatively low elastic modulus and short in vivo duration. Therefore, IP systems with sufficient gel duration and physical strength for the desired application must be developed.
In recent years, several reports have been published on IP systems that can form covalent cross-links after temperature-responsive gelation via chemical reactions such as the Michael addition-type thiol-ene reaction [35, 36], condensation reactions using activated esters [37], and click reactions [38, 39]. The Michael addition-type reaction can proceed under physiological conditions (37 °C, pH 7.4) and can involve biomolecules (i.e., it is bioorthogonal). We previously developed a temperature-responsive IP system with covalent cross-linking ability by using an ABA-type triblock copolymer of poly(ε-caprolactone-co-glycolide) and poly(ethylene glycol) (PEG), hereafter referred to as tri-PCG [40, 41]. We then introduced acryloyl groups at both termini of tri-PCG to produce tri-PCG-acryl and mixed tri-PCG-acryl and tri-PCG micellar solutions containing dipentaerythritolhexakis(3-mercaptopropionate) (DPMP) as a hydrophobic hexafunctional thiol [42]. Thus, we succeeded in constructing IP systems exhibiting covalent cross-linking ability in response to temperature increases via the thiol-ene reaction. The maximum duration of the IP hydrogel exceeded 90 d, and the duration and mechanical strength (storage modulus) of the IP hydrogel could be controlled by changing the mixing ratio of tri-PCG-acryl in the IP formulation. We also reported that AdSCs embedded in this covalent bond-forming IP system could effectively treat ischemic heart disease [43].
Stem cells differentiate into different cell types depending on the elastic modulus of the culture matrix [44, 45]. Suppressing unintended differentiation and maintaining multipotency are desirable when performing regenerative medicine using the multipotency or inherent properties of stem cells. These requirements highlight the necessity of constructing a system that can maintain undifferentiated stem cells by default and differentiate them into target cells on demand using differentiation-inducing factors.
In this study, we investigated whether the undifferentiated state and multipotency of AdSCs could be maintained in IP hydrogels. We also examined the effect of the mechanical strength of the IP hydrogel on these properties by using a covalent bond-forming IP hydrogel system based on tri-PCG-acryl, which features controllable mechanical strength. Initially, we attempted to maintain the undifferentiated state of the AdSCs in the IP hydrogel and then differentiate them into the intended direction after culture by applying differentiating factors in the IP hydrogel or recovery from the IP hydrogel (Fig. 1). However, we found that the differentiation ability of the cells decreased after culture, which defeats our original purpose. These results reveal that the chemical and physical properties of the scaffold hydrogel should be carefully controlled. These phenomena are extremely important information for future attempts at tissue engineering using stem cells in such gels.
Materials and methods
Materials
Tri-PCG and tri-PCG-acryl were synthesized according to previously reported methods [42]. The materials for the synthesis and synthetic details are described in the Supplementary Information (SI). A LabAssay ALP kit was purchased from FUJIFILM Wako Pure Chemical Co., Ltd. (Osaka, Japan). Water was purified using a Millipore Elix UV3 Direct-Q UV system (Merck, Darmstadt, Germany). Dulbecco’s phosphate-buffered saline (PBS) (−) was purchased from Nissui Pharmaceutical Co., Ltd. (Tokyo, Japan). Dulbecco’s modified Eagle’s medium nutrient mixture F-12 (DMEM/F12), collagenase type VIII, 1% BSA solution, and Coomassie protein assay reagent were obtained from Sigma‒Aldrich (St. Louis, MO, USA). Ethylenediamine-N,N,N’,N’-tetraacetic acid and disodium salt (EDTA·2Na) were purchased from Dojindo Laboratories (Kumamoto, Japan). AdSC culture medium (KBM ADSC-1) and a lipid assay kit were purchased from Cosmo Bio Co., Ltd. (Tokyo, Japan). Fetal bovine serum (FBS) was purchased from Biowest (Nuaillé, France). FITC anti-mouse CD31, CD45, and CD90.2, FITC anti-mouse/human CD44, FITC anti-mouse/rat CD29, and PE anti-mouse CD34 antibodies were obtained from BioLegend (San Diego, CA, USA). NucleoSpin RNA and a PrimeScriptTM RT Reagent Kit (Perfect Real Time) were purchased from Takara Bio Inc. (Shiga, Japan). SsoAdvancedTM Universal SYBER Green Mix was purchased from Bio-Rad Laboratories Inc. (Hercules, CA, USA). Hank’s balanced salt solution (HBSS) was obtained from Thermo Fisher Scientific (Waltham, MA, USA). StemXvivo® Osteogenic Supplement, Osteogenic/Adipogenic Base Media, and Adipogenic Supplement were purchased from R&D Systems, Inc. (Minneapolis, MN, USA).
Animals
Nine-week-old C57BL/6 N male mice were purchased from SHIMIZU Laboratory Supplies Co., Ltd. (Kyoto, Japan). AdSCs were collected from the mice as reported previously [13, 43]. Prior to the experiments, the mice were anesthetized with isoflurane using a small animal anesthesia station (DS Pharma Biomedical Co. Ltd., Osaka, Japan). All animal experiments were performed following the guidelines listed at Kansai University and approved by the Ethical Committee for Animal Experiments of Kansai University (7 May 2019; Identification No. 1903). This study was carried out in compliance with the ARRIVE guidelines.
Measurements
Quantitative real-time reverse-transcription polymerase chain reaction (RT‒qPCR) was performed on a CFX96 deep-well real-time system (Bio-Rad Laboratories, Inc.). Flow cytometry (FCM) was performed using a Gallios flow cytometer (Beckman Coulter, Inc., CA, USA) with an Ar-ion coherent beam laser (488 nm). The UV absorbance of the microplated solutions was measured using an iMark microplate reader (Bio-Rad Laboratories, Inc.).
Evaluation of surface expression markers for AdSCs
We collected AdSCs from 9-week-old male C57BL/6 N mice (SHIMIZU Laboratory Supplies Co., Ltd., Kyoto, Japan), as reported previously [13, 43], and confirmed the expression of AdSC-specific surface markers in these cells. The mice were euthanized by blood removal from the epigastric cavity using a syringe with a 26–29 G needle under isoflurane anesthesia. Subcutaneous inguinal adipose tissue was collected and placed on a culture dish (ϕ = 3.5 cm). The adipose tissue was cut into small pieces with scissors and placed in a 15 mL centrifuge tube. HBSS (3 mL) containing BSA (1%) and collagenase VIII solution (2 mg/mL) was added to the tube at 37 °C. After incubation at 37 °C for 30 min with inversion and mixing, 3 mL of DMEM/F12 medium containing 10% FBS was added to stop the enzymatic reaction. The top fat layer was removed by suction, and the supernatant was passed through a cell strainer (40 μm, BD Bioscience, Franklin Lake, NJ, USA) and collected into a 50 mL tube. Centrifugation (1200 rpm × 5 min) was performed to remove the supernatant. The cell pellet was suspended in PBS(−) containing 1 mM EDTA (1 mL) up to a volume of 10 mL. Centrifugation was performed once more, and the supernatant was removed. The cell pellet was suspended in DMEM/F12 or KBM ADSC-1 containing 10% FBS, seeded in culture dishes, and cultured in a humidified atmosphere containing 5% CO2 for 3 d at 37 °C to obtain AdSCs as adherent cells.
The cell suspension (2 × 105 cells/500 μL) was centrifuged (400 g) at 4 °C for 5 min, and the supernatant was removed. Antibody solution (100 μL) was added to the cells. Incubation in an ice bath was then performed for 30 min. FITC anti-mouse/rat CD29 (0.5 mg/mL), FITC anti-mouse/human CD44 (0.5 mg/mL), and FITC anti-mouse CD90.2 (0.5 mg/mL) antibodies were used as positive markers, whereas FITC anti-mouse CD31 (0.5 mg/mL), PE anti-mouse CD34 (0.2 mg/mL), and FITC anti-mouse CD45 (0.5 mg/mL) antibodies were used as negative markers. After incubation, the cells were washed twice with PBS(−), added to PBS (500 µL), and then subjected to FCM measurements.
AdSC culture in the IP hydrogels and quantification of gene expression
The preparation of the IP formulations (tri-PCG/DPMP + tri-PCG-acryl mixture containing 16–33 wt% tri-PCG-acryl in the total polymer) and confirmation of their sol–gel transition are described in Figs. S1 and S2 in the SI and our previous study [42]. The IP formulations (tri-PCG only or a mixture of tri-PCG-acryl and tri-PCG/DPMP aqueous solutions) were sterilized by filtration. The AdSC suspension (100 μL) and IP formulation (100 μL) were mixed and dispensed into sterilized Eppendorf tubes. After gelation by incubation at 37 °C for 30 min, KBM ADSC-1 (400 µL) was gently placed on top of an IP gel containing AdSCs. The cells were then further incubated in a humid atmosphere containing 5% CO2 at 37 °C. An aliquot of the supernatant (200 μL) was removed and replaced with fresh KBM ADSC-1 every 2 d. Next, the IP gel was broken, and the homogeneous suspension was collected by repeated pipetting with PBS(−) (3 mL). The cells were collected by centrifugation. This operation was repeated three times to remove the IPs and DPMP.
mRNA extraction and RT‒qPCR were performed using NucleoSpin RNA and PrimeScript RT reagents, respectively, according to the manufacturer’s instructions. The mRNA levels of OCT4 [46], Nanog [47], and Sox2 [48] as undifferentiated markers and AFP [49], Brachyury [50], and Pax6 [51] as embryonic markers were quantified using the Bio-Rad CFX96 Deep Well Real-Time System, SsoAdvanced Universal SYBR Green Supermix, and primers obtained from Eurofin Genomics LLC (Louisville, KY, USA) (see the SI). GAPDH was used as the housekeeping gene in all experiments. Relative RNA expression was determined using Eq. (1):
where ΔCt = Ct of the gene of interest − Ct. Ct: cycle threshold.
Differentiation of AdSCs into osteoblasts in the IP hydrogel (Protocol (1))
Tri-PCG-acryl (20 wt%) and tri-PCG/DPMP (20 wt%) were prepared separately via the protocols described above using osteogenic differentiation medium (StemXVivo) instead of ADSC-1 and then mixed and stirred with a vortex mixer to induce osteogenic differentiation (+). The obtained mixture (IP formulation; 75 µL) was sterilized by filtration, mixed with the cell suspension in the same medium (25 µL), and dispensed into a sterilized Eppendorf tube (100 μL). After gelation by incubation at 37 °C for 30 min, the cells were further incubated in a humidified atmosphere containing 5% CO2 at 37 °C for 3 d. The osteogenic differentiation medium (1000 µL) was gently placed on top of the IP gel containing AdSCs, and the cells were further incubated for 14 or 21 d in a humidified atmosphere containing 5% CO2 at 37 °C. The supernatant was replaced with medium every 2 d. Next, the IP gel was broken, and a homogeneous suspension was obtained by repeated pipetting with PBS( − ) (3 mL). The cells were collected by centrifugation. This operation was repeated three times to remove the IPs and DPMP. The collected cells were seeded in 24-well plates at a density of 2 × 104 cells/well and cultured in osteogenic differentiation medium. The medium was replaced every few days. AdSCs treated via the same protocol using KBM ADSC-1 instead of osteogenic differentiation medium were also prepared; these cells were considered osteogenic differentiation induction (−) cells. AdSCs cultured on tissue culture polystyrene (TCPS) dishes were prepared using osteogenic differentiation medium (osteogenic differentiation induction (+)) or KBM ADSC-1 (osteogenic differentiation induction (−)). The AdSC suspensions were used for alkaline phosphatase (ALP), total protein quantification, and RT‒qPCR assays.
Differentiation of AdSCs into osteoblasts on TCPS after incubation in the IP hydrogel (Protocol (2))
AdSCs were incubated in the IP hydrogel via Protocol (1) using KBM ADSC-1 (osteogenic differentiation induction (−)) for 7 d. The obtained cells were seeded in 24-well TCPS plates at a density of 2 × 104 cells/well and cultured for 14 or 21 d in osteogenic differentiation medium (osteogenic differentiation induction (+)). The obtained cells were subjected to ALP assays, total protein quantification, and RT‒qPCR assays. The ALP assay and total protein quantification procedures are described in the SI.
Differentiation of AdSCs into adipocytes on TCPS after incubation in the IP hydrogel
AdSCs were cultured in the IP formulation containing KBM ADSC-1 (without differentiation) for 7 d. The obtained cells were then seeded in 24-well TCPS plates at a density of 2 × 104 cells/well and cultured for 14 or 21 d in StemXvivo® adipogenic differentiation medium. The culture medium was removed, and each well was washed with PBS(−) (500 µL). Neutral buffered formalin solution (10%, 500 µL) was added to the wells for fixation. After incubation at 25 °C for 20 min, the fixed cells were washed with water (500 μL). ORO solution (500 μL) from the lipid assay kit was dispensed into the wells, and the plate was incubated at 25 °C for 15 min. The ORO solution was then removed, and the wells were washed three times with water and dried. The extraction solution from the lipid assay kit (500 μL) was added to the wells, and the solution was incubated at 25 °C for 30 min to extract the dye. Finally, the absorbance of the extracted solution was measured at 570 nm using a spectrophotometer.
Statistical analysis
Statistical significance was determined using the Tukey–Kramer method.
Results and discussion
Characterization of AdSCs collected from mice
We confirmed the expression of MSC-specific surface markers in cells collected from mice by FCM (see Fig. S3 in the SI). Most cells expressed the positive markers CD29, CD44, and CD90. CD29- and CD44-positive cells showed a unimodal distribution, whereas CD90-positive cells exhibited a bimodal distribution. Approximately 84% of the cells analyzed were CD90 positive. Almost no cells expressed the negative markers CD31, CD34, and CD45. These results indicate that nearly all of the cells collected from mouse adipose tissue could be characterized as AdSCs expressing the specific surface markers of MSCs.
Maintenance of the undifferentiated state of AdSCs in the IP hydrogels
We investigated the gene expression levels of undifferentiated markers (OCT4, Nanog, and Sox2) [46,47,48] in AdSCs cultured in IP hydrogels with various tri-PCG-acryl contents by RT‒qPCR (Figs. 2a–c). The gene expression levels of the undifferentiated markers of cells cultured in the IP hydrogels were equal to or higher than those of AdSCs cultured on TCPS. Moreover, the gene expression level increased as the incubation time increased. Interestingly, the gene expression levels of the markers of undifferentiated AdSCs were higher after culture in the IP hydrogels than before culture.
Relative mRNA expression levels of (a) OCT4/GAPDH, (b) Nanog/GAPDH, (c) Sox2/GAPDH, (d) AFP/GAPDH, (e) Brachyury/GAPDH, and (f) Pax6/GAPDH in adipose-derived stem cells cultured in injectable polymer hydrogels or tissue culture polystyrene (TCPS) for 2, 4, or 7 d, as analyzed by RT‒qPCR. Data are expressed as the mean ± standard deviation (n = 3). *p < 0.05, as determined by the Tukey–Kramer test
We previously reported that the mechanical strength (storage modulus, G’) of IP hydrogels could be controlled from approximately 50–5000 Pa by changing the tri-PCG-acryl content [42]. The IP hydrogels used in this study exhibited storage moduli of 50–1000 Pa. However, no obvious trends in the relationship between tri-PCG-acryl content and the gene expression of the undifferentiated markers of AdSCs incubated in the IP hydrogels were observed. These results indicate that mechanical strength in this range (50–1000 Pa) has no significant influence on the differentiation potency of AdSCs. Thus, the AdSCs maintained their undifferentiated state even after culture in the IP hydrogels.
We investigated the gene expression levels of tridermic differentiation markers (AFP, Brachyury, and Pax6) [49,50,51] in AdSCs cultured in the IP hydrogels. The gene expression levels of AdSCs cultured in the IP hydrogels were equal to or higher than those of cells cultured on TCPS (Figs. 2d–f). Gene expression levels increased as the tri-PCG-acryl content increased, although this tendency was not obvious. In fact, most of the data were not significantly different, with small absolute values and large error bars, as determined by the Tukey–Kramer test. These results indicate that the types of genes that show increased expression in the AdSCs cultured in the hydrogels may differ depending on the properties of the hydrogel matrix, such as its elastic modulus. Overall, the increase in the gene expression levels of the undifferentiated cell markers was more apparent than that of the tridermic differentiation markers. The mechanism by which these undifferentiated cell markers increased in the IP hydrogel is currently unclear. Although some reports on the maintenance of the undifferentiated state are available [52,53,54], we did not find any report on the increase in undifferentiated cell markers attributable to the external environment. We presume that this phenomenon is due to the low elastic modulus and cell adhesion ability of the IP hydrogel, but we have not yet obtained concrete data to support this supposition. Based on the results, we concluded that the undifferentiated state of AdSCs was maintained in all IP hydrogels tested despite variations in tri-PCG-acryl content. Therefore, the IP formulation containing 16 wt% tri-PCG-acryl and an equivalent amount of DPMP were used in subsequent experiments.
Evaluation of multipotency
Next, we investigated whether the AdSCs cultured in the IP hydrogel maintained their ability to differentiate into osteoblasts. The differentiation ability of osteoblasts was investigated using an ALP assay and RT‒qPCR according to the following protocols: Protocol (1): Differentiation was performed during incubation in the IP hydrogel with osteogenic differentiation medium; Protocol (2): The cells were first incubated in the IP hydrogel with normal medium for AdSCs (ADSC-1) and then differentiated on TCPS with osteogenic differentiation medium.
Figure 3a shows the ALP activity of AdSCs cultured in the IP hydrogels with osteogenic differentiation medium or ADSC-1 (Protocol (1)). The viability of cells cultured in the IP hydrogel for 3 weeks was estimated to be approximately 20% by the live/dead assay. The viable cells collected from the IP hydrogel after culture did not show adhesion and spreading ability on TCPS for at least 1 week following their recovery from the IP hydrogel. The following data describe the results of AdSCs that survived after incubation. AdSCs cultured in the IP hydrogel with osteogenic differentiation medium showed nearly the same level of ALP activity as non-differentiation-induced AdSCs on Days 14 and 21. In addition, the gene expression of bone differentiation markers (ATF4, Osx, and Runx2) in AdSCs cultured in the IP hydrogel containing osteogenic differentiation medium was similar to or less than that of cells cultured in the IP hydrogel containing ADSC-1 (nondifferentiation) (Fig. 3b–d). These results suggest that AdSC differentiation does not proceed in the IP hydrogels because the cells are unable to adhere to the matrix and have low cell viability.
Evaluation of the osteogenic differentiation of adipose-derived stem cells. (a) ALP activity of adipose-derived stem cells cultured in injectable polymer hydrogels with (+) or without (−) osteoblast differentiation inductive factors for 14 or 21 d. (b)–(d) Relative mRNA expression levels of (b) ATF4/GAPDH, (c) Osx/GAPDH, and (d) Runx2/GAPDH in adipose-derived stem cells cultured with (+) or without (−) osteoblast differentiation inductive factors for 14 or 21 d (Protocol (1)), as analyzed by RT‒qPCR. (e) and (f) ALP activity of adipose-derived stem cells cultured with (+) or without (−) osteoblast differentiation inductive factors for 14 or 21 d on tissue culture polystyrene (TCPS) (e) with or (f) without preincubation in the IP hydrogel for 7 d. (g)–(i) Relative mRNA expression levels of (g) ATF4/GAPDH, (h) Osx/GAPDH, and (i) Runx2/GAPDH in adipose-derived stem cells cultured with (+) or without (−) osteoblast differentiation inductive factors for 14 or 21 d on TCPS after preincubation in the IP hydrogel for 7 d (Protocol (2)), as analyzed by RT‒qPCR. Data are expressed as the mean ± standard deviation (n = 3). *p < 0.05, **p < 0.01, as determined by the Tukey–Kramer test
We attempted to induce the differentiation of AdSCs into osteoblasts by reseeding on TCPS after culture under non-differentiation-inducing conditions in the IP hydrogel (Protocol (2)). The ALP activity of the cells normalized to the total amount of proteins was compared between AdSCs with (+) and without (−) differentiation induction factors (Fig. 3e–g). After preincubation in the IP hydrogel, ALP activity increased by only approximately 1.2 times (Fig. 3e). Without preincubation in the IP hydrogel, the ALP activity of AdSCs with differentiation induction factors increased by approximately 10 times relative to that of AdSCs incubated without differentiation induction factors for 21 d (Fig. 3(f)). Moreover, the gene expression of bone differentiation markers (ATF4, Osx, and Runx2) [55] in AdSCs cultured with differentiation induction factors (+) on TCPS after preincubation in the IP hydrogel (Protocol (2)) was not significantly different from that of AdSCs cultured without differentiation induction factors (−) (Fig. 3g–i). These results suggest that the bone differentiation ability of AdSCs is reduced by culture in IP hydrogels.
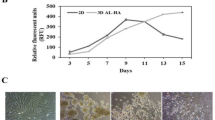
Next, we investigated the differentiation of AdSCs into adipocytes. Stem cells have been reported to differentiate into adipocytes, rather than osteoblasts, when cultured on a matrix with a low elastic modulus [56]. After the AdSCs were cultured in the IP hydrogel for 7 d under non-differentiation-inducing conditions, we investigated the adipocyte differentiation of AdSCs cultured under various adipocytic differentiation conditions on TCPS for 14 or 21 d. The Oil red O (ORO) staining results of AdSCs cultured with (+) or without (−) adipocyte differentiation factors on TCPS as a control experiment are shown in Fig. 4a. The absorbance of the dye extracted from the stained cells is shown in Fig. 4b. AdSCs cultured with (+) adipocyte differentiation factors were redder than AdSCs without (−) adipocyte differentiation factors, suggesting the successful adipocyte differentiation of the cells. The results of cell cultures preincubated in the IP hydrogel for 7 d are shown in Fig. 4c,d. An increase in the number of ORO-stained cells was not observed under the various adipocytic differentiation conditions (Fig. 4c). The absorbance of AdSCs cultured with (+) adipocyte differentiation factors was lower than or similar to that of cells without (−) differentiation factors (Fig. 4d), although the absorbance should be normalized by the number of viable cells. These results suggest that AdSCs cultured in IP hydrogels have a reduced ability to differentiate into adipocytes.
Evaluation of adipocyte differentiation of adipose-derived stem cells. (a) Microscopic (×10) (upper) and whole (bottom) images of the wells of adipose-derived stem cells (AdSCs) cultured with (+) or without (−) adipocyte differentiation medium on tissue culture polystyrene (TCPS) for 14 or 21 d. (b) Absorbance of the culture medium with extracted pigments of AdSCs cultured with (+) or without (−) adipocyte differentiation medium on TCPS for 14 or 21 d. (c) Microscopic (×10) (upper) and whole images (bottom) of the wells of AdSCs cultured first in the IP hydrogel for 7 d and then on TCPS with (+) or without (–) adipocyte differentiation medium for 14 or 21 d. (d) Absorbance of the culture medium with extracted pigments of AdSCs cultured first in the IP hydrogel for 7 d and then in TCPS with (+) or without (−) adipocyte differentiation medium for 14 or 21 d. The cells were stained with ORO. (e)–(g) Relative mRNA expression levels of (e) APN/GAPDH, (f) LPL/GAPDH, and (g) PPARγ2/GAPDH in adipose-derived stem cells cultured with (+) or without (−) adipose differentiation inductive factors for 14 or 21 d on TCPS with or without preincubation in the IP hydrogel for 7 d, as analyzed by RT‒qPCR. Data in (b) and (d)–(g) are expressed as the mean ± standard deviation (n = 3). *p < 0.05, **p < 0.01, ***p < 0.001, as determined by the Tukey–Kramer test
Figure 4e, f show the gene expression levels of adipose differentiation markers (APN, LPL, and PPARγ2) [56]. When differentiation on TCPS without preincubation in the IP hydrogel (control experiment) was conducted, the gene expression level of all adipose differentiation markers obviously increased. In contrast, the increase in the gene expression of adipose differentiation markers under differentiation conditions was almost nonexistent or minimal after preincubation in the IP hydrogel. These results suggest that the ability of AdSCs to differentiate into adipocytes is strongly reduced after culture in the IP hydrogel.
In previous reports [57,58,59], stem cells were cultured in hydrogels with elastic moduli of approximately 1000–10,000 Pa with or without cell adhesive ligands. The elastic modulus of the IP hydrogel in the present experiment was approximately 50–1000 Pa, which is lower than that in previous reports. We presumed that the low elastic modulus and weakly adhesive nature of the IP hydrogel prevented the adhesion and spreading of AdSCs. These characteristics may be key factors influencing the observed decrease in the differentiation ability of the AdSCs. Future experiments employing careful control of the elastic modulus of the IP hydrogel and the introduction of cell-adhesive ligands into the IP hydrogel will provide more information.
In summary, we prepared a temperature-responsive IP hydrogel that partially forms covalent cross-links using a thiol-ene reaction and investigated the maintenance of the undifferentiated state and multipotency of AdSCs cultured on this gel. The AdSCs maintained an undifferentiated state in the IP hydrogel. However, contrary to expectations, we found that their multipotency, that is, their ability to differentiate into multiple cells, such as osteoblasts and adipocytes, decreased, likely because of the extreme softness of the IP hydrogel and its poor cell adhesive property. This phenomenon may be transient, and the differentiation ability of the cells may be regained if they are cultured on TCPS or other stiff cell culture matrices for an extended period of time. These results highlight the need to assess the properties of IP hydrogel systems with low mechanical strength for use in stem cell delivery and tissue engineering. The mechanical properties of the hydrogel scaffold and its capability for cell adhesion must be considered when attempting to induce differentiation into specific cells using such IP systems. Moreover, although the chemical structure of the hydrogel may also exert some effects on the maintenance of the undifferentiated state and multipotency of AdSCs, this consideration was not investigated in the present study and may be examined in future work. The cytokine secretion ability of AdSCs is related to their undifferentiated state. We previously confirmed that AdSCs cultured in the same IP hydrogel secrete various cytokines, including vascular endothelial growth factor [43]. Thus, maintaining these cells in an undifferentiated state for as long as possible in the IP hydrogel may be desirable during stem cell delivery to encourage the secretion of various therapeutic cytokines. Taken together, our results collectively indicate that IP systems containing AdSCs can potentially be applied to various biomedical fields, such as cellular therapeutics for myocardial infarction.
References
Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, et al. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282:1145–7. https://doi.org/10.1126/science.282.5391.1145
Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–76. https://doi.org/10.1016/j.cell.2006.07.024
Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ, et al. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001;7:211–28. https://doi.org/10.1089/107632701300062859
Zuk PA, Zhu M, Ashjian P, De Ugarte DA, Huang JI, Mizuno H, et al. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell 2002;13:4279–95. https://doi.org/10.1091/mbc.e02-02-0105
Safford KM, Hicok KC, Safford SD, Halvorsen YDC, Wilkison WO, Gimble JM, et al. Neurogenic differentiation of murine and human adipose-derived stromal cells. Biochem Biophys Res Commun 2002;294:371–9. https://doi.org/10.1016/s0006-291x(02)00469-2
Miranville A, Heeschen C, Sengenès C, Curat CA, Busse R, Bouloumié A. Improvement of postnatal neovascularization by human adipose tissue-derived stem cells. Circulation. 2004;110:349–55. https://doi.org/10.1161/01.cir.0000135466.16823.d0
Planat-Benard V, Silvestre J-S, Cousin B, André M, Nibbelink M, Tamarat R, et al. Plasticity of human adipose lineage cells toward endothelial cells: physiological and therapeutic perspectives. Circulation. 2004;109:656–63. https://doi.org/10.1161/01.cir.0000114522.38265.61
Kilroy GE, Foster SJ, Wu X, Ruiz J, Sherwood S, Heifetz A, et al. Cytokine profile of human adipose-derived stem cells: expression of angiogenic, hematopoietic, and pro-inflammatory factors. J Cell Physiol 2007;212:702–9. https://doi.org/10.1002/jcp.21068
Gonzalez-Rey E, Anderson P, González MA, Rico L, Büscher D, Delgado M. Human adult stem cells derived from adipose tissue protect against experimental colitis and sepsis. Gut. 2009;58:929–39. https://doi.org/10.1136/gut.2008.168534
Gonzalez-Rey E, Gonzalez MA, Varela N, O’Valle F, Hernandez-Cortes P, Rico L, et al. Human adipose-derived mesenchymal stem cells reduce inflammatory and T cell responses and induce regulatory T cells in vitro in rheumatoid arthritis. Ann Rheum Dis 2010;69:241–8. https://doi.org/10.1136/ard.2008.101881
Kim MH, Hong HN, Hong JP, Park CJ, Kwon SW, Kim SH, et al. The effect of VEGF on the myogenic differentiation of adipose tissue derived stem cells within thermosensitive hydrogel matrices. Biomaterials. 2010;31:1213–8. https://doi.org/10.1016/j.biomaterials.2009.10.057
Yu H, Lu K, Zhu JY, Wang JA. Stem cell therapy for ischemic heart diseases. Br Med Bull. 2017;121:135–54. https://doi.org/10.1093/bmb/ldw059
Nagata H, Ii M, Kohbayashi E, Hoshiga M, Hanafusa T, Asahi M. Cardiac adipose-derived stem cells exhibit high differentiation potential to cardiovascular cells in C57BL/6 mice. Stem Cells Transl Med. 2016;5:141–51. https://doi.org/10.5966/sctm.2015-0083
Yang D, Wang W, Li L, Peng Y, Chen P, Huang H, et al. The relative contribution of paracrine effect versus direct differentiation on adipose-derived stem cell transplantation mediated cardiac repair. PLoS One. 2013;8:e59020 https://doi.org/10.1371/journal.pone.0059020
Gautam M, Fujita D, Kimura K, Ichikawa H, Izawa A, Hirose M, et al. Transplantation of adipose tissue-derived stem cells improves cardiac contractile function and electrical stability in a rat myocardial infarction model. J Mol Cell Cardiol 2015;81:139–49. https://doi.org/10.1016/j.yjmcc.2015.02.012
Bai X, Yan Y, Song Y-H, Seidensticker M, Rabinovich B, Metzele R, et al. Both cultured and freshly isolated adipose tissue-derived stem cells enhance cardiac function after acute myocardial infarction. Eur Heart J 2010;31:489–501. https://doi.org/10.1093/eurheartj/ehp568
Qazi TH, Mooney DJ, Duda GN, Geissler S. Biomaterials that promote cell-cell interactions enhance the paracrine function of MSCs. Biomaterials. 2017;140:103–14. https://doi.org/10.1016/j.biomaterials.2017.06.019
Burdick JA, Mauck RL, Gerecht S. To serve and protect: hydrogels to improve stem cell-based therapies. Cell Stem Cell. 2016;18:13–5. https://doi.org/10.1016/j.stem.2015.12.004
Yu L, Ding J. Injectable hydrogels as unique biomedical materials. Chem Soc Rev 2008;37:1473–81. https://doi.org/10.1039/b713009k
Yang JA, Yeom J, Hwang BW, Hoffman AS, Hahn SK. In situ-forming injectable hydrogels for regenerative medicine. Prog Polym Sci 2014;39:1973–86. https://doi.org/10.1016/j.progpolymsci.2014.07.006
Moon HJ, Ko DY, Park MH, Joo MK, Jeong B. Temperature-responsive compounds as in situ gelling biomedical materials. Chem Soc Rev 2012;41:4860–83. https://doi.org/10.1039/c2cs35078e
Nagahama K, Takahashi A, Ohya Y. Biodegradable polymers exhibiting temperature-responsive sol-gel transition as injectable biomedical materials. React Funct Polym 2013;73:979–85. https://doi.org/10.1016/j.reactfunctpolym.2012.11.003
Li Y, Rodrigues J, Tomás H. Injectable and biodegradable hydrogels: gelation, biodegradation and biomedical applications. Chem Soc Rev 2012;41:2193–221. https://doi.org/10.1039/c1cs15203c
Nguyen MK, Lee DS. Injectable biodegradable hydrogels. Macromol Biosci 2010;10:563–79. https://doi.org/10.1002/mabi.200900402
Mathew AP, Uthaman S, Cho KH, Cho CS, Park IK. Injectable hydrogels for delivering biotherapeutic molecules. Int J Biol Macromol 2018;110:17–29. https://doi.org/10.1016/j.ijbiomac.2017.11.113
Choi S, Baudys M, Kim SW. Control of blood glucose by novel GLP-1 delivery using biodegradable triblock copolymer of PLGA-PEG-PLGA in type 2 diabetic rats. Pharm Res 2004;21:827–31. https://doi.org/10.1023/b:pham.0000026435.27086.94
Manokruang K, Lee DS. Albumin-conjugated pH/thermo responsive poly(amino urethane) multiblock copolymer as an injectable hydrogel for protein delivery. Macromol Biosci 2013;13:1195–1203. https://doi.org/10.1002/mabi.201300236
Zhang Z, Ni J, Chen L, Yu L, Xu J, Ding D. Biodegradable and thermoreversible PCLA-PEG-PCLA hydrogel as a barrier for prevention of post-operative adhesion. Biomaterials. 2011;32:4725–36. https://doi.org/10.1016/j.biomaterials.2011.03.046
Yu L, Hu H, Chen L, Bao X, Li Y, Chen L, et al. Comparative studies of thermogels in preventing post-operative adhesions and corresponding mechanisms. Biomater Sci 2014;2:1100–9. https://doi.org/10.1039/C4BM00029C
Chen X, Huang L, Sun H-J, Cheng SZD, Zhu M, Yang G. Stimuli-responsive nanocomposite: potential injectable embolization agent. Macromol Rapid Commun 2014;35:579–84. https://doi.org/10.1002/marc.201300720
Weng L, Rostambeigi N, Zantek ND, Rostamzadeh P, Bravo M, Carey J, et al. An in situ forming biodegradable hydrogel-based embolic agent for interventional therapies. Acta Biomater. 2013;9:8182–92. https://doi.org/10.1016/j.actbio.2013.06.020
Yu L, Xu W, Shen W, Cao L, Liu Y, Li Z, et al. Poly(lactic acid-co-glycolic acid)-poly(ethylene glycol)-poly(lactic acid-co-glycolic acid) thermogel as a novel submucosal cushion for endoscopic submucosal dissection. Acta Biomater. 2014;10:1251–8. https://doi.org/10.1016/j.actbio.2013.12.007
Yeon B, Park MH, Moon HJ, Kim S-J, Cheon YW, Jeong B. 3D culture of adipose-tissue-derived stem cells mainly leads to chondrogenesis in poly(ethylene glycol)-poly(L-alanine) diblock copolymer thermogel. Biomacromolecules. 2013;14:3256–66. https://doi.org/10.1021/bm400868j
Oyama N, Minami H, Kawano D, Miyazaki M, Maeda T, Toma K, et al. A nanocomposite approach to develop biodegradable thermogels exhibiting excellent cell-compatibility for injectable cell delivery. Biomater Sci 2014;2:1057–62. https://doi.org/10.1039/C4BM00074A
Metters A, Hubbell J. Network formation and degradation behavior of hydrogels formed by Michael-type addition reactions. Biomacromolecules. 2005;6:290–301. https://doi.org/10.1021/bm049607o
Pratt AB, Weber FE, Schmoekel HG, Müller R, Hubbell JA. Synthetic extracellular matrices for in situ tissue engineering. Biotechnol Bioeng 2004;86:27–36. https://doi.org/10.1002/bit.10897
Kurakazu M, Katashima T, Chijiishi M, Nishi K, Akagi Y, Matsunaga T, et al. Evaluation of gelation kinetics of tetra-PEG gel. Macromolecules. 2010;43:3935–40. https://doi.org/10.1021/ma100176f
Johnson JA, Finn MG, Koberstein JT, Turro NJ. Construction of linear polymers, dendrimers, networks, and other polymeric architectures by copper-catalyzed azide-alkyne cycloaddition “click” chemistry. Macromol Rapid Commun 2008;29:1052–72. https://doi.org/10.1002/marc.200800208
Zheng J, Callahan LAS, Hao J, Guo K, Wesdemiotis C, Weiss RA, et al. Strain-promoted cross-linking of PEG-based hydrogels via copper-free cycloaddition. ACS Macro Lett. 2012;1:1071–3. https://doi.org/10.1021/mz3003775
Yoshida Y, Takahashi A, Kuzuya A, Ohya Y. Instant preparation of a biodegradable injectable polymer formulation exhibiting a temperature-responsive sol-gel transition. Polym J 2014;46:632–5. https://doi.org/10.1038/pj.2014.30
Yoshida Y, Kawahara K, Inamoto K, Mitsumune S, Ichikawa S, Suzuya A, et al. Biodegradable injectable polymer systems exhibiting temperature-responsive irreversible sol-to-gel transition by covalent bond formation. ACS Biomater Sci Eng 2017;3:56–67. https://doi.org/10.1021/acsbiomaterials.6b00581
Yoshida Y, Takai H, Kawahara K, Mitsumune S, Takata K, Kuzuya A, et al. Biodegradable injectable polymer systems exhibiting a longer and controllable duration time of the gel state. Biomater Sci 2017;5:1304–14. https://doi.org/10.1039/C7BM00357A
Yoshizaki Y, Ii M, Takai H, Mayumi N, Fujiwara S, Kuzuya A, et al. Cellular therapy for myocardial ischemia using a temperature-responsive biodegradable injectable polymer system with adipose-derived stem cells. Sci Technol Adv Mater 2021;22:627–42. https://doi.org/10.1080/14686996.2021.1938212
Engler AJ, Sen S, Sweeney HL, Discher DE. Matrix elasticity directs stem cell lineage specification. Cell. 2006;126:677–89. https://doi.org/10.1016/j.cell.2006.06.044
Smith LR, Cho S, Discher DE. Stem cell differentiation is regulated by extracellular matrix mechanics. Physiol (Bethesda). 2018;33:16–25. https://doi.org/10.1152/physiol.00026.2017
Nichols J, Zevnik B, Anastassiadis K, Niwa H, Klewe-Nebenius D, Chambers I, et al. Formation of pluripotent stem cells in the mammalian embryo depends on the POU transcription factor Oct4. Cell. 1998;95:379–91. https://doi.org/10.1016/s0092-8674(00)81769-9
Chambers I, Colby D, Robertson M, Nichols J, Lee S, Tweedie S, et al. Functional expression cloning of Nanog, a pluripotency sustaining factor in embryonic stem cells. Cell. 2003;113:643–55. https://doi.org/10.1016/s0092-8674(03)00392-1
Avilion AA, Nicolis SK, Pevny LH, Perez L, Vivian N, Lovell-Badge R. Multipotent cell lineages in early mouse development depend on SOX2 function. Genes Dev. 2003;17:126–40. https://doi.org/10.1101/gad.224503
Abe K, Niwa H, Iwase K, Takiguchi M, Mori M, Abé SI, et al. Endoderm-specific gene expression in embryonic stem cells differentiated to embryoid bodies. Exp Cell Res 1996;229:27–34. https://doi.org/10.1006/excr.1996.0340
Kispert A, Herrmann BG. The Brachyury gene encodes a novel DNA binding protein. EMBO J. 1993;12:3211–20. 10.1002%2Fj.1460-2075.1993.tb05990.x
Walther C, Gruss P. Pax-6, a murine paired box gene, is expressed in the developing CNS. Development. 1991;113:1435–49. https://doi.org/10.1242/dev.113.4.1435
Kuhn NZ, Tuan RS. Regulation of stemness and stem cell niche of mesenchymal stem cells: Implications in tumorigenesis and metastasis. J Cell Physiol 2010;222:268–77. https://doi.org/10.1002/jcp.21940
Gerecht S, Burdick JA, Ferreira LS, Townsend SA, Langer R, Vunjak-Novakovic G. Hyaluronic acid hydrogel for controlled self-renewal and differentiation of human embryonic stem cells. Proc Natl Acad Sci Usa 2007;104:11298–303. https://doi.org/10.1073/pnas.0703723104
Dawson E, Mapili G, Erickson K, Taqvi S, Roy K. Biomaterials for stem cell differentiation. Adv Drug Deliv Rev 2008;60:215–28. https://doi.org/10.1016/j.addr.2007.08.037
Liu TM, Lee EH. Transcriptional regulatory cascades in Runx2-dependent bone development. Tissue Eng B 2013;19:254–63. https://doi.org/10.1089/ten.teb.2012.0527
Fu Y, Li R, Zhong J, Fu N, Wei X, Cun X, et al. Adipogenic differentiation potential of adipose-derived mesenchymal stem cells from ovariectomized mice. Cell Prolif. 2014;47:604–14. https://doi.org/10.1111/cpr.12131
Sinclair A, O’Kelly MB, Bai T, Hung H-C, Jain P, Jiang S. Self-healing zwitterionic microgels as a versatile platform for malleable cell constructs and injectable therapies. Adv Mater 2018;30:1803087 https://doi.org/10.1002/adma.201803087
Dong Y, Sigen A, Rodrigues M, Li X, Kwon SH, Kosaric N, et al. Injectable and tunable gelatin hydrogels enhance stem cell retention and improve cutaneous wound healing. Adv Funct Mater 2017;27:1606619 https://doi.org/10.1002/adfm.201606619
Zhang KY, Feng Q, Xu J, Xu X, Tian F, Yeung KWK, et al. Self-assembled injectable nanocomposite hydrogels stabilized by bisphosphonate-magnesium (Mg2+) coordination regulates the differentiation of encapsulated stem cells via dual crosslinking. Adv Funct Mater 2017;27:1701642 https://doi.org/10.1002/adfm.201701642
Acknowledgements
This work was financially supported in part by the Private University Research Branding Project with matching fund subsidies from the Ministry of Education, Culture, Sports, Science, and Technology (MEXT) Japan (2016–2020) and Grants-in-Aid for Scientific Research (16H01854 and 20H00670) from the Japan Society for the Promotion of Science (JSPS). The authors also thank SC Organic Chemical Co., Ltd., for providing DPMP.
Author information
Authors and Affiliations
Contributions
NMa designed and performed the experiments and wrote the manuscript draft. NMu analyzed the data and wrote the paper. YY designed and performed the experiments and analyzed the data. AK analyzed the data. YO supervised the experiments and wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mayumi, N., Murase, N., Yoshizaki, Y. et al. Loss of multipotency in adipose-derived stem cells after culture in temperature-responsive injectable polymer hydrogels. Polym J 55, 261–271 (2023). https://doi.org/10.1038/s41428-022-00739-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41428-022-00739-4