Abstract
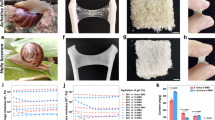
We developed a novel spray-type dextrin hydrogel-based adhesion barrier designed to create a site-specific barrier on a target. Our novel hydrogel is composed of Powder A, which mainly contains N-hydroxysuccinimide-modified carboxymethyl dextrin and trehalose as a stabilizing agent, and Powder B, which is composed of sodium carbonate and sodium hydrogen carbonate. Here, we describe the product specifications of the hydrogel and results of in vivo performance evaluations and clinical studies to demonstrate its efficacy and safety.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Pillai CKS, Sharma CP. Review paper: absorbable polymeric surgical sutures: chemistry, production, properties, biodegradability, and performance. J Biomater Appl. 2010;25:29–366.
Kim M, Oommen B, Ross SW, Lincourt AE, Matthews BD, Heniford BT, et al. The current status of biosynthetic mesh for ventral hernia repair. Surg Technol Int. 2014;25:114–21.
Spotnitz WD, Burks S. Hemostats, sealants, and adhesives: components of the surgical toolbox. Transfusion. 2008;48:1502–16.
Ohya Y. Temperature-responsive biodegradable injectable polymer systems with conveniently controllable properties. Polym J. 2019;51:997–1005.
Uyama H. Functional polymers from renewable plant oils. Polym J. 2018;50:1003–11.
DeWilde RL, Trew G, on behalf of the Expert Adhesions Working Party of the European Society of Gynaecological Endoscopy (ESGE. Postoperative abdominal adhesions and their prevention in gynaecological surgery. Expert consensus position. Gynecol Surg. 2007;4:161–8.
Ellis H, Moran BJ, Thompson JN, Parker MC, Wilson MS, Menzies D, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1999;353:1476–80.
Lower AM, Hawthorn RJ, Clark D, Boyd JH, Finlayson AR, Knight AD, Crowe AM, on behalf of the Surgical and Clinical Research (SCAR) Group. Adhesion-related readmissions following gynaecological laparoscopy or laparotomy in Scotland: an epidemiological study of 24,046 patients. Hum Reprod. 2004;19:1877–85.
Lower AM, Hawthorn RJ, Ellis H, O’Brien F, Buchan S, Crowe AM. The impact of adhesions on hospital readmissions over ten years after 8849 open gynaecological operations: an assessment from the Surgical and Clinical Adhesions Research Study. Br J Obstet Gynaecol. 2000;107:855–62.
DeWilde TG, on behalf of the Expert Adhesions Working Party of the European Society of Gynaecological Endoscopy (ESGE. Postoperative abdominal adhesions and their prevention in gynaecological surgery. Expert consensus position. Part 2—steps to reduce adhesions. Gynecol Surg. 2007;4:243–53.
diZerega GS. Contemporary adhesion prevention. Fertil Steril. 1994;61:219–35.
Rodgers KE, diZerega GS. Developing pharmacologic agents for adhesion prevention. In: diZerega GS, editor. Peritoneal surgery. New York: Springer-Verlag; 2000. p. 441–57.
Ahmad G, Mackie FL, Iles DA, O'Flynn H, Dias S, Metwally M, et al. Fluid and pharmacological agents for adhesion prevention after gynaecological surgery. Cochrane Database Syst Rev. 2014;9:CD001298.
El-Mowafi DM, Diamond MP. Are pelvic adhesions preventable? Surg Technol Int. 2003;11:222–35.
Risberg B. Adhesions: preventive strategies. Eur J Surg. 1997;577:32–9.
Awonuga AO, Saed GM, Diamond MO. Laparoscopy in gynecologic surgery: adhesion development, prevention, and use of adjunctive therapies. Clin Obstet Gynecol. 2009;52:412–22.
Fazio VW, Cohen Z, Fleshman JW, van Goor H, Bauer JJ, Wolff BG, et al. Reduction in adhesive small bowel obstruction by Seprafilm adhesion barrier after intestinal resection. Dis Colon Rectum. 2006;49:1–11.
Ten Broek RPG, Stommel MWJ, Strik C, van Laarhoven CJHM, Keus F, van Goor H. Benefits and harms of adhesion barriers for abdominal surgery: a systematic review and meta-analysis. Lancet. 2014;383:48–59.
Trew G, Pistofidis G, Pados G, Lower A, Mettler L, Wallwiener D, et al. Gynaecological endoscopic evaluation of 4% icodextrin solution: a European, multicentre, double-blind, randomized study of the efficacy and safety in the reduction of de novo adhesions after laparoscopic gynaecological surgery. Hum Reprod. 2011;26:2015–27.
Keller B, Yawalkar N, Pichler C, Braathen LR, Hunger RE. Hypersensitivity reaction against patent blue during sentinel lymph node removal in three melanoma patients. Am J Surg. 2007;193:122–4.
Takeuchi H, Kitade M, Kikuchi I, Shimanuki H, Kinoshita K. A novel instrument and technique for using Seprafilm hyaluronic acid/carboxymethylcellulose membrane during laparoscopic myomectomy. J Laparoendosc Adv Surg Tech A. 2006;16:497–502.
Chuang YC, Lu HF, Peng FS, Ting WH, Tu FC, Chen MJ, et al. Modified novel technique for improving the success rate of applying seprafilm by using laparoscopy. J Minim Invasive Gynecol. 2014;21:787–90.
Kusuki I, Suganuma I, Ito F, Akiyama M, Sasaki A, Yamanaka K, et al. Usefulness of moistening seprafilm before use in laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2014;24:e13–5.
Verco SJ, Peers EM, Brown CB, Rodgers KE, Roda N, diZerega G. Development of a novel glucose polymer solution (icodextrin) for adhesion prevention: pre-clinical studies. Hum Reprod. 2000;15:1764–72.
Brown CB, Luciano AA, Martin D, Peers E, Scrimgeour A, diZerega GS, Adept Adhesion Reduction Study Group. Adept (icodextrin 4% solution) reduces adhesions after laparoscopic surgery for adhesiolysis: a double blind, randomized, controlled study. Fertil Steril. 2007;88:1413–26.
Kai M, Maeda K, Tasaki M, Kira S, Nakamura S, Chino N, et al. Evaluation of a spray-type, novel dextrin hydrogel adhesion barrier under laparoscopic conditions in a porcine uterine horn adhesion model. J Minim Invasive Gynecol. 2017;25:447–54.
Cezar C, Korell M, Tchartchian G, Ziegler N, Senshu K, Herrmann A, et al. How to avoid risks for patients in minimal-access trials: avoiding complications in clinical first-in-human studies by example of the ADBEE study. Best Pract Res Clin Obstet Gynaecol. 2016;35:84–96.
Cezar C, Tchartchian G, Korell M, Ziegler N, Senshu K, De Wilde MS, et al. Long term follow-up concerning safety and efficacy of novel adhesion prophylactic agent for laparoscopic myomectomy in the prospective randomized ADBEE study. Best Pract Res Clin Obstet Gynaecol. 2016;35:97–112.
Suto T, Watanabe M, Endo T, Komori K, Ohue M, Kanemitsu Y, et al. The primary result of prospective randomized multicenter trial of new spray-type bio-absorbable adhesion barrier system (TCD-11091) against postoperative adhesion formation. J Gastrointest Surg. 2017;21:1683–91.
Acknowledgements
The authors would like to express their sincere gratitude to all those who collaborated and supported this research and for “The Award of the Society of Polymer Science, Japan (Technology) 2017” awarded by the Society of Polymer Science, Japan, for this study, “Development of a spray-type adhesion barrier”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chino, N., Ishihara, H., Niimi, T. et al. Development of a spray-type adhesion barrier. Polym J 52, 473–479 (2020). https://doi.org/10.1038/s41428-020-0306-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41428-020-0306-0