Abstract
Longitudinal characterization of SARS-CoV-2 PCR testing from COVID-19 patient’s nasopharynx and its juxtaposition with blood-based IgG-seroconversion diagnostic assays is critical to understanding SARS-CoV-2 infection durations. Here, we retrospectively analyze 851 SARS-CoV-2-positive patients with at least two positive PCR tests and find that 99 of these patients remain SARS-CoV-2-positive after 4 weeks from their initial diagnosis date. For the 851-patient cohort, the mean lower bound of viral RNA shedding was 17.3 days (SD: 7.8), and the mean upper bound of viral RNA shedding from 668 patients transitioning to confirmed PCR-negative status was 22.7 days (SD: 11.8). Among 104 patients with an IgG test result, 90 patients were seropositive to date, with mean upper bound of time to seropositivity from initial diagnosis being 37.8 days (95% CI: 34.3–41.3). Our findings from juxtaposing IgG and PCR tests thus reveal that some SARS-CoV-2-positive patients are non-hospitalized and seropositive, yet actively shed viral RNA (14 of 90 patients). This study emphasizes the need for monitoring viral loads and neutralizing antibody titers in long-term non-hospitalized shedders as a means of characterizing the SARS-CoV-2 infection lifecycle.
Similar content being viewed by others
Introduction
As COVID-19 continues to rage globally with over 11 million confirmed infected individuals and 500,000 deaths1, the world is grappling with the dual challenge of stemming the tide of the current pandemic and planning for reopening the economy in the post-COVID-19 phase. Currently, there are over a million patients that have recovered from COVID-191, and some governments have suggested that antibody-based tests in recovered individuals can be used as the basis for an “immunity passport”2 to travel or return-to-work assuming that they are protected against reinfection and likely not infectious. However, there are also emerging reports of viral shedding for many days post-recovery, as evidenced from PCR tests on stool samples3 and recurrent SARS-CoV-2-positive PCR tests in “cured” patients4.
In addition to routine RT-PCR assays that are being used for COVID-19 clinical diagnosis, recent studies have suggested droplet digital PCR (ddPCR) as a more sensitive assay for quantifying viral load in early stages of infection5,6. The crossing point (Cp) values from SARS-CoV-2 RT-PCR assays has also been correlated with culture positivity to suggest that Cp values above 33–34 may no longer be associated with replication-competent virus7.
The general lack of understanding of the period of infectivity, viral shedding, and potential for transmission necessitates longitudinal monitoring of viral clearance in COVID-19 patients. Such an analysis has the potential to help inform the immunological basis for rapid viral control and disease progression.
Results
Between February and June 2020, 131,646 individuals underwent routine SARS-CoV-2 PCR testing at the Mayo Clinic hospitals in Minnesota, Arizona, and Florida, and the associated Mayo Clinic Health System (Fig. 1a). Of these, 27,309 individuals (21%) were subjected to the PCR test more than once (Fig. 1a). Of all the individuals tested, 5699 patients tested SARS-CoV-2-positive at least once during the study period (Fig. 1b). The age distributions in the context of hospitalization, intensive care unit (ICU) admission, and mortality status are shown for SARS-CoV-2-positive patients in Fig. 1c–f. Notably, over 50% of the SARS-CoV-2-positive patients in this study are in the age group of 0–40. The pattern of increased hospitalization, ICU admissions, and death in the elderly compared to the younger populations is consistent with previous studies of COVID-19 patient demographics8,9,10.
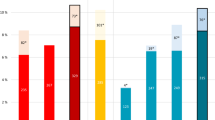
Distributions of a number of PCR tests per individual, b number of PCR tests taken by SARS-CoV-2-positive patients, c age of SARS-CoV-2-positive patients, d age of hospitalized SARS-CoV-2-positive patients, e age of ICU-admitted SARS-CoV-2-positive patients, f age of deceased SARS-CoV-2-positive patients, g the number of patients by sequence of SARS-COV-2 PCR positive and negative results, and h the number of switches between SARS-CoV-2-positive and SARS-CoV-2-positive status in longitudinal testing of SARS-CoV-2-positive patients; box indicates the count of patients that switched from SARS-CoV-2-positive to SARS-CoV-2-positive and back to SARS-CoV-2-positive status at least once.
Among the 5699 COVIDpos patients, 2126 patients (37.3%) were subjected to two or more PCR tests, and 851 patients (14.9%) had at least two SARS-CoV-2-positive PCR tests (Fig. 1b, g). We observed 203 patients oscillated from SARS-CoV-2-positive to SARS-CoV-2-negative and back to SARS-CoV-2-positive status one or more times (Fig. 1h). We henceforth consider a pair of contiguous SARS-CoV-2-negative PCR tests after the last positive PCR test to be indicative of a ‘confirmed COVID-19 negative’ status.
Despite the caveat of routine RT-PCR assays not providing data on the replication competency of the virus, the availability of these longitudinal PCR test results and the patients’ Electronic Health Records (EHRs), provides an excellent opportunity to quantify the duration of SARS-CoV-2-positive PCR results. Specifically, we aimed to quantify for each patient – (1) a lower bound of infection duration, defined as the time in days between the first and last positive SARS-CoV-2 PCR tests, and (2) an upper bound of infection duration, defined as the time in days between the first positive PCR test and the second negative PCR test after which there are no further positive PCR tests (Fig. 2a). The lower bound captures the most intuitive estimate of infection duration, at least from the standpoint of SARS-CoV-2 PCR positivity. Nevertheless, our quantification of the upper bound is motivated by recent reports of high false-negative rates for SARS-CoV-2 PCR tests11, our own observation of oscillations in serial PCR testing outcomes (Fig. 1h), and the requirement for healthcare workers to observe negative PCR results on 2 consecutive days to meet the CDC “Return to Work” criteria8.
SARS-CoV-2-positive patients whose lower bound of infection duration is >4 weeks (28 days) are hereafter referred to as patients with “long-term shedding of viral RNA”. For the 668 SARS-CoV-2-positive patients that switched to a confirmed negative status, i.e., two negative SARS-CoV-2 PCR tests following the last positive SARS-CoV-2 test, the distribution of the upper bound of infection duration was a mean of 22.8 days and a standard deviation of 11.8 days (Fig. 2b). Of the 851 SARS-CoV-2-positive patients with at least two PCR positive results, interestingly, 231 patients (27%) and 99 patients (11.6%) have viral RNA shedding beyond 21 days and 28 days of initial diagnosis, respectively (Fig. 2c). In both cases the majority of these patients are not hospitalized; i.e. 158 of 231 patients (68.4%, in the 21+ days category) and 61 of 99 patients (61.6%, in the 28+ days category).
Of 104 SARS-CoV-2-positive patients with available SARS-CoV-2 IgG serology data, 14 patients remain either serology negative or indeterminate till date. Of the remnant 90 patients who are seropositive till date, the upper bound of time to IgG-seropositivity from initial PCR diagnostic testing has a mean of 37.8 days (95% confidence interval: 34.3–41.3 days; Fig. 3a). Here, we consider this analysis as an “upper bound”, rather than a definitive time to seropositivity, as each patient may have experienced IgG seroconversion prior to the date when the serology test was actually administered. Based on the limited longitudinal real-world data available for IgG seropositivity, this upper bound is the best estimate we are able to obtain at this juncture.
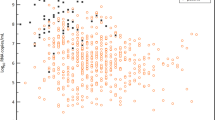
a Histogram of duration (in days) between the day of diagnosis based on SARS-CoV-2 PCR test and day of seropositive status based on SARS-CoV-2 IgG test. b Comparison of seropositive status (based on antibody test) and SARS-CoV-2-positive status (based on PCR test). Cases that are both IgG-seropositive and PCR positive are boxed. c Scatter plot of lower bound of viral RNA shedding (x-axis) versus the upper bound of IgG-seropositivity status (y-axis).
Next, we juxtaposed the SARS-CoV-2 PCR results against the IgG-seropositivity results for 90 SARS-CoV-2-positive patients with both sets of longitudinal data (Fig. 3b). Surprisingly, 14 of these patients had viral RNA shedding between 0 and 64 days after their confirmed date of IgG-seropositivity (Fig. 3c). The finding that the time to IgG seropositivity can be shorter than the lower bound of positive PCR tests in some patients, suggests that SARS-CoV-2-positive patients can continue to shed viral RNA for days or even weeks while generating IgG antibodies.
Long-term SARS-CoV-2-positive PCR tests are not necessarily indicative of long-term replication-competent virus12,13. Consequently, we evaluated 488 SARS-CoV-2-positive PCR tests’ Cp values from nasopharyngeal swab samples of 208 patients. Among these, the mean Cp value was 28.6 with a standard deviation of 5 (Fig. 4a). From 63 patients with viral RNA shedding beyond 21 days of initial diagnosis, the distribution of Cp values showed a mean of 31.87 and standard deviation of 1.14 (Fig. 4b). In a subset of 17 patients who demonstrated longer-term viral RNA shedding beyond 28 days of initial diagnosis, the Cp values had a mean of 31.93 with a standard deviation of 1.22 (Fig. 4c). The overall decreased mean Cp value across all compiled positive PCR tests relative to the long-term shedder’s PCR test Cp values, implies a smaller amount of viral RNA available for amplification in the swab samples from long-term shedders (post 21 and 28 days of initial diagnosis).
Distributions of RT-PCR Crossing point (Cp) values: a all reported SARS-CoV-2-positive tests; b the last reported SARS-CoV-2-positive test for each patient who continue to shed viral RNA beyond 21 days of initial diagnosis; and c the last reported SARS-CoV-2-positive test for each patient who continue to shed viral RNA beyond 28 days of initial diagnosis.
Discussion
A recent study analyzing the fecal samples and respiratory swabs of 74 COVID-19 patients observed SARS-CoV-2-positive swabs with a mean duration of 15.4 days and standard deviation of 6.7 days from the first symptom onset14. Studies focusing on the temporal profiles of viral shedding suggest that the viral loads are highest at symptom onset, and subsequently decrease over the following 21 day13,15 and that live virus could no longer be cultured after day 8, leading to the hypothesis that SARS-CoV-2 infectiousness may decline from the time of symptom onset12,13. Whether such experimental results are generalizable to all SARS-CoV-2-positive patients that are long-term shedders is an important follow-up question.
Based on a recent study that characterized SARS-CoV-2 viral replication as a function of RT-PCR Cp values7, we attempted to predict the percentage of positive cultures. A characterization of 488 PCR tests from 208 SARS-CoV-2-positive patients in our study suggests a predicted percentage of positive cultures with a mean 49.2% and standard deviation 23.7% (Fig. 4 and Supplementary Fig. 1a). Likewise, extrapolating the corresponding distribution of predicted percentage of positive culture values in the 63 patients with viral RNA shedding beyond 21 days based on the last positive PCR tests suggests a mean of 33.3% and standard deviation of 7.6% (Fig. 4 and Supplementary Fig. 1b), while these figures beyond the 28 days threshold would have a mean of 33.6% and standard deviation of 8.2% (Fig. 4 and Supplementary Fig. 1c). Given it is impractical to effectively apply the relationship garnered between Cp values and positive cultures from different published RT-PCR assays towards this study, positive culture characterization for our RT-PCR assay would involve a follow-up investigation that incorporates longitudinal viral load assessments.
Although the SARS-CoV-2-positive RT-PCR tests by no means causally implicate replication-competent virus, the presence of viral RNA for several weeks from initial infection certainly warrants longitudinal monitoring of the viral load5,7. Furthermore, the question still remains as to why some SARS-CoV-2-positive patients harbor virus or viral RNA for far longer than other SARS-CoV-2-positive patients.
Our observations regarding non-hospitalized, IgG-seropositive, and long-term viral RNA shedders highlights the need for follow-up studies to characterize the neutralizing potential of antibodies generated by long-term viral RNA shedders and contextualize this in relation to viral loads and quantitative assays such as ddPCR5,6. The assessment of whether any of the IgG and IgM antibodies generated are able to neutralize the SARS-CoV-2 surface proteins (spike, envelope, and membrane) or the nucleocapsid protein16 would add an immunological lens to interpret the seroconversion noted in this study. Taken together, such additional research would help inform whether current CDC guidelines of 10 days self-quarantining for asymptomatic patients may be broadly satisfactory, including for patients that are noted to be long-term SARS-CoV-2 RNA shedders8.
Several factors could influence the persistent SARS-CoV-2 PCR positive status. Replicative fitness of a given virus is one of them. For instance, in HIV, not all viruses replicate equivalently, and differences may be attributable in part to polymorphisms in different genes17. For SARS-CoV-2, there are reports of different polymorphisms that have been speculated to impact disease severity or transmissibility, such as the D164G mutation in the spike (S) protein18. Another factor that may influence the persistence of PCR positivity could be the timing and robustness of the immune response. For example, given the role of the IFN response in viral shedding19, early IFN response is likely to be beneficial and reduce shedding, whereas late IFN response may be deleterious and delay clearance. Another potential factor to consider is the T-cell response20. When T cells express high levels of different effector pathway members (e.g. Perforin/granzyme B, IFN), they are thought to work better than if they produce only one effector pathway.
It may be noted that the clinical sensitivity of SARS-CoV-2 PCR tests has been debated21, and certainly there are anecdotal examples from our own clinic experience where critical ill SARS-CoV-2-positive patients can switch from a SARS-CoV-2-PCR positive status to a SARS-CoV-2-PCR negative status within a short period of time. To robustly enable scientific assessment of the sensitivity of the routine RT-PCR testing data analyzed here, we summarized the entire pattern of serial PCR outcomes across the 5569 COVID-19 patients in this study. This analysis shows that the vast majority of the COVID-19 patients subjected to our RT-PCR assays do produce consistent results, as determined by multiple contiguous PCR tests resulting in the same outcome. There is a small minority of COVID-19 patients where aberrant switching of PCR results is indeed observed, with the underlying reasons undetermined at this juncture.
In order to understand whether long-term SARS-CoV-2 RNA shedders display any other distinctive features from the structured EHR, we defined a control cohort of COVID-19 patients with an upper bound of infection duration between 1 and 13 days (“short-term shedders”). We compared the long-term shedders with this control cohort by analyzing the counts of over 15,000 features constituting the fields of structured EHR databases, including diagnosis, ICD codes, medication history, immunization records, procedures, and demographics (see Methods section). We do not find any significant distinguishing clinical features for long-term shedders compared to short-term shedders across multiple scenarios: (1) all patients, features from last 90 days, (2) all patients, features from after diagnosis, (3) all patients, features from 21 days after diagnosis, (4) all patients, features from 28 days after diagnosis, (5) non-hospitalized patients, features from last 90 days, (6) non-hospitalized patients, features from 21 days after diagnosis, (7) non-hospitalized patients, features from 28 days after diagnosis, and (8) non-hospitalized patients, features from diagnosis date.
While this preliminary observation from structured EHR counts has to be monitored as more SARS-CoV-2-positive patients’ longitudinal lab results are available, at this juncture, it appears that the majority of long-term shedders are non-hospitalized patients with likely mild or moderate symptoms that do not prompt their detailed clinical follow-up. Given that some of these long-term viral RNA shedders are already seropositive when they continue shedding, suggests that we cannot yet rely on IgG or any other antibody response alone to estimate immunity or odds of reinfection potential with SARS-CoV-2 without investigating the salience of long-term RNA shedding. The fact that replication-competent virus in some of these long-term RNA shedders cannot be ruled out based on the data available from PCR Ct values, underlines the need for prolonged monitoring of viral loads and immune responses in such SARS-CoV-2-PCR patients.
Our findings raise important additional follow-up questions from the standpoint of analyzing actual complete lab testing results longitudinally for large COVID-19 patient cohorts. Recent studies have identified coagulation associated issues in COVID-19 patients22,23. Building on findings reported in this study, it may be interesting to examine the rate of change of coagulation signals (e.g. by longitudinal lab testing of platelet count, fibrinogen levels, and d-dimer values) and the levels of immune cells (e.g. neutrophils, monocytes, basophils, lymphocytes) in COVID-19 patients that are long-term SARS-CoV-2 RNA shedders versus patients who are able to more rapidly eliminate the viral RNA. Follow-up studies need to examine how the duration of SARS-CoV-2 PCR positive status correlates to the rate of IgG seroconversion and the presence of effective humoral immunity as measured by neutralizing antibodies.
Methods
SARS-CoV-2 diagnostic tests conducted by Mayo Clinic hospitals and health system
Patients seen at Mayo Clinic in Rochester MN were tested by either a laboratory-developed test or the Roche cobas SARS-CoV-2 assay24,25. The Roche cobas test was employed by the Mayo Clinic’s Florida hospitals, and the Abbott diagnostic test was used by the Mayo Clinic’s Arizona hospitals26. These SARS-CoV-2 PCR tests amplify different segments of the viral genome but are considered largely equivalent from the perspective of their analytical performance. The Logical Observation Identifiers Names and Codes (LOINC) code of the SARS-CoV-2 IgG test analyzed is 94563-4 (https://loinc.org/94563-4/)27. For the SARS-CoV-2 IgG test, patient serum samples were tested by the Euroimmun Inc. Anti-SARS-CoV-2 IgG ELISA (Lubeck, Germany) according to the manufacturer instructions and as described previously on the Agility automated ELISA analyzer (Dynex Technologies, Inc., Chantilly, VA)28. This is a qualitative ELISA for detection of IgG-class antibodies against a recombinant version of the SARS-CoV-2 spike subunit 1 (S1) protein and has received Food and Drug Administration Emergency Use Authorization.
Statistical analysis of longitudinal SARS-CoV-2 RT-PCR results
The features considered in the analysis to differentiate the SARS-CoV-2-positive patients that are persistently PCR positive include all structured entities from the EHR, including but not limited to demographics, diagnosis, International Statistical Classification of Diseases and Related Health Problems (ICD) codes, medication history, immunization record, procedures, vitals, and lab tests. Any feature which is enriched significantly towards either shorter durations (<14 days between first positive to second negative test, as depicted in Fig. 2b) or longer durations (≥28 days between first positive to recent/final positive test, as depicted in Fig. 2c) was noted down. During the observation period (n = 201; 99 persistently PCR positive patients; 102 control patients), there were 289 EHR-derived features that were considered, including potentially prior to each patient’s COVID-19 diagnosis. The 2-proportion z-test p-value (after Benjamini–Hochberg (BH) adjustment for multiple hypothesis correction) was used to assess the differences of each feature between the persistently PCR positive patients and the control cohort, defined as those SARS-CoV-2-positive patients with an upper bound of infection duration between 1 and 13 days. The procedure was as follows:
-
(1)
Filter by features which are present in overall at least 10% of the patients we are looking at.
-
(2)
It is possible that there is a bias of more overall features towards the long-term or control cohort. We are not interested in this bias. To account for this, for each feature, we compute the “baseline” proportion difference, i.e., the weighted mean proportion of persistently positive patients that are positive for that feature minus the weighted mean proportion of control cohort which is positive for that feature. Call this baseline difference O (we have one such O for each feature).
-
(3)
Perform a 2-proportion z-test for whether the difference between feature-positive rate in the long-term cohort and feature-positive rate in the control cohort is significantly different from the baseline O.
-
(4)
Adjust these p-values for multiple hypotheses using the Benjamini–Hochberg procedure (with False Discovery Rate (FDR) controlled at 0.1 level).
We repeated the above procedure for slightly different underlying data as well; in particular, we re-ran on the following variants:
-
(i)
We filtered to look only at patients who were not hospitalized (as those would be of most concern).
-
(ii)
Each binary feature (phenotype, lab test, etc) occurred at a particular day in the patient’s record. We filtered by only those features which occur 0, 21, or 28 days following diagnosis.
-
(iii)
Variations (i) and (ii) together
Prediction of positive culture probability by RT-PCR Cp value
Estimated probability of positive culture (‘y’) by RT-PCR cycle threshold Crossing point (Cp) values (‘x’) was calculated using the following formula.
References
Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/ (2020).
Phelan, A. L. COVID-19 immunity passports and vaccination certificates: scientific, equitable, and legal challenges. Lancet 395, 1595–1598 (2020).
Chen, Y. et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J. Med. Virol. https://doi.org/10.1002/jmv.25825 (2020).
Qu, Y.-M., Kang, E.-M. & Cong, H.-Y. Positive result of Sars-Cov-2 in sputum from a cured patient with COVID-19. Travel Med. Infect. Dis. 34, 101619 (2020).
Suo, T. et al. ddPCR: a more accurate tool for SARS-CoV-2 detection in low viral load specimens. Emerg. Microbes Infect. 1, 1–30 (2020).
Dong, L. et al. Highly accurate and sensitive diagnostic detection of SARS-CoV-2 by digital PCR. Talanta. https://doi.org/10.1101/2020.03.14.20036129 (2020).
La Scola, B. et al. Viral RNA load as determined by cell culture as a management tool for discharge of SARS-CoV-2 patients from infectious disease wards. Eur. J. Clin. Microbiol. Infect. Dis. 39, 1059–1061 (2020).
CDC. Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/end-home-isolation.html (2020).
Richardson, S. et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. https://doi.org/10.1001/jama.2020.6775 (2020).
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395, 1054–1062 (2020).
Kucirka, L. M., Lauer, S. A., Laeyendecker, O., Boon, D. & Lessler, J. Variation in false-negative rate of reverse transcriptase polymerase chain reaction–based SARS-CoV-2 tests by time since exposure. Ann. Int. Med. https://doi.org/10.7326/m20-1495 (2020).
Wölfel, R. et al. Virological assessment of hospitalized patients with COVID-2019. Nature 581, 465–469 (2020).
He, X. et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 26, 672–675 (2020).
Wu, Y. et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol. Hepatol. 5, 434–435 (2020).
To, K. K.-W. et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect. Dis. 20, 565–574 (2020).
Zhou, G. & Zhao, Q. Perspectives on therapeutic neutralizing antibodies against the Novel Coronavirus SARS-CoV-2. Int. J. Biol. Sci. 16, 1718–1723 (2020).
Natesampillai, S. et al. Patients with discordant responses to antiretroviral therapy have impaired killing of HIV-infected T cells. PLoS Pathog. 6, e1001213 (2010).
Korber, B. et al. Spike mutation pipeline reveals the emergence of a more transmissible form of SARS-CoV-2. https://doi.org/10.1101/2020.04.29.069054 (2020).
Klinkhammer, J. et al. IFN-λ prevents influenza virus spread from the upper airways to the lungs and limits virus transmission. Elife 7, e33354 (2018).
Sridhar, S. et al. Cellular immune correlates of protection against symptomatic pandemic influenza. Nat. Med. 19, 1305–1312 (2013).
Vogels, C. B. F. et al. Analytical sensitivity and efficiency comparisons of SARS-COV-2 qRT-PCR primer-probe sets. Nat. Microbiol. 5, 1299–1305 (2020).
Pawlowski, C. et al. Longitudinal laboratory testing tied to PCR diagnostics in COVID-19 patients reveals temporal evolution of distinctive coagulopathy signatures. https://doi.org/10.1101/2020.05.21.20109439 (2020).
Levi, M., Thachil, J., Iba, T. & Levy, J. H. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 7, e438–e440 (2020).
Rodino, K. G. et al. Evaluation of saline, phosphate-buffered saline, and minimum essential medium as potential alternatives to viral transport media for SARS-CoV-2 testing. J. Clin. Microbiol. 58, 1–2 (2020).
Roche diagnostics. cobas® SARS-CoV-2 Test (for the COVID-19 Coronavirus) | Roche Diagnostics. Diagnostics. https://diagnostics.roche.com/us/en/products/params/cobas-sars-cov-2-test.html (2020).
Abbott RealTime SARS-CoV-2 Assay (EUA) | Abbott Molecular. https://www.molecular.abbott/us/en/products/infectious-disease/RealTime-SARS-CoV-2-Assay (2020).
LOINC. SARS-CoV-2 (COVID-19) IgG Ab [Presence] in Serum or Plasma by Immunoassay Active. https://loinc.org/94563-4/ (2020).
Theel, E. S. et al. The role of antibody testing for SARS-CoV-2: is there one? J. Clin. Microbiol. 58 (2020).
Acknowledgements
The authors thank Mathai Mammen, Murali Aravamudan, Patrick Lenehan, Will Gibson, Jacob Martin, Travis Hughes, and Tyler Wagner for their helpful feedback on this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A.D.B. is a consultant for Abbvie, is on scientific advisory boards for nference and Zentalis, and is founder and President of Splissen therapeutics. E.S.T. is on the consulting/advisory board of Roche Diagnostics/Accelerate Diagnostics; has speaking associated engagement with Bio-Rad Diagnostics and research associated engagement with Ortho-Clinical Diagnostics. One or more of the investigators associated with this project and Mayo Clinic have a Financial Conflict of Interest in technology used in the research and that the investigator(s) and Mayo Clinic may stand to gain financially from the successful outcome of the research. This research has been reviewed by the Mayo Clinic Conflict of Interest Review Board and is being conducted in compliance with Mayo Clinic Conflict of Interest policies. The authors from nference have financial interests in nference.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Edited by Chiara Agrati
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Agarwal, V., Venkatakrishnan, A.J., Puranik, A. et al. Long-term SARS-CoV-2 RNA shedding and its temporal association to IgG seropositivity. Cell Death Discov. 6, 138 (2020). https://doi.org/10.1038/s41420-020-00375-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41420-020-00375-y
This article is cited by
-
A case of COVID-19 reinfection in a hemodialysis patient: the role of antibody in SARS-CoV-2 infection
CEN Case Reports (2022)
-
Evidence of SARS-CoV-2 reinfection: analysis of 35,000 subjects and overview of systematic reviews
Clinical and Experimental Medicine (2022)
-
A Novel Prediction Model for Long-Term SARS-CoV-2 RNA Shedding in Non-Severe Adult Hospitalized Patients with COVID-19: A Retrospective Cohort Study
Infectious Diseases and Therapy (2021)