Abstract
Background
Immune-related adverse events (irAEs) have been found to predict PD-L1 inhibitor efficacy in metastatic NSCLC. However, the relation of irAEs to clinical outcome for nonmetastatic NSCLC has remained unknown.
Methods
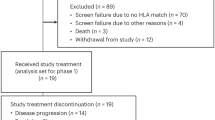
In this multicenter prospective study of Stage III NSCLC treated with PACIFIC regimen, the relation of irAEs to PFS was evaluated by 8-week landmark analysis to minimise lead-time bias as well as by multivariable analysis adjusted for baseline factors. irAEs were categorised as mild or nonmild according to whether they were treated with systemic steroid.
Results
Median PFS was 16.0 months, not reached, and 9.7 months for patients without (85 cases) or with mild (21 cases) or nonmild (21 cases) irAEs, respectively. Multivariable analysis indicated that nonmild irAEs were associated with poor PFS, with HRs of 3.86 (95% CI, 1.31–11.38) compared with no irAEs and 11.58 (95% CI, 2.11–63.63) compared with mild irAEs. This pattern was consistent after irAE grade, the number of durvalumab doses and immune profiles (PD-L1 score, CD8+ tumour-infiltrating lymphocyte density, and tumour mutation burden) were taken into consideration.
Conclusions
The development of mild irAEs might predict a better survival outcome, whereas immunosuppressive steroid–treated irAEs were associated with a worse outcome, regardless of baseline clinical and immune profiles.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data generated in this study are not publicly available as restricted by the study protocol due to the possibility that could compromise patient privacy or consent, but are possibly available upon reasonable request from the corresponding author.
References
Ribas A, Wolchok JD. Cancer immunotherapy using checkpoint blockade. Science. 2018;359:1350–5. https://doi.org/10.1126/science.aar4060.
Martins F, Sofiya L, Sykiotis GP, Lamine F, Maillard M, Fraga M, et al. Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance. Nat Rev Clin Oncol. 2019;16:563–80. https://doi.org/10.1038/s41571-019-0218-0.
Das S, Johnson DB. Immune-related adverse events and anti-tumor efficacy of immune checkpoint inhibitors. J Immunother Cancer. 2019;7:306 https://doi.org/10.1186/s40425-019-0805-8.
Conroy M, Naidoo J. Immune-related adverse events and the balancing act of immunotherapy. Nat Commun. 2022;13:392. https://doi.org/10.1038/s41467-022-27960-2.
Sullivan RJ, Weber JS. Immune-related toxicities of checkpoint inhibitors: mechanisms and mitigation strategies. Nat Rev Drug Discov. 2022;21:495–508. https://doi.org/10.1038/s41573-021-00259-5.
Haratani K, Hayashi H, Chiba Y, Kudo K, Yonesaka K, Kato R, et al. Association of immune-related adverse events with nivolumab efficacy in non-small-cell lung cancer. JAMA Oncol. 2018;4:374–8. https://doi.org/10.1001/jamaoncol.2017.2925.
Zhang Q, Wang W, Yuan Q, Li L, Wang YC, Chi CZ, et al. Correlation between immune-related adverse events and the efficacy of PD-1/PD-L1 inhibitors in the treatment of non-small cell lung cancer: systematic review and meta-analysis. Cancer Chemother Pharm. 2022;89:1–9. https://doi.org/10.1007/s00280-021-04375-2.
Socinski MA, Jotte RM, Cappuzzo F, Nishio M, Mok TSK, Reck M, et al. Association of immune-related adverse events with efficacy of atezolizumab in patients with non-small cell lung cancer: pooled analyses of the phase 3 IMpower130, IMpower132, and IMpower150 Randomized Clinical Trials. JAMA Oncol. 2023. https://doi.org/10.1001/jamaoncol.2022.7711.
Vansteenkiste J, Wauters E, Reymen B, Ackermann CJ, Peters S, De Ruysscher D. Current status of immune checkpoint inhibition in early-stage NSCLC. Ann Oncol. 2019;30:1244–53. https://doi.org/10.1093/annonc/mdz175.
Spigel DR, Faivre-Finn C, Gray JE, Vicente D, Planchard D, Paz-Ares L, et al. Five-year survival outcomes from the PACIFIC trial: durvalumab after chemoradiotherapy in stage iii non-small-cell lung cancer. J Clin Oncol. 2022;40:1301–11. https://doi.org/10.1200/JCO.21.01308.
Desilets A, Blanc-Durand F, Lau S, Hakozaki T, Kitadai R, Malo J, et al. Durvalumab therapy following chemoradiation compared with a historical cohort treated with chemoradiation alone in patients with stage III non-small cell lung cancer: a real-world multicentre study. Eur J Cancer. 2021;142:83–91. https://doi.org/10.1016/j.ejca.2020.10.008.
Girard N, Bar J, Garrido P, Garassino MC, McDonald F, Mornex F, et al. Treatment characteristics and real-world progression-free survival in patients with unresectable stage III NSCLC who received durvalumab after chemoradiotherapy: findings from the PACIFIC-R study. J Thorac Oncol. 2023;18:181–93. https://doi.org/10.1016/j.jtho.2022.10.003.
Voong KR, Hazell SZ, Fu W, Hu C, Lin CT, Ding K, et al. Relationship between prior radiotherapy and checkpoint-inhibitor pneumonitis in patients with advanced non-small-cell lung cancer. Clin Lung Cancer. 2019;20:e470–e479. https://doi.org/10.1016/j.cllc.2019.02.018.
Lu X, Wang J, Zhang T, Zhou Z, Deng L, Wang X, et al. Comprehensive pneumonitis profile of thoracic radiotherapy followed by immune checkpoint inhibitor and risk factors for radiation recall pneumonitis in lung cancer. Front Immunol. 2022;13:918787. https://doi.org/10.3389/fimmu.2022.918787.
Arbour KC, Mezquita L, Long N, Rizvi H, Auclin E, Ni A, et al. Impact of baseline steroids on efficacy of programmed cell death-1 and programmed death-ligand 1 blockade in patients with non-small-cell lung cancer. J Clin Oncol. 2018;36:2872–8. https://doi.org/10.1200/JCO.2018.79.0006.
Dall’Olio FG, Rizzo A, Mollica V, Massucci M, Maggio I, Massari F. Immortal time bias in the association between toxicity and response for immune checkpoint inhibitors: a meta-analysis. Immunotherapy. 2021;13:257–70. https://doi.org/10.2217/imt-2020-0179.
Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. New Engl J Med. 2017;377:1919–29. https://doi.org/10.1056/NEJMoa1709937.
Haratani K, Nakamura A, Mamesaya N, Mitsuoka S, Yoneshima Y, Saito R, et al. Tumor microenvironment landscape of NSCLC reveals resistance mechanisms for programmed death-ligand 1 blockade after chemoradiotherapy: a multicenter prospective biomarker study (WJOG11518L:SUBMARINE). J Thorac Oncol. 2023;18:1334–50. https://doi.org/10.1016/j.jtho.2023.06.012.
Brahmer JR, Lacchetti C, Schneider BJ, Atkins MB, Brassil KJ, Caterino JM, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2018;36:1714–68. https://doi.org/10.1200/JCO.2017.77.6385.
Tokunaga A, Sugiyama D, Maeda Y, Warner AB, Panageas KS, Ito S, et al. Selective inhibition of low-affinity memory CD8(+) T cells by corticosteroids. J Exp Med. 2019;216:2701–13. https://doi.org/10.1084/jem.20190738.
Haratani K, Hayashi H, Tanaka T, Kaneda H, Togashi Y, Sakai K, et al. Tumor immune microenvironment and nivolumab efficacy in EGFR mutation-positive non-small-cell lung cancer based on T790M status after disease progression during EGFR-TKI treatment. Ann Oncol. 2017;28:1532–9. https://doi.org/10.1093/annonc/mdx183.
Haratani K, Hayashi H, Takahama T, Nakamura Y, Tomida S, Yoshida T, et al. Clinical and immune profiling for cancer of unknown primary site. J Immunother Cancer. 2019;7:251. https://doi.org/10.1186/s40425-019-0720-z.
Isomoto K, Haratani K, Hayashi H, Shimizu S, Tomida S, Niwa T, et al. Impact of EGFR-TKI treatment on the tumor immune microenvironment in EGFR mutation-positive non-small cell lung cancer. Clin Cancer Res. 2020;26:2037–46. https://doi.org/10.1158/1078-0432.CCR-19-2027.
Takeda M, Sakai K, Hayashi H, Tanaka K, Haratani K, Takahama T, et al. Impact of coexisting gene mutations in EGFR-mutated non-small cell lung cancer before treatment on EGFR T790M mutation status after EGFR-TKIs. Lung Cancer. 2020;139:28–34. https://doi.org/10.1016/j.lungcan.2019.10.028.
Hayashi H, Sugawara S, Fukuda Y, Fujimoto D, Miura S, Ota K, et al. A randomized phase II study comparing nivolumab with carboplatin-pemetrexed for EGFR-mutated NSCLC with resistance to EGFR tyrosine kinase inhibitors (WJOG8515L). Clin Cancer Res. 2022;28:893–902. https://doi.org/10.1158/1078-0432.CCR-21-3194.
Haratani K, Yonesaka K, Takamura S, Maenishi O, Kato R, Takegawa N, et al. U3-1402 sensitizes HER3-expressing tumors to PD-1 blockade by immune activation. J Clin Investig. 2020;130:374–88. https://doi.org/10.1172/JCI126598.
Nishikawa H, Koyama S. Mechanisms of regulatory T cell infiltration in tumors: implications for innovative immune precision therapies. J Immunother Cancer. 2021;9. https://doi.org/10.1136/jitc-2021-002591.
Suzuki S, Haratani K, Hayashi H, Chiba Y, Tanizaki J, Kato R, et al. Association of tumour burden with the efficacy of programmed cell death-1/programmed cell death ligand-1 inhibitors for treatment-naive advanced non-small-cell lung cancer. Eur J Cancer. 2022;161:44–54. https://doi.org/10.1016/j.ejca.2021.11.011.
Brahmer JR, Abu-Sbeih H, Ascierto PA, Brufsky J, Cappelli LC, Cortazar FB, et al. Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immune checkpoint inhibitor-related adverse events. J Immunother Cancer. 2021;9. https://doi.org/10.1136/jitc-2021-002435.
Park R, Lopes L, Cristancho CR, Riano IM, Saeed A. Treatment-related adverse events of combination immune checkpoint inhibitors: systematic review and meta-analysis. Front Oncol. 2020;10:258 https://doi.org/10.3389/fonc.2020.00258.
Zhou X, Yao Z, Yang H, Liang N, Zhang X, Zhang F. Are immune-related adverse events associated with the efficacy of immune checkpoint inhibitors in patients with cancer? A systematic review and meta-analysis. BMC Med. 2020;18:87. https://doi.org/10.1186/s12916-020-01549-2.
Zhang YC, Zhu TC, Nie RC, Lu LH, Xiang ZC, Xie D, et al. Association between early immune-related adverse events and survival in patients treated with PD-1/PD-L1 inhibitors. J Clin Med. 2023;12. https://doi.org/10.3390/jcm12030736.
Hussaini S, Chehade R, Boldt RG, Raphael J, Blanchette P, Maleki Vareki S, et al. Association between immune-related side effects and efficacy and benefit of immune checkpoint inhibitors—a systematic review and meta-analysis. Cancer Treat Rev. 2021;92:102134. https://doi.org/10.1016/j.ctrv.2020.102134.
Fan Y, Xie W, Huang H, Wang Y, Li G, Geng Y, et al. Association of immune related adverse events with efficacy of immune checkpoint inhibitors and overall survival in cancers: a systemic review and meta-analysis. Front Oncol. 2021;11:633032. https://doi.org/10.3389/fonc.2021.633032.
Haratani K, Hayashi H, Nakagawa K. Association of immune-related adverse events with immune checkpoint inhibitor efficacy: real or imaginary? BMC Med. 2020;18:111. https://doi.org/10.1186/s12916-020-01583-0.
Baverel PG, Dubois VFS, Jin CY, Zheng Y, Song X, Jin X, et al. Population pharmacokinetics of durvalumab in cancer patients and association with longitudinal biomarkers of disease status. Clin Pharm Ther. 2018;103:631–42. https://doi.org/10.1002/cpt.982.
Sewell AK. Why must T cells be cross-reactive? Nat Rev Immunol. 2012;12:669–77. https://doi.org/10.1038/nri3279.
Bomze D, Hasan Ali O, Bate A, Flatz L. Association between immune-related adverse events during anti-PD-1 therapy and tumor mutational burden. JAMA Oncol. 2019;5:1633–5. https://doi.org/10.1001/jamaoncol.2019.3221.
Kerepesi C, Bakacs T, Moss RW, Slavin S, Anderson CC. Significant association between tumor mutational burden and immune-related adverse events during immune checkpoint inhibition therapies. Cancer Immunol Immunother. 2020;69:683–7. https://doi.org/10.1007/s00262-020-02543-6.
Sugimoto T, Fujimoto D, Sato Y, Tamiya M, Yokoi T, Taniguchi Y, et al. Prospective multicenter cohort study of durvalumab for patients with unresectable stage III non-small cell lung cancer and grade 1 radiation pneumonitis. Lung Cancer. 2022;171:3–8. https://doi.org/10.1016/j.lungcan.2022.07.005.
Faehling M, Schumann C, Christopoulos P, Hoffknecht P, Alt J, Horn M, et al. Durvalumab after definitive chemoradiotherapy in locally advanced unresectable non-small cell lung cancer (NSCLC): real-world data on survival and safety from the German expanded-access program (EAP). Lung Cancer. 2020;150:114–22. https://doi.org/10.1016/j.lungcan.2020.10.006.
Freeman-Keller M, Kim Y, Cronin H, Richards A, Gibney G, Weber JS. Nivolumab in resected and unresectable metastatic melanoma: characteristics of immune-related adverse events and association with outcomes. Clin Cancer Res. 2016;22:886–94. https://doi.org/10.1158/1078-0432.CCR-15-1136.
Eggermont AMM, Kicinski M, Blank CU, Mandala M, Long GV, Atkinson V, et al. Association between immune-related adverse events and recurrence-free survival among patients with stage III melanoma randomized to receive pembrolizumab or placebo: a secondary analysis of a randomized clinical trial. JAMA Oncol. 2020;6:519–27. https://doi.org/10.1001/jamaoncol.2019.5570.
Tsujino K, Hashimoto T, Shimada T, Yoden E, Fujii O, Ota Y, et al. Combined analysis of V20, VS5, pulmonary fibrosis score on baseline computed tomography, and patient age improves prediction of severe radiation pneumonitis after concurrent chemoradiotherapy for locally advanced non-small-cell lung cancer. J Thorac Oncol. 2014;9:983–90. https://doi.org/10.1097/JTO.0000000000000187.
Acknowledgements
The authors thank all patients, their families, and the investigators who participated in this study; members of the WJOG Data Center (in particular, Koji Takeda, and Shinichiro Nakamura) for central data management and administrative support; and Haruka Yamaguchi, Yume Shinkai, Michiko Kitano, Mami Kitano, Shinji Kurashimo and Yoshihiro Mine of Kindai University Faculty of Medicine for technical support. Shunsuke Teraoka is currently an employee of AstraZeneca K.K.
Funding
This study was conducted by the West Japan Oncology Group (WJOG) Data Center with a research grant from AstraZeneca KK.
Author information
Authors and Affiliations
Contributions
K Haratani developed the hypothesis, designed the overall study concept, wrote the study protocol, provided clinical data and samples, supervised IHC experiments, performed FCM experiments, performed data analysis and interpreted the data, wrote the manuscript, and supervised the project. A Nakamura, N Mamesaya, K Sawa, Y Shiraishi, R Saito, J Tanizaki, Y Tamura, A Hata, K Tsuruno, T Sakamoto, S Teraoka, M Oki, H Watanabe, T Tokito, K Nagata and T Masuda provided clinical data and samples. Y Nakamura supervised IHC experiments and evaluated IHC staining. K Sakai performed genomic sequencing and processed genomic data. Y Chiba wrote the study protocol and supervised the statistical analysis. A Ito supervised IHC experiments, evaluated IHC staining, and provided administrative support. K Nishio, N Yamamoto, K Nakagawa and H Hayashi provided administrative support and supervised the project. All authors critically revised the manuscript for important intellectual content and approved the final version.
Corresponding author
Ethics declarations
Competing interests
K Haratani has received lecture fees or honoraria from AS ONE Corporation, Bristol-Myers Squibb Co. Ltd., MSD K.K., and Ono Pharmaceutical Co. Ltd.; and research funding from AstraZeneca K.K., and MSD K.K. A Nakamura has received lecture fees or honoraria from AstraZeneca K.K., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., MSD K.K., Nippon Kayaku Co. Ltd., Novartis Pharma K.K., Taiho Pharmaceutical Co. Ltd., and Thermo Fisher Scientific Inc. K Sawa has received lecture fees or honoraria from AstraZeneca K.K., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., Kyowa Kirin Co. Ltd., Nippon Boehringer Ingelheim Co. Ltd., Ono Pharmaceutical Co. Ltd., and Taiho Pharmaceutical Co. Ltd. Y Shiraishi has received lecture fees or honoraria from AstraZeneca K.K., Bristol-Myers Squibb Co. Ltd., Chugai Pharmaceutical Co. Ltd., Ono Pharmaceutical Co. Ltd., and Taiho Pharmaceutical Co. Ltd.; and research funding from Chugai Pharmaceutical Co. Ltd. J Tanizaki has received lecture fees or honoraria from AstraZeneca K.K., Boehringer Ingelheim Japan Inc., Bristol-Myers Squibb Co. Ltd., Chugai Pharmaceutical Co. Ltd., Daiichi Sankyo Co. Ltd., Eli Lilly Japan K.K., MSD K.K., Nihon Medi-Physics Co. Ltd., Nippon Kayaku Co. Ltd., Ono Pharmaceutical Co. Ltd., Pfizer Japan Inc., and Taiho Pharmaceutical Co. Ltd. A Hata has received lecture fees or honoraria from AstraZeneca K.K., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., MSD K.K., Nippon Boehringer Ingelheim Co. Ltd., Nippon Kayaku Co. Ltd., Pfizer Inc., and Taiho Pharmaceutical Co. Ltd.; and research funding from MSD K.K., Eli Lilly Japan K.K., Nippon Boehringer Ingelheim Co. Ltd., and AstraZeneca K.K. T Sakamoto has received lecture fees or honoraria from AstraZeneca K.K., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., Hisamitsu Pharmaceutical Co. Inc., Illumina K.K., Janssen Pharmaceutical K.K., Kyowa Kirin Co., Ltd., Merck KGaA, MSD K.K., Novartis Pharma K.K., Ono Pharmaceutical Co. Ltd., Pfizer Japan Inc., Taiho Pharmaceutical Co. Ltd., and Takeda Pharmaceutical Co., Ltd. S Teraoka has received lecture fees or honoraria from AstraZeneca K.K. Boehringer Ingelheim Japan Inc., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., Novartis Pharma K.K., Ono Pharmaceutical Co. Ltd., Pfizer R&D Japan G.K., and Taiho Pharmaceutical Co. Ltd.; and advisory board fees from Pfizer R&D Japan G.K. S Teraoka is currently an employee of AstraZeneca K.K. M. Oki has received lecture fees or honoraria from AMCO Inc., AstraZeneca K.K., Canon Medical Systems Corporation., Chugai Pharmaceutical Co. Ltd., Fujifilm Toyama Chemical Co. Ltd., Kaneka Medix Corp., Merit Medical Japan K.K., Novartis Pharma K.K., Olympus Corporation, and Sanofi K.K.; and research funding from AbbVie Inc., AstraZeneca K.K., Chugai Pharmaceutical Co. Ltd., Fujifilm Toyama Chemical Co. Ltd., GlaxoSmithKline K.K., Janssen Pharmaceutical K.K., MSD K.K., Ono Pharmaceutical Co. Ltd., Parxel International Corporation, Pfizer Japan Inc., and Sanofi K.K. Takaaki Tokito has received lecture fees or honoraria from AstraZeneca K.K., Boehringer Ingelheim Japan Inc., Bristol-Myers Squibb Co. Ltd., Chugai Pharmaceutical Co. Ltd., MSD K.K., Nippon Kayaku Co. Ltd., Novartis Pharma K.K., and Ono Pharmaceutical Co. Ltd. Takeshi Masuda has received lecture fees or honoraria from AstraZeneca K.K., Bristol-Myers Squibb Co. Ltd., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., Kyowa Kirin Co. Ltd., MSD K.K., Ono Pharmaceutical Co. Ltd., Otsuka Pharmaceutical Co. Ltd., and Taiho Pharmaceutical Co. Ltd.; and research funding from MSD K.K. Yasushi Nakamura has received consulting fees from LSI Medience Corporation., and Nikon Corporation.; and advisory fees from Agilent Technologies Inc. K Sakai has received lecture fees or honoraria from Chugai Pharmaceutical Co. Ltd., Hitachi Ltd., Life Technologies Corporation, Takeda Pharmaceutical Co. Ltd., and Yodosha Co. Ltd. Y Chiba has received lecture fees or honoraria from Chugai Pharmaceutical Co. Ltd. K. Nishio has received research funding from Clinical Research Support Center Kyushu, Eli Lilly Japan K.K., Hitachi Ltd., Nichirei Biosciences Inc., Nippon Boehringer Ingelheim Co. Ltd., North East Japan Study Group, Otsuka Pharmaceutical Co. Ltd., Sysmex Corporation, Thoracic Oncology Research Group and West Japan Oncology Group. N Yamamoto has received lecture fees or honoraria from Amgen Inc., AstraZeneca K.K., Bristol-Myers Squibb Co. Ltd., Chugai Pharmaceutical Co. Ltd., Daiichi Sankyo Co. Ltd., Eli Lilly Japan K.K., GlaxoSmithKline K.K., Guardant Health Japan Corp., Janssen Pharmaceutical K.K., Kyorin Pharmaceutical Co. Ltd., Kyowa Kirin Co. Ltd., Merck kGaA, MIYARISAN Pharmaceutical Co,, MSD K.K., Nippon Boehringer Ingelheim Co. Ltd., Nippon Kayaku Co. Ltd., Novartis Pharma K.K., Ono Pfizer Japan Inc., Pharmaceutical Co. Ltd., Otsuka Pharmaceutical Co. Ltd., Sanofi K.K., Taiho Pharmaceutical Co. Ltd., Takeda Pharmaceutical Co. Ltd., and TSUMURA & CO.; and advisory board fees from AstraZeneca K.K., Eli Lilly Japan K.K., and Takeda Pharmaceutical Co. Ltd.; and research funding from AbbVie Inc., Amgen Inc., Asahi Kasei Pharma Corporation, Astellas Pharma Inc., AstraZeneca K.K., Bristol-Myers Squibb Co. Ltd., Chugai Pharmaceutical Co. Ltd., Daiichi Sankyo Co. Ltd., Eisai Co. Ltd., Eli Lilly Japan K.K., Janssen Pharmaceutical K.K., MSD K.K., Nippon Boehringer Ingelheim Co. Ltd., Nippon Kayaku Co. Ltd., Nobelpharma Co. Ltd., Novartis Pharma K.K., Ono Pharmaceutical Co. Ltd., Otsuka Pharmaceutical Co. Ltd., Pfizer Japan Inc., Sanofi K.K., Shionogi & Co. Ltd., Taiho Pharmaceutical Co. Ltd., Takeda Pharmaceutical Co. Ltd., TOSOH CORPORATION. and TSUMURA & CO. K. Nakagawa has received lecture fees or honoraria from AstraZeneca K.K., Amgen Inc., Bayer Yakuhin Ltd., Care Net Inc., Chugai Pharmaceutical Co. Ltd., CMIC Co. Ltd., CMIC ShiftZero K.K., Eli Lilly Japan K.K., Japan Clinical Research Operations, Kyowa Kirin Co. Ltd., Life Technologies Japan Ltd., Merck Biopharma Co. Ltd., Medical Mobile Communications Co. Ltd, Medical Review Co. Ltd., MSD K.K., Nikkei Business Publications Inc., Nippon Boehringer Ingelheim Co. Ltd., Nippon Kayaku Co. Ltd., Novartis Pharma K.K., Ono Pharmaceutical Co. Ltd., Pfizer Japan Inc., Taiho Pharmaceutical Co. Ltd., TAIYO Pharma Co. Ltd., Takeda Pharmaceutical Co. Ltd., Yodosya Co. Ltd., and 3H Clinical Trial Inc.; and consulting fees from Eli Lilly Japan K.K., and Ono Pharmaceutical Co. Ltd.; and research funding from Amgen Inc., AstraZeneca K.K., Bristol-Myers Squibb Co. Ltd., Chugai Pharmaceutical Co. Ltd., Covance Japan Inc., Daiichi Sankyo Co. Ltd., Eisai Co. Ltd., Eli Lilly Japan K.K., EP-CRSU Co. Ltd., EPS Corporation, EPS International Co. Ltd., GlaxoSmithKline K.K., IQVIA Services JAPAN K.K., Janssen Pharmaceutical K.K., Japan Clinical Research Operations, Kissei Pharmaceutical Co. Ltd., Mebix Inc., Medical Research Support, MSD K.K., Mochida Pharmaceutical Co. Ltd., Nippon Boehringer Ingelheim Co. Ltd., Nippon Kayaku Co. Ltd., Novartis Pharma K.K., Ono Pharmaceutical Co. Ltd., Otsuka Pharmaceutical Co. Ltd., PAREXEL International Corp., PPD-SNBL K.K., PRA Health Sciences., Sanofi K.K., SRL Inc., SymBio Pharmaceuticals Limited., Syneos Health Clinical K.K., Sysmex Corporation., Taiho Pharmaceutical Co. Ltd., Takeda Pharmaceutical Co. Ltd.; and has patents pending with Daiichi Sankyo Co. Ltd. H. Hayashi has received lecture fees or honoraria from Amgen K.K., AstraZeneca K.K., Boehringer Ingelheim Japan Inc., Bristol-Myers Squibb Co. Ltd., Chugai Pharmaceutical Co. Ltd., Daiichi Sankyo Co. Ltd., Eli Lilly Japan K.K., Guardant health Inc., Kyorin Pharmaceutical Co. Ltd., Merck Biopharma Co. Ltd., MSD K.K., Novartis Pharmaceuticals K.K., Ono Pharmaceutical Co. Ltd., Shanghai Haihe Biopharm, Taiho Pharmaceutical Co. Ltd., Pfizer Japan Inc., and Takeda Pharmaceutical Co. Ltd.; and research funding from AbbVie Inc, Astellas Pharma Inc., AstraZeneca K.K., A2 Healthcare Corp., Bayer Yakuhin Ltd., Bristol-Myers Squibb Co. Ltd., Chugai Pharmaceutical Co. Ltd., CMIC ShiftZero K.K., Daiichi Sankyo Co. Ltd., Eisai Co. Ltd., Eli Lilly Japan K.K., EP-CRSU Co. Ltd., EPS Corporation., EPS International Co. Ltd., GRITSONE ONCOLOGY INC., ICON Japan K.K., inVentiv Health Japan, IQVIA Services JAPAN K.K., Kissei Pharmaceutical Co. Ltd., Kyowa Hakko Kirin Co. Ltd, Merck Biopharma Co. Ltd., Merck Serono Co. Ltd., MSD K.K., Linical Co. Ltd., Nippon Boehringer Ingelheim Co. Ltd., Novartis Pharma K.K., Ono Pharmaceutical Co. Ltd., Otsuka Pharmaceutical Co. Ltd., PAREXEL International Corp., Pfizer Japan Inc., Pfizer R&D Japan G.K., SymBio Pharmaceuticals Limited., Quintiles Inc., Syneos Health, Taiho Pharmaceutical Co. Ltd., and Takeda Pharmaceutical Co. Ltd. All other authors declare competing interests.
Ethics approval and consent to participate
This study was performed in accordance with the protocol and the Declaration of Helsinki. The full protocol and informed consent form were approved by the ethics committee of each institution. All participants provided written consent before study entry.
Consent for publication
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Haratani, K., Nakamura, A., Mamesaya, N. et al. Association of immune-related adverse events with durvalumab efficacy after chemoradiotherapy in patients with unresectable Stage III non-small cell lung cancer. Br J Cancer (2024). https://doi.org/10.1038/s41416-024-02662-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41416-024-02662-2