Abstract
Background
In treatment of colon cancer, strict waiting-time targets are enforced, leaving professionals no room to lengthen treatment intervals when advisable, for instance to optimise a patient’s health status by means of prehabilitation. Good quality studies supporting these targets are lacking. With this study we aim to establish whether a prolonged treatment interval is associated with a clinically relevant deterioration in overall and cancer free survival.
Methods
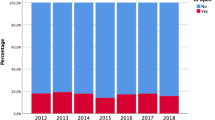
This retrospective multicenter non-inferiority study includes all consecutive patients who underwent elective oncological resection of a biopsy-proven primary non-metastatic colon carcinoma between 2010 and 2016 in six hospitals in the Southern Netherlands. Treatment interval was defined as time between diagnosis and surgical treatment. Cut-off points for treatment interval were ≤35 days and ≤49 days.
Findings
3376 patients were included. Cancer recurred in 505 patients (15.0%) For cancer free survival, a treatment interval >35 days and >49 days was non-inferior to a treatment interval ≤35 days. Results for overall survival were inconclusive, but no association was found.
Conclusion
For cancer free survival, a prolonged treatment interval, even over 49 days, is non-inferior to the currently set waiting-time target of ≤35 days. Therefore, the waiting-time targets set as fundamental objective in current treatment guidelines should become directional instead of strict targets
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data and material cannot be shared publicly because of ethical concerns. Patients were included on a no objection base to conduct retrospective data studies and publish findings, but were not asked for permission to publish full encrypted data. Data are available from the VieCuri Institutional Data Access (contact via wetenschapsbureau@viecuri.nl) for researchers who meet the criteria for access to confidential data.
References
Molenaar CJL, Janssen L, van der Peet DL, Winter DC, Roumen RMH, Slooter GD. Conflicting guidelines: a systematic review on the proper interval for colorectal cancer treatment. World J Surg. 2021;45:2235–50.
Franssen RFW, Strous MTA, Bongers BC, Vogelaar FJ, Janssen-Heijnen MLG. The association between treatment interval and survival in patients with colon or rectal cancer: a systematic review. World J Surg. 2021;45:2924–37.
de Roos MAJ, Hugen N, Hazebroek EJ, Spillenaar Bilgen EJ. Delayed surgical resection of primary left-sided obstructing colon cancer is associated with improved short- and long-term outcomes. J Surg Oncol. 2021;124:1146–53.
Lo BD, Caturegli G, Stem M, Biju K, Safar B, Efron JE, et al. The impact of surgical delays on short- and long-term survival among colon cancer patients. Am Surg. 2021;87:1783–92.
Kaltenmeier C, Shen C, Medich DS, Geller DA, Bartlett DL, Tsung A, et al. Time to surgery and colon cancer survival in the United States. Ann Surg. 2021;274:1025–31.
Davidson JTT, Abelson JS, Glasgow SC, Hunt SR, Mutch MG, Wise PE, et al. Delaying definitive resection in early stage (I/II) colon cancer appears safe up to 6 weeks. Am J Surg. 2021;222:402–7.
Hangaard Hansen C, Gogenur M, Tvilling Madsen M, Gogenur I. The effect of time from diagnosis to surgery on oncological outcomes in patients undergoing surgery for colon cancer: a systematic review. Eur J Surg Oncol. 2018;44:1479–85.
Gleason F, Chu DI, Kennedy GD, Kenzik KM. Early elective surgery after colon cancer diagnosis has higher risk of readmission and death. Ann Surg. 2021;273:188–94.
Bagaria SP, Heckman MG, Diehl NN, Parker A, Wasif N. Delay to colectomy and survival for patients diagnosed with colon cancer. J Invest Surg. 2019;32:350–7.
Kucejko RJ, Holleran TJ, Stein DE, Poggio JL. How soon should patients with colon cancer undergo definitive resection? Dis Colon Rectum. 2020;63:172–82.
Redaniel MT, Martin RM, Blazeby JM, Wade J, Jeffreys M. The association of time between diagnosis and major resection with poorer colorectal cancer survival: a retrospective cohort study. BMC Cancer. 2014;14:642.
Yun YH, Kim YA, Min YH, Park S, Won YJ, Kim DY, et al. The influence of hospital volume and surgical treatment delay on long-term survival after cancer surgery. Ann Oncol. 2012;23:2731–7.
Moore JS, Aulet TH. Colorectal cancer screening. Surg Clin North Am. 2017;97:487–502.
Lawrence VA, Hazuda HP, Cornell JE, Pederson T, Bradshaw PT, Mulrow CD, et al. Functional independence after major abdominal surgery in the elderly. J Am Coll Surg. 2004;199:762–72.
Barberan-Garcia A, Ubre M, Roca J, Lacy AM, Burgos F, Risco R, et al. Personalised prehabilitation in high-risk patients undergoing elective major abdominal surgery: a randomized blinded controlled trial. Ann Surg. 2018;267:50–56.
Berkel AEM, Bongers BC, Kotte H, Weltevreden P, de Jongh FHC, Eijsvogel MMM, et al. Effects of community-based exercise prehabilitation for patients scheduled for colorectal surgery with high risk for postoperative complications: results of a randomized clinical trial. Ann Surg. 2022;275:e299–e306.
Netherlands Cancer Registry (NKR) managed by IKNL.
Overheid.nl. Parliamentary paper. https://zoek.officielebekendmakingen.nl/kst-25170-31.html 2003.
Strous MTA, Janssen-Heijnen MLG, Vogelaar FJ. Impact of therapeutic delay in colorectal cancer on overall survival and cancer recurrence–is there a safe timeframe for prehabilitation? Eur J Surg Oncol. 2019;45:2295–301.
Wanis KN, Patel SVB, Brackstone M. Do moderate surgical treatment delays influence survival in colon cancer? Dis Colon Rectum. 2017;60:1241–9.
Molenaar CJL, Minnella EM, Coca-Martinez M, Ten Cate DWG, Regis M, Awasthi R, et al. Effect of multimodal prehabilitation on reducing postoperative complications and enhancing functional capacity following colorectal cancer surgery: the PREHAB randomized clinical trial. JAMA Surg. 2023;158:572–81.
Collaborative, P.-A.T. SupPoRtive Exercise Programmes for Accelerating REcovery after major ABdominal Cancer surgery trial (PREPARE-ABC): Pilot phase of a multicentre randomised controlled trial. Colorectal Dis. 2021;23:3008–22.
Gillis C, Li C, Lee L, Awasthi R, Augustin B, Gamsa A, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014;121:937–47.
Tevis SE, Kennedy GD. Postoperative complications: looking forward to a safer future. Clin Colon Rectal Surg. 2016;29:246–52.
Bousquet-Dion G, Awasthi R, Loiselle SE, Minnella EM, Agnihotram RV, Bergdahl A, et al. Evaluation of supervised multimodal prehabilitation programme in cancer patients undergoing colorectal resection: a randomized control trial. Acta Oncol. 2018;57:849–59.
Fowler AJ, Wan YI, Prowle JR, Chew M, Campbell D, Cuthbertson B, et al. Long-term mortality following complications after elective surgery: a secondary analysis of pooled data from two prospective cohort studies. Br J Anaesth. 2022;129:588–97.
Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242:326–41. discussion 341-3
Moonesinghe SR, Harris S, Mythen MG, Rowan KM, Haddad FS, Emberton M, et al. Survival after postoperative morbidity: a longitudinal observational cohort study. Br J Anaesth. 2014;113:977–84.
Justesen TF, Gogenur M, Clausen JSR, Mashkoor M, Rosen AW, Gogenur I. The impact of time to surgery on oncological outcomes in stage I-III dMMR colon cancer - a nationwide cohort study. Eur J Surg Oncol. 2023;49:106887.
Redaniel MT, Martin RM, Cawthorn S, Wade J, Jeffreys M. The association of waiting times from diagnosis to surgery with survival in women with localised breast cancer in England. Br J Cancer. 2013;109:42–9.
de Klerk M, van Dalen DH, Nahar-van Venrooij LMW, Meijerink W, Verdaasdonk EGG. A multimodal prehabilitation program in high-risk patients undergoing elective resection for colorectal cancer: a retrospective cohort study. Eur J Surg Oncol. 2021;47:2849–56.
Rydbeck D, Bock D, Haglind E, Angenete E, Onerup A. Survival in relation to time to start of curative treatment of colon cancer: a national register-based observational noninferiority study. Colorectal Dis. 2023;25:1613–21.
Acknowledgements
This study was financed by the Research fund VieCuri Medical Centre. The authors thank the registration team of the Netherlands Comprehensive Cancer Organisation (IKNL) for the collection of data for the Netherlands Cancer Registry. The results of this study were presented at ESSO 41 on the 19th October 2022 in Bordeaux, France.
Author information
Authors and Affiliations
Contributions
Guarantor of the integrity of the study: MS. Conceptualisation: MS, RF, CM, MJ, and FV. Literature research: MS, RF, and CM. Methodology: MS, FO, MJ, and FV. Formal analysis: MS and FO. Investigation: MS, RF, and CM. Recourses: EB, JB, GS, JM, JH, and FV. Data curation, analysis and interpretation: MS and FO. Manuscript preparation: MS, RF, and CM. Manuscript editing and review: FO, EB, JB, GS, JM, JH, AB, MJ, and FV. Visualisation: MS and RF. Project administration: MS. Funding acquisition: MS, AB, MJ, and FV.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interest.
Ethics approval and consent to participate
This study was approved by the research committee and the Board of Directors of all six participating hospitals. Data were obtained under the Dutch law ‘scientific research and statistics in the interest of public health, where asking for permission is not possible or inappropriate for several reasons’, unless patients had objected to the general use of their personal medical record for scientific research. Data were encrypted with an encryption key provided by the NCR. Encryption was shortly lifted to access the patients’ number for accessing his/her medical record. A waiver of informed consent was given by the METC Zuyderland under the reference number METCZ20200069.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Strous, M.T.A., Molenaar, C.J.L., Franssen, R.F.W. et al. Treatment interval in curative treatment of colon cancer, does it impact (cancer free) survival? A non-inferiority analysis. Br J Cancer 130, 251–259 (2024). https://doi.org/10.1038/s41416-023-02505-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02505-6