Abstract
Background
An association was observed between an inflammation-related risk score (IRRS) and worse overall survival (OS) among a cohort of mostly White women with invasive epithelial ovarian cancer (EOC). Herein, we evaluated the association between the IRRS and OS among Black women with EOC, a population with higher frequencies of pro-inflammatory exposures and worse survival.
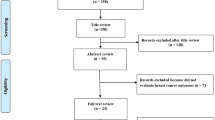
Methods
The analysis included 592 Black women diagnosed with EOC from the African American Cancer Epidemiology Study (AACES). Cox proportional hazards models were used to compute hazard ratios (HRs) and 95% confidence intervals (CIs) for the association of the IRRS and OS, adjusting for relevant covariates. Additional inflammation-related exposures, including the energy-adjusted Dietary Inflammatory Index (E-DIITM), were evaluated.
Results
A dose–response trend was observed showing higher IRRS was associated with worse OS (per quartile HR: 1.11, 95% CI: 1.01–1.22). Adding the E-DII to the model attenuated the association of IRRS with OS, and increasing E-DII, indicating a more pro-inflammatory diet, was associated with shorter OS (per quartile HR: 1.12, 95% CI: 1.02–1.24). Scoring high on both indices was associated with shorter OS (HR: 1.54, 95% CI: 1.16–2.06).
Conclusion
Higher levels of inflammation-related exposures were associated with decreased EOC OS among Black women.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated and/or analysed during the current study are available on reasonable request, in accordance with the NIH data sharing policy.
Code availability
All analyses were performed using R (version 4.2.0), and the code is available on reasonable request.
References
Torre LA, Trabert B, DeSantis CE, Miller KD, Samimi G, Runowicz CD, et al. Ovarian cancer statistics, 2018. CA Cancer J Clin. 2018;68:284–96.
Peres LC, Risch H, Terry KL, Webb PM, Goodman MT, Wu AH, et al. Racial/ethnic differences in the epidemiology of ovarian cancer: a pooled analysis of 12 case-control studies. Int J Epidemiol. 2018;47:1011.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33.
Terplan M, Smith EJ, Temkin SM. Race in ovarian cancer treatment and survival: a systematic review with meta-analysis. Cancer Causes Control. 2009;20:1139–50.
Howell EA, Egorova N, Hayes MP, Wisnivesky J, Franco R, Bickell N. Racial disparities in the treatment of advanced epithelial ovarian cancer. Obstet Gynecol. 2013;122:1025–32.
Basch E, Reeve BB, Mitchell SA, Clauser SB, Minasian LM, Dueck AC, et al. Development of the National Cancer Institute’s patient-reported outcomes version of the common terminology criteria for adverse events (PRO-CTCAE). J Natl Cancer Inst. 2014;106:dju244.
Du XL, Sun CC, Milam MR, Bodurka DC, Fang S. Ethnic differences in socioeconomic status, diagnosis, treatment, and survival among older women with epithelial ovarian cancer. Int J Gynecol Cancer. 2008;18:660–9.
Jemal A, Ward EM, Johnson CJ, Cronin KA, Ma J, Ryerson B, et al. Annual report to the nation on the status of cancer, 1975-2014, featuring survival. J Natl Cancer Inst. 2017;109:djx030.
Brenner DR, Scherer D, Muir K, Schildkraut J, Boffetta P, Spitz MR, et al. A review of the application of inflammatory biomarkers in epidemiologic cancer research. Cancer Epidemiol Biomark Prev. 2014;23:1729–51.
Schildkraut JM. Invited Commentary: Relationship between ovulation and markers of systemic inflammation versus markers of localized inflammation. Am J Epidemiol. 2020;189:671–3.
Hathaway CA, Wang T, Townsend MK, Vinci C, Jake-Schoffman DE, Saeed-Vafa D, et al. Lifetime exposure to cigarette smoke and risk of ovarian cancer by T-cell tumor immune infiltration. Cancer Epidemiol Biomark Prev. 2023;32:66–73.
Ye CJ, Feng T, Kwon HK, Raj T, Wilson M, Asinovski N, et al. Intersection of population variation and autoimmunity genetics in human T cell activation. Science. 2014;345:1254665.
Brieger KK, Peterson S, Lee AW, Mukherjee B, Bakulski KM, Alimujiang A, et al. Menopausal hormone therapy prior to the diagnosis of ovarian cancer is associated with improved survival. Gynecol Oncol. 2020;158:702–9.
Brieger KK, Phung MT, Mukherjee B, Bakulski KM, Anton-Culver H, Bandera EV, et al. High prediagnosis inflammation-related risk score associated with decreased ovarian cancer survival. Cancer Epidemiol Biomark Prev. 2022;31:443–52.
Schildkraut JM, Johnson C, Dempsey LF, Qin B, Terry P, Akonde M, et al. Survival of epithelial ovarian cancer in Black women: a society to cell approach in the African American cancer epidemiology study (AACES). Cancer Causes Control. 2022;34:251–65.
Peres LC, Moorman PG, Alberg AJ, Bandera EV, Barnholtz-Sloan J, Bondy M, et al. Lifetime number of ovulatory cycles and epithelial ovarian cancer risk in African American women. Cancer Causes Control. 2017;28:405–14.
Peres LC, Hebert JR, Qin B, Guertin KA, Bandera EV, Shivappa N, et al. Prediagnostic proinflammatory dietary potential is associated with all-cause mortality among African-American women with high-grade serous ovarian carcinoma. J Nutr. 2019;149:1606–16.
Peres LC, Bandera EV, Qin B, Guertin KA, Shivappa N, Hebert JR, et al. Dietary inflammatory index and risk of epithelial ovarian cancer in African American women. Int J Cancer. 2017;140:535–43.
Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–35.
Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S.: adults compliance with the Physical Activity Guidelines for Americans. Am J Prev Med. 2011;40:454–61.
Cavicchia PP, Steck SE, Hurley TG, Hussey JR, Ma Y, Ockene IS, et al. A New Dietary Inflammatory Index predicts interval changes in serum high-sensitivity C-reactive protein. J Nutr. 2009;139:2365–72.
Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014;17:1689–96.
Buuren S, van, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Softw. 2011;45:1–67.
Li R, Chambless L. Test for additive interaction in proportional hazards models. Ann Epidemiol. 2007;17:227–36.
VanderWeele TJ. Causal interactions in the proportional hazards model. Epidemiology. 2011;22:713–7.
Acknowledgements
We would like to acknowledge the AACES interviewers Brandy Arredondo, Rachel Boehm, Dannelle Charles, Melody Chavez, Lauren Dempsey, Kierstin Faw, Juliana Fucinari, Mary Kan, Mary Beth Kolbicz, Arianna Mason, Juana Paniagua, and Maelia Pendley. We also acknowledge the individuals responsible for facilitating case ascertainment across the sites, including Kevin Ward and Mackenzie Crawford (Georgia); Tingting Li and Lauren Maniscalco (Louisiana); Dhanya Chanumolu and Myneka Macenat (New Jersey); Paul Terry (Tennessee); Ann Hamilton (California), Mary Beth Kolbicz (Michigan); Cynthia Webb, JoElla Marting, and Heather Tipaldos (North Carolina); and Maxwell Akonde, Stephanie Chiodini, and Deb Hurley (South Carolina).
Funding
The AACES study was funded by the National Cancer Institute (R01CA142081 and R01CA237318). Additional support was provided by Metropolitan Detroit Cancer Surveillance System (MDCSS) with federal funds from the National Cancer Institute, National Institute of Health, Dept. of Health and Human Services, under Contract No. HHSN261201000028C and the Epidemiology Research Core, supported in part by NCI Center Grant (P30CA22453) to the Karmanos Cancer Institute, Wayne State University School of Medicine. This work has been supported in part by the Participant Research, Interventions, and Measurements Core Facility at the H. Lee Moffit Cancer Center & Research Institute, an NCI designated Comprehensive Cancer Center (P30-CA076292). LJC was supported by K99CA277580 from the National Cancer Institute of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
The following authors were a part of the writing group: CEJ, JMS, AJA, EVB, PT, ESP, BQ, HBM, MLC, MA, TAH, and LJC. The analysis was completed by: CEJ. The following authors provided comments and edits to the manuscript: LVP, AGS, ABL, and JRH. The following authors helped in data collection: JMSchildkraut, AJA, EVB, PT, MA, ESP, MLC, JRM, MB, AGS, and HBM. JRH developed the energy-adjusted dietary inflammatory index.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Western Institutional Review Board-Copernicus Group (WCG IRB). The study was performed in accordance with the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Johnson, C.E., Alberg, A.J., Bandera, E.V. et al. Association of inflammation-related exposures and ovarian cancer survival in a multi-site cohort study of Black women. Br J Cancer 129, 1119–1125 (2023). https://doi.org/10.1038/s41416-023-02385-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02385-w


