Abstract
Background
This systematic review and meta-analysis aimed to evaluate existing evidence on the relationship between diagnostic and treatment intervals and outcomes for colorectal cancer.
Methods
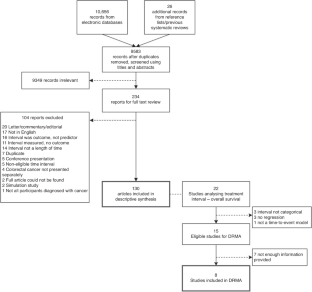
Four databases were searched for English language articles assessing the role of time before initial treatment in colorectal cancer on any outcome, including stage and survival. Two reviewers independently screened articles for inclusion and data were synthesised narratively. A dose–response meta-analysis was performed to examine the association between treatment interval and survival.
Results
One hundred and thirty papers were included in the systematic review, eight were included in the meta-analysis. Forty-five different intervals were considered in the time from first symptom to treatment. The most common finding was of no association between the length of intervals on any outcome. The dose–response meta-analysis showed a U-shaped association between the treatment interval and overall survival with the nadir at 45 days.
Conclusion
The review found inconsistent, but mostly a lack of, association between interval length and colorectal cancer outcomes, but study design and quality were heterogeneous. Meta-analysis suggests survival becomes increasingly poorer for those commencing treatment more than 45 days after diagnosis.
Registration
This review was registered, and the protocol is available, in PROSPERO, the international database of systematic reviews, with the registration ID CRD42021255864.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Data availability
Data used in this review is provided in Supplementary Appendices; any additional data are available upon request to the corresponding author.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Xi Y, Xu P. Global colorectal cancer burden in 2020 and projections to 2040. Transl Oncol. 2021;14:101174.
Emery J, Brown G, Macrae F, Bell C, Tse J, Skinner I, et al. Guidelines: colorectal cancer/the symptomatic patient. Sydney: Cancer Council Australia; 2017.
Neal RD. Do diagnostic delays in cancer matter? Br J Cancer. 2009;101:S9–s12.
Weller D, Vedsted P, Rubin G, Walter FM, Emery J, Scott S, et al. The Aarhus statement: improving design and reporting of studies on early cancer diagnosis. Br J Cancer. 2012;106:1262–7.
Aslam MI, Chaudhri S, Singh B, Jameson JS. The "two-week wait" referral pathway is not associated with improved survival for patients with colorectal cancer. Int J Surg. 2017;43:181–5.
Olesen F, Hansen RP, Vedsted P. Delay in diagnosis: the experience in Denmark. Br J Cancer. 2009;101:S5–8.
Walter F, Webster A, Scott S, Emery J. The Andersen Model of Total Patient Delay: a systematic review of its application in cancer diagnosis. J Health Serv Res Policy. 2012;17:110–8.
Ramos M, Esteva M, Cabeza E, Campillo C, Llobera J, Aguiló A. Relationship of diagnostic and therapeutic delay with survival in colorectal cancer: a review. Eur J Cancer. 2007;43:2467–78.
Ramos M, Esteva M, Cabeza E, Llobera J, Ruiz A. Lack of association between diagnostic and therapeutic delay and stage of colorectal cancer. Eur J Cancer. 2008;44:510–21.
Hanna TP, King WD, Thibodeau S, Jalink M, Paulin GA, Harvey-Jones E, et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020;371:m4087.
Whittaker TM, Abdelrazek MEG, Fitzpatrick AJ, Froud JLJ, Kelly JR, Williamson JS, et al. Delay to elective colorectal cancer surgery and implications for survival: a systematic review and meta-analysis. Colorectal Dis. 2021;23:1699–711.
Franssen RFW, Strous MTA, Bongers BC, Vogelaar FJ, Janssen-Heijnen MLG. The association between treatment interval and survival in patients with colon or rectal cancer: a systematic review. World J Surg. 2021;45:2924–37.
Hangaard Hansen C, Gögenur M, Tvilling Madsen M, Gögenur I. The effect of time from diagnosis to surgery on oncological outcomes in patients undergoing surgery for colon cancer: a systematic review. Eur J Surg Oncol. 2018;44:1479–85.
Neal RD, Tharmanathan P, France B, Din NU, Cotton S, Fallon-Ferguson J, et al. Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review. Br J Cancer. 2015;112:S92–107.
Castelo M, Sue-Chue-Lam C, Paszat L, Kishibe T, Scheer AS, Hansen BE, et al. Time to diagnosis and treatment in younger adults with colorectal cancer: a systematic review. PLoS ONE. 2022;17:e0273396.
Tørring ML, Frydenberg M, Hamilton W, Hansen RP, Lautrup MD, Vedsted P. Diagnostic interval and mortality in colorectal cancer: U-shaped association demonstrated for three different datasets. J Clin Epidemiol. 2012;65:669–78.
Rupassara KS, Ponnusamy S, Withanage N, Milewski PJ. A paradox explained? Patients with delayed diagnosis of symptomatic colorectal cancer have good prognosis. Colorectal Dis. 2006;8:423–9.
Crawford SC, Davis JA, Siddiqui NA, de Caestecker L, Gillis CR, Hole D, et al. The waiting time paradox: population based retrospective study of treatment delay and survival of women with endometrial cancer in Scotland. BMJ. 2002;325:196.
Crippa A, Discacciati A, Bottai M, Spiegelman D, Orsini N. One-stage dose-response meta-analysis for aggregated data. Stat Methods Med Res. 2019;28:1579–96.
Orsini N, Spiegelman D Meta-analysis of dose-response relationships. Handbook of meta-analysis. Boca Raton, FL: Chapman and Hall/CRC; 2020. p. 395-428.
Li Y, Gu M, Jing F, Cai S, Bao C, Wang J, et al. Association between physical activity and all cancer mortality: dose-response meta-analysis of cohort studies. Int J Cancer. 2016;138:818–32.
Wang F, Yeung KL, Chan WC, Kwok CC, Leung SL, Wu C, et al. A meta-analysis on dose-response relationship between night shift work and the risk of breast cancer. Ann Oncol. 2013;24:2724–32.
Drosdowsky A, Lamb KE, Bergin RJ, Boyd L, Milley K, IJ MJ, et al. A systematic review of methodological considerations in time to diagnosis and treatment in colorectal cancer research. Cancer Epidemiol. 2023;83:102323.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Veritas Health Innovation. Covidence systematic review software, Melbourne, Australia, 2023.
The Joanna Briggs Institute. Critical Appraisal Tools. 2023. https://joannabriggs.org/critical-appraisal-tools.
Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17:2815–34.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007;8:16.
PlotDigitizer. 2022. https://plotdigitizer.com/.
Il'yasova D, Hertz-Picciotto I, Peters U, Berlin JA, Poole C. Choice of exposure scores for categorical regression in meta-analysis: a case study of a common problem. Cancer Causes Control. 2005;16:383–8.
Taylor K. Wanting a particular reference category in categorical risk data. University of Oxford; 2022. https://www.cebm.ox.ac.uk/resources/data-extraction-tips-meta-analysis/reference-category-risk-data.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing, 2021.
Crippa A, Orsini N. Multivariate dose-response meta-analysis: the dosresmeta R package. J Stat Softw. 2016;72:1–15.
Gleason F, Chu DI, Kennedy GD, Kenzik KM. Early elective surgery after colon cancer diagnosis has higher risk of readmission and death. Ann Surg. 2021;273:188–94.
Kaltenmeier C, Shen C, Medich DS, Geller DA, Bartlett DL, Tsung A, et al. Time to surgery and colon cancer survival in the United States. Ann Surg. 2021;274:1025–31.
Lo BD, Caturegli G, Stem M, Biju K, Safar B, Efron JE, et al. The impact of surgical delays on short- and long-term survival among colon cancer patients. Am Surg. 2021;87:1783–92.
Harrell FE. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. Berlin: Springer; 2001.
Abdulaal A, Arhi C, Ziprin P. Effect of health care provider delays on short-term outcomes in patients with colorectal cancer: multicenter population-based observational study. Interact J Med Res. 2020;9:e15911.
Ahmed RN, Rai L, Samo KA, Saeed S, Salam A, Khan H, et al. Factors affecting delay in diagnosis of colorectal cancer: a cross‐sectional study from a tertiary care hospital of Karachi, Pakistan. Int J Clin Pract. 2021;75:e14529.
Amri R, Bordeianou LG, Sylla P, Berger DL. Treatment delay in surgically-treated colon cancer: does it affect outcomes? Ann Surg Oncol. 2014;21:3909–16.
Arbman G, Nilsson E, Störgren-Fordell V, Sjödahl R. A short diagnostic delay is more important for rectal cancer than for colonic cancer. Eur J Surg. 1996;162:899–904.
Arhi CS, Burns EM, Bottle A, Bouras G, Aylin P, Ziprin P, et al. Delays in referral from primary care worsen survival for patients with colorectal cancer: a retrospective cohort study. Br J Gen Pract. 2020;70:e463–e71.
Auvinen A. Social class and colon cancer survival in Finland. Cancer 1992;70:402–9.
Bagaria SP, Heckman MG, Diehl NN, Parker A, Wasif N. Delay to colectomy and survival for patients diagnosed with colon cancer. J Invest. Surg. 2019;32:350–7.
Bako G, Hill G, Ferenczi L, Hanson J. Factors influencing the survival of patients with cancer of the colon or rectum. Chronic Dis Can. 1988;9:101–4.
Barillari P, De Angelis R, Valabrega S, Indinnimeo M, Gozzo P, Ramacciato G, et al. Relationship of symptom duration and survival in patients with colorectal carcinoma. Eur J Surg Oncol. 1989;15:441–5.
Bassett ML, Bennett SA, Goulston KJ. Colorectal cancer. A study of 230 patients. Med J Aust. 1979;1:589–92.
Ben-Ishay O, Brauner E, Peled Z, Othman A, Person B, Kluger Y. Diagnosis of colon cancer differs in younger versus older patients despite similar complaints. Isr Med Assoc J. 2013;15:284–7.
Bharucha S, Hughes S, Kenyon V, Anderson ID, Carlson GL, Scott NA. Targets and elective colorectal cancer: outcome and symptom delay at surgical resection. Colorectal Dis. 2005;7:169–71.
Bjerkeset T, Søreide O. Symptoms in colorectal adenocarcinomas and their relation to tumor characteristics and survival. Dig Surg. 1988;5:61–5.
Cerdán-Santacruz C, Cano-Valderrama O, Cárdenas-Crespo S, Torres-García AJ, Cerdán-Miguel J. Colorectal cancer and its delayed diagnosis: have we improved in the past 25 years? Rev Esp Enferm Dig. 2011;103:458–63.
Chapuis PH, Dent OF, Fisher R, Newland RC, Pheils MT, Smyth E, et al. A multivariate analysis of clinical and pathological variables in prognosis after resection of large bowel cancer. Br J Surg. 1985;72:698–702.
Chen FW, Sundaram V, Chew TA, Ladabaum U. Advanced-stage colorectal cancer in persons younger than 50 years not associated with longer duration of symptoms or time to diagnosis. Clin Gastroenterol Hepatol. 2017;15:728–37.e3.
Clarke AM, Jones IS. Diagnostic accuracy and diagnostic delay in carcinoma of the large bowel. NZ Med J. 1970;71:341–7.
Comber H, Cronin DP, Deady S, Lorcain PO, Riordan P. Delays in treatment in the cancer services: impact on cancer stage and survival. Ir Med J. 2005;98:238–9.
Cubiella J, Lorenzo M, Baiocchi F, Tejido C, Conde A, Sande-Meijide M, et al. Impact of a colorectal cancer screening program implantation on delays and prognosis of non-screening detected colorectal cancer. World J Gastroenterol. 2021;27:6689–700.
Curtis NJ, West MA, Salib E, Ockrim J, Allison AS, Dalton R, et al. Time from colorectal cancer diagnosis to laparoscopic curative surgery-is there a safe window for prehabilitation? Int J Colorectal Dis. 2018;33:979–83.
Davidson JTT, Abelson JS, Glasgow SC, Hunt SR, Mutch MG, Wise PE, et al. Delaying definitive resection in early stage (I/II) colon cancer appears safe up to 6 weeks. Am J Surg. 2021;222:402–7.
de Roos MAJ, Hugen N, Hazebroek EJ, Spillenaar Bilgen EJ. Delayed surgical resection of primary left-sided obstructing colon cancer is associated with improved short- and long-term outcomes. J Surg Oncol. 2021;124:1146–53.
de Sousa JB, Souza CS, Fernandes MB, de Castro Durães L, de Almeida RM, Dos Santos AC, et al. Do young patients have different clinical presentation of colorectal cancer causing delay in diagnosis? Int J Colorectal Dis. 2014;29:519–27.
Delisle M, Helewa RM, Ward MA, Hochman DJ, Park J, McKay A. The association between wait times for colorectal cancer treatment and health care costs: a population-based analysis. Dis Colon Rectum. 2020;63:160–71.
Deng SX, An W, Gao J, Yin J, Cai QC, Yang M, et al. Factors influencing diagnosis of colorectal cancer: a hospital-based survey in China. J Dig Dis. 2012;13:517–24.
Di Girolamo C, Walters S, Gildea C, Benitez Majano S, Rachet B, Morris M. Can we assess cancer waiting time targets with cancer survival? A population-based study of individually linked data from the National Cancer Waiting Times monitoring dataset in England, 2009-2013. PLoS ONE. 2018;13:e0201288.
Dregan A, Møller H, Charlton J, Gulliford MC. Are alarm symptoms predictive of cancer survival?: population-based cohort study. Br J Gen Pract. 2013;63:e807–12.
Duff SE, Wood C, McCredie V, Levine E, Saunders MP, O'Dwyer ST. Waiting times for treatment of rectal cancer in North West England. J R Soc Med. 2004;97:117–8.
Edwards GC, Gamboa AC, Feng MP, Muldoon RL, Hopkins MB, Abdel-Misih S, et al. What’s the magic number? Impact of time to initiation of treatment for rectal cancer. Surgery. 2022;171:1185–92.
Eldar S, Kemeny MM, Terz JJ. Extended resections for carcinoma of the colon and rectum. Surg Gynecol Obstet. 1985;161:319–22.
Fegiz G, Barillari P, Ramacciato G, De Angelis R, Gozzo P, Indinnimeo M, et al. Right colon cancer: long-term results after curative surgery and prognostic significance of duration of symptoms. J Surg Oncol. 1989;41:250–5.
Fernández-de Castro JD, Baiocchi Ureta F, Fernández González R, Pin Vieito N, Cubiella Fernández J. The effect of diagnostic delay attributable to the healthcare system on the prognosis of colorectal cancer. Gastroenterol Hepatol. 2019;42:527–33.
Fisher DA, Zullig LL, Grambow SC, Abbott DH, Sandler RS, Fletcher RH, et al. Determinants of medical system delay in the diagnosis of colorectal cancer within the Veteran Affairs Health System. Dig Dis Sci. 2010;55:1434–41.
Flemming JA, Nanji S, Wei X, Webber C, Groome P, Booth CM. Association between the time to surgery and survival among patients with colon cancer: a population-based study. Eur J Surg Oncol. 2017;43:1447–55.
Garcia-Botello S, Martín-Arevalo J, Cozar-Lozano C, Benitez-Riesco A, Moro-Valdezate D, Pla-Martí V, et al. Does delaying curative surgery for colorectal cancer influence long-term disease-free survival? A cohort study. Langenbeck’s Arch Surg. 2021;406:2383–90.
Gómez-Domínguez E, Trapero-Marugán M, del Pozo AJ, Cantero J, Gisbert JP, Maté J. The colorectal carcinoma prognosis factors. Significance of diagnosis delay. Rev Esp Enferm Dig. 2006;98:322–9.
Gonzalez-Hermoso F, Perez-Palma J, Marchena-Gomez J, Lorenzo-Rocha N, Medina-Arana V. Can early diagnosis of symptomatic colorectal cancer improve the prognosis? World J Surg. 2004;28:716–20.
Goodman D, Irvin TT. Delay in the diagnosis and prognosis of carcinoma of the right colon. Br J Surg. 1993;80:1327–9.
Gort M, Otter R, Plukker JT, Broekhuis M, Klazinga NS. Actionable indicators for short and long term outcomes in rectal cancer. Eur J Cancer. 2010;46:1808–14.
Graffner H, Olsson SA. Patient’s and doctor’s delay in carcinoma of the colon and rectum. J Surg Oncol. 1986;31:188–90.
Grass F, Behm KT, Duchalais E, Crippa J, Spears GM, Harmsen WS, et al. Impact of delay to surgery on survival in stage I-III colon cancer. Eur J Surg Oncol. 2020;46:455–61.
Guzmán Laura KP, Bolíbar Ribas I, Alepuz MT, González D, Martín M. Impact on patient care time and tumor stage of a program for fast diagnostic and treatment of colorectal cancer. Rev Esp Enferm Dig. 2011;103:13–9.
Hafström L, Johansson H, Ahlberg J. Does diagnostic delay of colorectal cancer result in malpractice claims? A retrospective analysis of the Swedish board of malpractice from 1995-2008. Patient Saf Surg. 2012;6:13.
Helewa RM, Turner D, Park J, Wirtzfeld D, Czaykowski P, Hochman D, et al. Longer waiting times for patients undergoing colorectal cancer surgery are not associated with decreased survival. J Surg Oncol. 2013;108:378–84.
Holliday HW, Hardcastle JD. Delay in diagnosis and treatment of symptomatic colorectal cancer. Lancet. 1979;1:309–11.
Irvin TT, Greaney MG. Duration of symptoms and prognosis of carcinoma of the colon and rectum. Surg, Gynecol Obstet. 1977;144:883–6.
Iversen LH, Antonsen S, Laurberg S, Lautrup MD. Therapeutic delay reduces survival of rectal cancer but not of colonic cancer. Br J Surg. 2009;96:1183–9.
Janssen RM, Takach O, Nap-Hill E, Enns RA. Time to endoscopy in patients with colorectal cancer: analysis of wait-times. Can J Gastroenterol Hepatol. 2016;2016:8714587.
Järvinen HJ, Turunen MJ. Colorectal carcinoma before 40 years of age: prognosis and predisposing conditions. Scand J Gastroenterol. 1984;19:634–8.
Jolly KD, Scott JP, MacKinnon MJ, Clarke AM. Diagnosis and survival in carcinoma of the large bowel. Aust NZ J Surg. 1982;52:12–6.
Jullumstrø E, Lydersen S, Møller B, Dahl O, Edna TH. Duration of symptoms, stage at diagnosis and relative survival in colon and rectal cancer. Eur J Cancer. 2009;45:2383–90.
Keddie N, Hargreaves A. Symptoms of carcinoma of the colon and rectum. Lancet. 1968;2:749–50.
Khattak I, Eardley NJ, Rooney PS. Colorectal cancer–a prospective evaluation of symptom duration and GP referral patterns in an inner city teaching hospital. Colorectal Dis. 2006;8:518–21.
Khorana AA, Tullio K, Elson P, Pennell NA, Grobmyer SR, Kalady MF, et al. Time to initial cancer treatment in the United States and association with survival over time: an observational study. PLoS ONE. 2019;14:e0213209.
Khubchandani M. Relationship of symptom duration and survival in patients with carcinoma of the colon and rectum. Dis Colon Rectum. 1985;28:585–7.
Kim TJ, Kim ER, Hong SN, Chang DK, Kim YH. Long-term outcome and prognostic factors of sporadic colorectal cancer in young patients: a large institutional-based retrospective study. Medicine 2016;95:e3641.
Kiran PR, Glass RE. Duration of symptoms and spread of colorectal cancer: a short history does not mean early disease. Ann R Coll Surg Engl. 2002;84:381–5.
Korsgaard M, Pedersen L, Sørensen HT, Laurberg S. Delay of treatment is associated with advanced stage of rectal cancer but not of colon cancer. Cancer Detect Prev. 2006;30:341–6.
Kucejko RJ, Holleran TJ, Stein DE, Poggio JL. How soon should patients with colon cancer undergo definitive resection? Dis Colon Rectum. 2020;63:172–82.
Kyle SM, Isbister WH, Yeong ML. Presentation, duration of symptoms and staging of colorectal carcinoma. Aust NZ J Surg. 1991;61:137–40.
Langenbach MR, Sauerland S, Kröbel KW, Zirngibl H. Why so late?!–delay in treatment of colorectal cancer is socially determined. Langenbeck’s Arch Surg. 2010;395:1017–24.
Langenbach MR, Schmidt J, Neumann J, Zirngibl H. Delay in treatment of colorectal cancer: multifactorial problem. World J Surg. 2003;27:304–8.
Law CW, Roslani AC, Ng LL. Treatment delay in rectal cancer. Med J Malays. 2009;64:163–5.
Lee YH, Kung PT, Wang YH, Kuo WY, Kao SL, Tsai WC. Effect of length of time from diagnosis to treatment on colorectal cancer survival: a population-based study. PLoS ONE. 2019;14:e0210465.
Leiva A, Esteva M, Llobera J, Macià F, Pita-Fernández S, González-Luján L, et al. Time to diagnosis and stage of symptomatic colorectal cancer determined by three different sources of information: a population based retrospective study. Cancer Epidemiol. 2017;47:48–55.
Lim BS, Dennis CR, Gardner B, Newman J. Analysis of survival versus patient and doctor delay of treatment in gastrointestinal cancer. Am J Surg. 1974;127:210–4.
Lino-Silva LS, Guzmán-López JC, Zepeda-Najar C, Salcedo-Hernández RA, Meneses-García A. Overall survival of patients with colon cancer and a prolonged time to surgery. J Surg Oncol. 2019;119:503–9.
MacArthur C, Smith A. Factors associated with speed of diagnosis, referral, and treatment in colorectal cancer. J Epidemiol Commun Health 1984;38:122–6.
Maguire A, Porta M, Malats N, Gallén M, Piñol JL, Fernandez E. Cancer survival and the duration of symptoms. An analysis of possible forms of the risk function. ISDS II Project Investigators. Eur J Cancer. 1994;30a:785–92.
Majumdar SR, Fletcher RH, Evans AT. How does colorectal cancer present? Symptoms, duration, and clues to location. Am J Gastroenterol. 1999;94:3039–45.
Marble K, Banerjee S, Greenwald L. Colorectal carcinoma in young patients. J Surg Oncol. 1992;51:179–82.
McDermott F, Hughes E, Pihl E, Milne BJ, Price A. Symptom duration and survival prospects in carcinoma of the rectum. Surg Gynecol Obstet. 1981;153:321–6.
McDermott FT, Hughes ES, Pihl E, Milne BJ, Price AB. Prognosis in relation to symptom duration in colon cancer. Br J Surg. 1981;68:846–9.
Mulcahy H, O’Donoghue D. Duration of colorectal cancer symptoms and survival: the effect of confounding clinical and pathological variables. Eur J Cancer. 1997;33:1461–7.
Murchie P, Raja EA, Brewster DH, Campbell NC, Ritchie LD, Robertson R, et al. Time from first presentation in primary care to treatment of symptomatic colorectal cancer: effect on disease stage and survival. Br J Cancer. 2014;111:461–9.
Nilsson E, Bolin S, Sjödahl R. Carcinoma of the colon and rectum. Delay in diagnosis. Acta Chir Scand. 1982;148:617–22.
Olsson L, Bergkvist L, Ekbom A. Symptom duration versus survival in non-emergency colorectal cancer. Scand J Gastroenterol. 2004;39:252–8.
Ortiz-Ortiz KJ, Ríos-Motta R, Marín-Centeno H, Cruz-Correa M, Ortiz AP. Factors associated with late stage at diagnosis among Puerto Rico’s government health plan colorectal cancer patients: a cross-sectional study. BMC Health Serv Res. 2016;16:1–10.
Öztürk E, Kuzu MA, Öztuna D, Işık Ö, Canda AE, Balık E, et al. Fall of another myth for colon cancer: duration of symptoms does not differ between right- or left-sided colon cancers. Turk J Gastroenterol. 2019;30:686–94.
Påhlman L, Glimelius B, Enblad P. Clinical characteristics and their relation to surgical curability in adenocarcinoma of the rectum and rectosigmoid. A population-based study on 279 consecutive patients. Acta Chir Scand. 1985;151:685–93.
Patel R, Anderson JE, McKenzie C, Simpson M, Singh N, Ruzvidzo F, et al. Compliance with the 62-day target does not improve long-term survival. Int J Colorectal Dis. 2018;33:65–9.
Pearson C, Fraser J, Peake M, Valori R, Poirier V, Coupland VH, et al. Establishing population-based surveillance of diagnostic timeliness using linked cancer registry and administrative data for patients with colorectal and lung cancer. Cancer Epidemiol. 2019;61:111–8.
Pescatori M, Maria G, Beltrani B, Mattana C. Site, emergency, and duration of symptoms in the prognosis of colorectal cancer. Dis Colon Rectum. 1982;25:33–40.
Pita-Fernández S, González-Sáez L, López-Calviño B, Seoane-Pillado T, Rodríguez-Camacho E, Pazos-Sierra A, et al. Effect of diagnostic delay on survival in patients with colorectal cancer: a retrospective cohort study. BMC Cancer. 2016;16:664.
Polissar L, Sim D, Francis A. Survival of colorectal cancer patients in relation to duration of symptoms and other prognostic factors. Dis Colon Rectum. 1981;24:364–9.
Porta M, Gallén M, Malats N, Planas J. Influence of "diagnostic delay" upon cancer survival: an analysis of five tumour sites. J Epidemiol Commun Health 1991;45:225–30.
Porter GA, Inglis KM, Wood LA, Veugelers PJ. Access to care and satisfaction in colorectal cancer patients. World J Surg. 2005;29:1444–51.
Pruitt SL, Harzke AJ, Davidson NO, Schootman M. Do diagnostic and treatment delays for colorectal cancer increase risk of death? Cancer Causes Control. 2013;24:961–77.
Ratcliffe R, Kiff RS, Hoare EM, Kingston RD, Walsh SH, Jeacock J. Early diagnosis in colorectal cancer still no benefit? Ann Chir. 1989;43:570–4.
Redaniel MT, Martin RM, Ridd MJ, Wade J, Jeffreys M. Diagnostic intervals and its association with breast, prostate, lung and colorectal cancer survival in England: historical cohort study using the Clinical Practice Research Datalink. PLoS ONE. 2015;10:e0126608.
Ristvedt SL, Birnbaum EH, Dietz DW, Fleshman JW, Kodner IJ, Read TE. Delayed treatment for rectal cancer. Dis colon rectum. 2005;48:1736–41.
Robinson E, Mohilever J, Zidan J, Sapir D. Colorectal cancer: incidence, delay in diagnosis and stage of disease. Eur J Cancer Clin Oncol. 1986;22:157–61.
Roder D, Karapetis CS, Olver I, Keefe D, Padbury R, Moore J, et al. Time from diagnosis to treatment of colorectal cancer in a South Australian clinical registry cohort: how it varies and relates to survival. BMJ Open. 2019;9:e031421.
Roland CL, Schwarz RE, Tong L, Ahn C, Balch GC, Yopp AC, et al. Is timing to delivery of treatment a reliable measure of quality of care for patients with colorectal adenocarcinoma? Surgery. 2013;154:421–8.
Roncoroni L, Pietra N, Violi V, Sarli L, Choua O, Peracchia A. Delay in the diagnosis and outcome of colorectal cancer: a prospective study. Eur J Surg Oncol. 1999;25:173–8.
Rowejones DC, Aylett SO. Delay in treatment in carcinoma of colon and rectum. Lancet. 1965;2:973–6.
Rubin M, Zer M, Dintsman M. Factors influencing delay in treatment of cancer of rectum and colon in Israel. Isr J Med Sci. 1980;16:641–5.
Sandar M, Hsiang LG, Yew CK, Guat LB. Use of population-based cancer registry data to determine the effect of timely treatment on the survival of colorectal cancer patients. J Registry Manag. 2015;42:130–8.
Sey MS, Gregor J, Adams P, Khanna N, Vinden C, Driman D, et al. Wait times for diagnostic colonoscopy among outpatients with colorectal cancer: a comparison with Canadian Association of Gastroenterology targets. Can J Gastroenterol. 2012;26:894–6.
Shin DW, Cho J, Kim SY, Guallar E, Hwang SS, Cho B, et al. Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol. 2013;20:2468–76.
Simunovic M, Rempel E, Thériault ME, Baxter NN, Virnig BA, Meropol NJ, et al. Influence of delays to nonemergent colon cancer surgery on operative mortality, disease-specific survival and overall survival. Can J Surg. 2009;52:E79–e86.
Singh H, Shu E, Demers A, Bernstein CN, Griffith J, Fradette K. Trends in time to diagnosis of colon cancer and impact on clinical outcomes. Can J Gastroenterol. 2012;26:877–80.
Stapley S, Peters TJ, Sharp D, Hamilton W. The mortality of colorectal cancer in relation to the initial symptom at presentation to primary care and to the duration of symptoms: a cohort study using medical records. Br J Cancer. 2006;95:1321–5.
Strous MTA, Janssen-Heijnen MLG, Vogelaar FJ. Impact of therapeutic delay in colorectal cancer on overall survival and cancer recurrence - is there a safe timeframe for prehabilitation? Eur J Surg Oncol. 2019;45:2295–301.
Stubbs RS, Long MG. Symptom duration and pathologic staging of colorectal cancer. Eur J Surg Oncol. 1986;12:127–30.
Terhaar sive Droste JS, Oort FA, van der Hulst RW, Coupé VM, Craanen ME, Meijer GA, et al. Does delay in diagnosing colorectal cancer in symptomatic patients affect tumor stage and survival? A population-based observational study. BMC Cancer. 2010;10:332.
Thompson MR, Asiimwe A, Flashman K, Tsavellas G. Is earlier referral and investigation of bowel cancer patients presenting with rectal bleeding associated with better survival? Colorectal Dis. 2011;13:1242–8.
Tiong J, Gray A, Jackson C, Thompson-Fawcett M, Schultz M. Audit of the association between length of time spent on diagnostic work-up and tumour stage in patients with symptomatic colon cancer. ANZ J Surg. 2017;87:138–42.
Tørring ML, Falborg AZ, Jensen H, Neal RD, Weller D, Reguilon I, et al. Advanced-stage cancer and time to diagnosis: an International Cancer Benchmarking Partnership (ICBP) cross-sectional study. Eur J Cancer Care. 2019;28:e13100.
Tørring ML, Frydenberg M, Hansen RP, Olesen F, Hamilton W, Vedsted P. Time to diagnosis and mortality in colorectal cancer: a cohort study in primary care. Br J Cancer. 2011;104:934–40.
Tørring ML, Frydenberg M, Hansen RP, Olesen F, Vedsted P. Evidence of increasing mortality with longer diagnostic intervals for five common cancers: a cohort study in primary care. Eur J Cancer. 2013;49:2187–98.
Tørring ML, Murchie P, Hamilton W, Vedsted P, Esteva M, Lautrup M, et al. Evidence of advanced stage colorectal cancer with longer diagnostic intervals: a pooled analysis of seven primary care cohorts comprising 11720 patients in five countries. Br J Cancer. 2017;117:888–97.
Trepanier M, Paradis T, Kouyoumdjian A, Dumitra T, Charlebois P, Stein BS, et al. The impact of delays to definitive surgical care on survival in colorectal cancer patients. J Gastrointest Surg. 2020;24:115–22.
Turnbull PR, Isbister WH. Colorectal cancer in New Zealand: a Wellington study. Aust NZ J Surg. 1979;49:45–8.
Turunen MJ, Peltokallio P. Delay in the diagnosis of colorectal cancer. Ann Chir Gynaecol. 1982;71:277–82.
Van Hout AM, de Wit NJ, Rutten FH, Peeters PH. Determinants of patient’s and doctor’s delay in diagnosis and treatment of colorectal cancer. Eur J Gastroenterol Hepatol. 2011;23:1056–63.
Viiala CH, Tang KW, Lawrance IC, Murray K, Olynyk JK. Waiting times for colonoscopy and colorectal cancer diagnosis. Med J Aust. 2007;186:282–5.
Walming S, Block M, Bock D, Angenete E. Timely access to care in the treatment of rectal cancer and the effect on quality of life. Colorectal Dis. 2018;20:126–33.
Wanis KN, Patel SVB, Brackstone M. Do moderate surgical treatment delays influence survival in colon cancer? Dis Colon Rectum. 2017;60:1241–9.
Wattacheril J, Kramer JR, Richardson P, Havemann BD, Green LK, Le A, et al. Lagtimes in diagnosis and treatment of colorectal cancer: determinants and association with cancer stage and survival. Aliment Pharmacol Ther. 2008;28:1166–74.
Wheeler, Wakefield, Mortensen NJMcC, Kettlewell. Delays experienced by patients with symptomatic colorectal cancer. Colorectal Dis. 1999;1:174–6.
Young CJ, Sweeney JL, Hunter A. Implications of delayed diagnosis in colorectal cancer. Aust NZ J Surg. 2000;70:635–8.
Yun YH, Kim YA, Min YH, Park S, Won YJ, Kim DY, et al. The influence of hospital volume and surgical treatment delay on long-term survival after cancer surgery. Ann Oncol. 2012;23:2731–7.
Zhang JK, Fang LL, Wu XM, Liu JC, Zhang CD, Dai DQ. Factors associated with delaying medical assessment of patients and impacting the prognosis of rectal cancer. Eur J Cancer Prev 2015;24:391–9.
Burke JR, Brown P, Quyn A, Lambie H, Tolan D, Sagar P. Tumour growth rate of carcinoma of the colon and rectum: retrospective cohort study. BJS Open. 2020;4:1200–7.
Ng J, Stovezky YR, Brenner DJ, Formenti SC, Shuryak I. Development of a model to estimate the association between delay in cancer treatment and local tumor control and risk of metastases. JAMA Netw Open. 2021;4:e2034065.
Cohen J. The cost of dichotomization. Appl Psychol Meas. 1983;7:249–53.
Royston P, Altman DG, Sauerbrei W. Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med. 2006;25:127–41.
Petrova D, Špacírová Z, Fernández-Martínez NF, Ching-López A, Garrido D, Rodríguez-Barranco M, et al. The patient, diagnostic, and treatment intervals in adult patients with cancer from high- and lower-income countries: a systematic review and meta-analysis. PLoS Med. 2022;19:e1004110.
Siciliani L, Moran V, Borowitz M. What works? Waiting policies in the health sector. Eurohealth Observer. 2015;21:14–7.
Australian Government Department of Health. Optimal cancer care pathways. Canberra: Commonwealth of Australia; 2016.
Funding
AD is supported by a NHMRC Postgraduate Scholarship. RJB is supported by a Victorian Cancer Agency, Early Career Research Fellowship (ECRF20015).
Author information
Authors and Affiliations
Contributions
All authors have significantly contributed to the conceptualisation, design, conduct and reporting (writing and reviewing) of this systematic review.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethics approval was not required for this review.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Drosdowsky, A., Lamb, K.E., Karahalios, A. et al. The effect of time before diagnosis and treatment on colorectal cancer outcomes: systematic review and dose–response meta-analysis. Br J Cancer 129, 993–1006 (2023). https://doi.org/10.1038/s41416-023-02377-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02377-w
