Abstract
Background
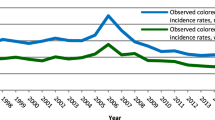
Combining the faecal immunochemical test (FIT) result with risk factors for advanced neoplasia (AN) may increase the yield of colorectal cancer (CRC) screening without increasing the number of colonoscopies. We conducted a randomised controlled trial in the Dutch CRC screening programme to evaluate a previously developed risk model including FIT, age, sex, smoking status, and CRC family history.
Methods
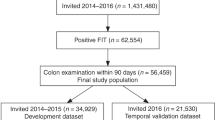
A total of 22,748 individuals aged 56–75 years were pre-randomised to the risk-model group or the FIT-only group. Both groups received the FIT; those allocated to the risk-model group also received a single-page questionnaire. Study participants with a positive result (FIT ≥ 15 µg Hb/g faeces and/or risk ≥0.10) were referred for colonoscopy. The primary outcome measure was the proportion of invitees in whom AN was detected.
Results
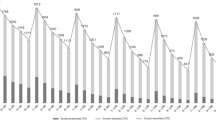
In the risk-model group, 3113/11,364 invitees (27%) returned the FIT and questionnaire versus 3061/11,384 invitees (27%) in the FIT-only group (p = 0.40). The yield of AN was 3.70/1000 invitees in the risk-model group versus 3.43/1000 in the FIT-only group (absolute difference: 0.27/1000, 95%CI: −1.30 to 1.82, p = 0.82).
Conclusions
Combining FIT with risk factors for CRC did not increase the yield of AN compared to FIT-only in an existing CRC screening programme. There was no difference in participation between groups.
Clinical trial registration
NCT04490551 (ClinicalTrials.gov).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Study data cannot be shared publicly, but access can be requested via the Netherlands Institute of Public Health and the Environment (RIVM). Analytic methods can be shared by the authors on request.
References
Levin TR, Corley DA, Jensen CD, Schottinger JE, Quinn VP, Zauber AG, et al. Effects of organized colorectal cancer screening on cancer incidence and mortality in a large community-based population. Gastroenterology. 2018;155:1383–91.e1385.
Zauber AG, Winawer SJ, O'Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366:687–96.
Schreuders EH, Ruco A, Rabeneck L, Schoen RE, Sung JJ, Young GP, et al. Colorectal cancer screening: a global overview of existing programmes. Gut. 2015;64:1637–49.
Gies A, Cuk K, Schrotz-King P, Brenner H. Direct comparison of diagnostic performance of 9 quantitative fecal immunochemical tests for colorectal cancer screening. Gastroenterology. 2018;154:93–104.
Wieten E, de Klerk CM, van der Steen A, Ramakers CR, Kuipers EJ, Hansen BE, et al. Equivalent accuracy of 2 quantitative fecal immunochemical tests in detecting advanced neoplasia in an organized colorectal cancer screening program. Gastroenterology. 2018;155:1392–9.e1395.
Stegeman I, de Wijkerslooth TR, Stoop EM, van Leerdam ME, Dekker E, van Ballegooijen M, et al. Combining risk factors with faecal immunochemical test outcome for selecting CRC screenees for colonoscopy. Gut. 2014;63:466–71.
Cooper JA, Parsons N, Stinton C, Mathews C, Smith S, Halloran SP, et al. Risk-adjusted colorectal cancer screening using the FIT and routine screening data: development of a risk prediction model. Br J Cancer. 2018;118:285–93.
Park CH, Jung YS, Kim NH, Park JH, Park DI, Sohn CI. Usefulness of risk stratification models for colorectal cancer based on fecal hemoglobin concentration and clinical risk factors. Gastrointest Endosc. 2019;89:1204–11.e1201.
Kaminski MF, Polkowski M, Kraszewska E, Rupinski M, Butruk E, Regula J. A score to estimate the likelihood of detecting advanced colorectal neoplasia at colonoscopy. Gut. 2014;63:1112–9.
National Institute for Public Health and the Environment (RIVM). National monitoring colorectal cancer screening programme 2020. https://www.rivm.nl/sites/default/files/2021-10/Monitor_bevolkingsonderzoek_darmkanker_2020_eng.pdf. Accessed 21 February 2022.
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332.
Grobbee EJ, Wieten E, Hansen BE, Stoop EM, de Wijkerslooth TR, Lansdorp-Vogelaar I, et al. Fecal immunochemical test-based colorectal cancer screening: the gender dilemma. U Eur Gastroenterol J. 2017;5:448–54.
Toll DB, Janssen KJM, Vergouwe Y, Moons KGM. Validation, updating and impact of clinical prediction rules: a review. J Clin Epidemiol. 2008;61:1085–94.
Bronzwaer MES, Depla A, van Lelyveld N, Spanier BWM, Oosterhout YH, van Leerdam ME, et al. Quality assurance of colonoscopy within the Dutch national colorectal cancer screening program. Gastrointest Endosc. 2019;89:1–13.
Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, et al. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76:182–8.
Schlemper RJ, Riddell RH, Kato Y, Borchard F, Cooper HS, Dawsey SM, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000;47:251–5.
Zorzi M, Hassan C, Capodaglio G, Narne E, Turrin A, Baracco M, et al. Divergent long-term detection rates of proximal and distal advanced neoplasia in fecal immunochemical test screening programs. Ann Intern Med. 2018;169:602–9.
Haug U, Kuntz KM, Knudsen AB, Hundt S, Brenner H. Sensitivity of immunochemical faecal occult blood testing for detecting left- vs right-sided colorectal neoplasia. Br J Cancer. 2011;104:1779–85.
R Core Team. R: a language and environment for statistical computing. v. 4.0.3. R Foundation for Statistical Computing, Vienna, Austria. 2021.
Kuipers EJ, Spaander MC. Personalized screening for colorectal cancer. Nat Rev Gastroenterol Hepatol. 2018;15:391–2.
Chen H, Lu M, Liu C, Zou S, Du L, Liao X, et al. Comparative evaluation of participation and diagnostic yield of colonoscopy vs fecal immunochemical test vs risk-adapted screening in colorectal cancer screening: interim analysis of a multicenter randomized controlled trial (TARGET-C). Am J Gastroenterol. 2020;115:1264–74.
Central Statistical Bureau (CBS). [Smoking status of adults by demographic characteristics, 2019]. https://www.cbs.nl/nl-nl/maatwerk/2020/51/rookstatus-volwassenen-naar-achtergrondkenmerken-2019. Accessed 6 December 2021.
Babyak MA. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom Med. 2004;66:411–21.
Chiu H-M, Ching JYL, Wu KC, Rerknimitr R, Li J, Wu D-C, et al. A risk-scoring system combined with a fecal immunochemical test is effective in screening high-risk subjects for early colonoscopy to detect advanced colorectal neoplasms. Gastroenterology. 2016;150:617–25.e613.
Liu F, Long Q, He H, Dong S, Zhao L, Zou C, et al. Combining the fecal immunochemical test with a logistic regression model for screening colorectal neoplasia. Front Pharmacol. 2021;12:635481.
Chen LS, Yen AM, Chiu SY, Liao CS, Chen HH. Baseline faecal occult blood concentration as a predictor of incident colorectal neoplasia: longitudinal follow-up of a Taiwanese population-based colorectal cancer screening cohort. Lancet Oncol. 2011;12:551–8.
Grobbee EJ, Schreuders EH, Hansen BE, Bruno MJ, Lansdorp-Vogelaar I, Spaander MCW, et al. Association between concentrations of hemoglobin determined by fecal immunochemical tests and long-term development of advanced colorectal neoplasia. Gastroenterology. 2017;153:1251–9.e1252.
Senore C, Zappa M, Campari C, Crotta S, Armaroli P, Arrigoni A, et al. Faecal haemoglobin concentration among subjects with negative FIT results is associated with the detection rate of neoplasia at subsequent rounds: a prospective study in the context of population based screening programmes in Italy. Gut. 2020;69:523–30.
Breekveldt ECH, Toes-Zoutendijk E, de Jonge L, Spaander MCW, Dekker E, van Kemenade FJ, et al. Personalized colorectal cancer screening: study protocol of a mixed-methods study on the effectiveness of tailored intervals based on prior f-Hb concentration in a fit-based colorectal cancer screening program (PERFECT-FIT). BMC Gastroenterol. 2023;23:45.
Acknowledgements
We would like to express our gratitude to the Foundation of Population Screening Mid-West Netherlands, in particular to Erwin Humer, Maja Groothuis, and Toos Portegies–te Brake, for their effort in enabling this study to be carried out. We also like to thank Frejanne van Maaren–Meijer for her assistance in data acquisition. Third, we would like to thank all staff of the endoscopy unit of Bergman Clinics, location IZA, and in particular, Mariska Rustenburg.
Funding
This study was supported by the Netherlands Organisation for Health Research and Development (ZonMw). ZonMw had no role in the study design; data collection, analysis, or interpretation; in the writing of the report, and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
ED, PB, and MV conceived and designed this study. AM, ILV, MS, and RK participated in meetings discussing the design of the study. TK enrolled participants and collected the data. ED, PB, and MV supervised the study and data collection. TK, PB, ED, and MV contributed to data analysis and interpretation. TK drafted the manuscript. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. TK and PB accessed and verified the data.
Corresponding author
Ethics declarations
Competing interests
AM received financial support from Pentax Europe. MS received material and financial support from Sentinel, Sysmex, and Medtronic. ED received endoscopic equipment on loan from FujiFilm and Olympus, received a research grant from FujiFilm, received honorarium for consultancy from FujiFilm, Olympus, GI Supply, CPP-FAP, PAION, and Ambu, and speakers’ fees from Olympus, GI Supply, Norgine, IPSEN, PAION, and FujiFilm. The remaining authors disclose no conflicts.
Ethics approval and consent to participate
This study was approved by the Dutch Health Council according to the law on population screening. Written informed consent was required for study enrolment. The study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kortlever, T.L., van der Vlugt, M., Duijkers, F.A.M. et al. Diagnostic yield of a risk model versus faecal immunochemical test only: a randomised controlled trial in a colorectal cancer screening programme. Br J Cancer 129, 791–796 (2023). https://doi.org/10.1038/s41416-023-02358-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02358-z