Abstract
Background
Long-term prognosis remains poor for colorectal cancer (CRC) patients with advanced disease due to treatment resistance. The identification of novel targets is essential for the development of new therapeutic approaches. GPR56, an adhesion GPCR, is highly expressed in CRC tumours and correlates with poor survival. Here, we describe the generation and preclinical evaluation of a novel ADC consisting of an anti-GPR56 antibody (10C7) conjugated with the DNA-damaging payload duocarmycin.
Methods
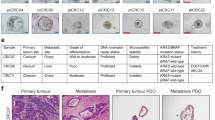
RNA-seq dataset analysis was performed to determine GPR56 expression in CRC subtypes. The specificity of binding, epitope mapping, and internalisation of 10C7 was examined. 10C7 was conjugated to payload and ADC cytotoxicity was assessed against a panel of CRC cell lines and tumour organoids. Antitumour efficacy was evaluated in xenograft models of CRC cell lines and patient-derived tumours.
Results
High GPR56 was shown to be associated with the microsatellite stable (MSS) subtype that accounts for 80–85% of CRC. GPR56 ADC selectively induced cytotoxicity in CRC cells and tumour organoids at low nanomolar potency in a GPR56-dependent manner and showed significant antitumour efficacy against GPR56-expressing xenograft models.
Conclusions
This study provides the rationale for the future development of a GPR56-targeted ADC approach to potentially treat a large fraction of MSS CRC patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this article and its supplementary information files.
References
Society AC. Cancer Facts & Figures 2021. Atlanta, GA: American Cancer Society; 2021.
Xie YH, Chen YX, Fang JY. Comprehensive review of targeted therapy for colorectal cancer. Signal Transduct Target Ther. 2020;5:22.
Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med. 2015;372:2509–20.
Fu Z, Li S, Han S, Shi C, Zhang Y. Antibody drug conjugate: the “biological missile” for targeted cancer therapy. Signal Transduct Target Ther. 2022;7:93.
Leal M, Sapra P, Hurvitz SA, Senter P, Wahl A, Schutten M, et al. Antibody-drug conjugates: an emerging modality for the treatment of cancer. Ann N Y Acad Sci. 2014;1321:41–54.
Teicher BA. Antibody drug conjugates. Curr Opin Oncol. 2014;26:476–83.
Beck A, Goetsch L, Dumontet C, Corvaia N. Strategies and challenges for the next generation of antibody-drug conjugates. Nat Rev Drug Discov. 2017;16:315–37.
Ke N, Sundaram R, Liu G, Chionis J, Fan W, Rogers C, et al. Orphan G protein-coupled receptor GPR56 plays a role in cell transformation and tumorigenesis involving the cell adhesion pathway. Mol Cancer Ther. 2007;6:1840–50.
Liu Z, Huang Z, Yang W, Li Z, Xing S, Li H, et al. Expression of orphan GPR56 correlates with tumor progression in human epithelial ovarian cancer. Neoplasma. 2016;64:32–9.
Sewda K, Coppola D, Enkemann S, Yue B, Kim J, Lopez AS, et al. Cell-surface markers for colon adenoma and adenocarcinoma. Oncotarget. 2016;7:17773–89.
Zhang S, Chatterjee T, Godoy C, Wu L, Liu QJ, Carmon KS. GPR56 drives colorectal tumor growth and promotes drug resistance through upregulation of MDR1 expression via a RhoA-mediated mechanism. Mol Cancer Res. 2019;17:2196–207.
Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal. 2013;6:pl1.
Haitina T, Olsson F, Stephansson O, Alsio J, Roman E, Ebendal T, et al. Expression profile of the entire family of adhesion G protein-coupled receptors in mouse and rat. BMC Neurosci. 2008;9:43.
Kaiser F, Morawski M, Krohn K, Rayes N, Hsiao CC, Quaas M, et al. Adhesion GPCR GPR56 expression profiling in human tissues. Cells. 2021;10:3557.
Shashidhar S, Lorente G, Nagavarapu U, Nelson A, Kuo J, Cummins J, et al. GPR56 is a GPCR that is overexpressed in gliomas and functions in tumor cell adhesion. Oncogene. 2005;24:1673–82.
Ji B, Feng Y, Sun Y, Ji D, Qian W, Zhang Z, et al. GPR56 promotes proliferation of colorectal cancer cells and enhances metastasis via epithelialmesenchymal transition through PI3K/AKT signaling activation. Oncol Rep. 2018;40:1885–96.
Jin G, Sakitani K, Wang H, Jin Y, Dubeykovskiy A, Worthley DL, et al. The G-protein coupled receptor 56, expressed in colonic stem and cancer cells, binds progastrin to promote proliferation and carcinogenesis. Oncotarget. 2017;8:40606–19.
Chatterjee T, Zhang S, Posey TA, Jacob J, Wu L, Yu W, et al. Anti-GPR56 monoclonal antibody potentiates GPR56-mediated Src-Fak signaling to modulate cell adhesion. J Biol Chem. 2021;296:100261.
Gong X, Azhdarinia A, Ghosh SC, Xiong W, An Z, Liu Q, et al. LGR5-targeted antibody-drug conjugate eradicates gastrointestinal tumors and prevents recurrence. Mol Cancer Ther. 2016;15:1580–90.
Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, Aksoy BA, et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401–4.
Cancer Genome Atlas N. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–7.
Ghandi M, Huang FW, Jane-Valbuena J, Kryukov GV, Lo CC, McDonald ER 3rd, et al. Next-generation characterization of the Cancer Cell Line Encyclopedia. Nature. 2019;569:503–8.
Berg KCG, Eide PW, Eilertsen IA, Johannessen B, Bruun J, Danielsen SA, et al. Multi-omics of 34 colorectal cancer cell lines—a resource for biomedical studies. Mol Cancer. 2017;16:116.
Ahmed D, Eide PW, Eilertsen IA, Danielsen SA, Eknaes M, Hektoen M, et al. Epigenetic and genetic features of 24 colon cancer cell lines. Oncogenesis. 2013;2:e71.
Nejadmoghaddam MR, Minai-Tehrani A, Ghahremanzadeh R, Mahmoudi M, Dinarvand R, Zarnani AH. Antibody-drug conjugates: possibilities and challenges. Avicenna J Med Biotechnol. 2019;11:3–23.
Biller LH, Schrag D. Diagnosis and treatment of metastatic colorectal cancer: a review. J Am Med Assoc. 2021;325:669–85.
Le DT, Durham JN, Smith KN, Wang H, Bartlett BR, Aulakh LK, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357:409–13.
Tolcher AW. Antibody drug conjugates: lessons from 20 years of clinical experience. Ann Oncol. 2016;27:2168–72.
Nadal-Serrano M, Morancho B, Escriva-de-Romani S, Morales CB, Luque A, Escorihuela M, et al. The second generation antibody-drug conjugate SYD985 overcomes resistances to T-DM1. Cancers. 2020;12:670.
Jukes Z, Morais GR, Loadman PM, Pors K. How can the potential of the duocarmycins be unlocked for cancer therapy? Drug Discov Today. 2021;26:577–84.
Powderly JD, Jang S, Lohr J, Spira AI, Bohac GC, Sharma M. Preliminary dose escalation results from a phase I/II, first-in-human study of MGC018 (anti-B7-H3 antibody-drug conjugate) in patients with advanced solid tumors. J Clin Oncol. 2020;38:3071.
Banerji U, van Herpen CML, Saura C, Thistlethwaite F, Lord S, Moreno V, et al. Trastuzumab duocarmazine in locally advanced and metastatic solid tumours and HER2-expressing breast cancer: a phase 1 dose-escalation and dose-expansion study. Lancet Oncol. 2019;20:1124–35.
Liao MZ, Lu D, Kagedal M, Miles D, Samineni D, Liu SN, et al. Model-informed therapeutic dose optimization strategies for antibody-drug conjugates in oncology: what can we learn from US Food and Drug Administration-approved antibody-drug conjugates? Clin Pharm Ther. 2021;110:1216–30.
Caimi PF, Ai W, Alderuccio JP, Ardeshna KM, Hamadani M, Hess B, et al. Loncastuximab tesirine in relapsed or refractory diffuse large B-cell lymphoma (LOTIS-2): a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2021;22:790–800.
Banks WA. From blood-brain barrier to blood-brain interface: new opportunities for CNS drug delivery. Nat Rev Drug Discov. 2016;15:275–92.
Stepan LP, Trueblood ES, Hale K, Babcook J, Borges L, Sutherland CL. Expression of Trop2 cell surface glycoprotein in normal and tumor tissues: potential implications as a cancer therapeutic target. J Histochem Cytochem. 2011;59:701–10.
Peng YM, van de Garde MD, Cheng KF, Baars PA, Remmerswaal EB, van Lier RA, et al. Specific expression of GPR56 by human cytotoxic lymphocytes. J Leukoc Biol. 2011;90:735–40.
Chang GW, Hsiao CC, Peng YM, Vieira Braga FA, Kragten NA, Remmerswaal EB, et al. The adhesion G protein-coupled receptor GPR56/ADGRG1 is an inhibitory receptor on human NK cells. Cell Rep. 2016;15:1757–70.
Langenhan T, Aust G, Hamann J. Sticky signaling—adhesion class G protein-coupled receptors take the stage. Sci Signal. 2013;6:re3.
Arac D, Boucard AA, Bolliger MF, Nguyen J, Soltis SM, Sudhof TC, et al. A novel evolutionarily conserved domain of cell-adhesion GPCRs mediates autoproteolysis. EMBO J. 2012;31:1364–78.
Daria D, Kirsten N, Muranyi A, Mulaw M, Ihme S, Kechter A, et al. GPR56 contributes to the development of acute myeloid leukemia in mice. Leukemia. 2016;30:1734–41.
Pabst C, Bergeron A, Lavallee VP, Yeh J, Gendron P, Norddahl GL, et al. GPR56 identifies primary human acute myeloid leukemia cells with high repopulating potential in vivo. Blood. 2016;127:2018–27.
Acknowledgements
We would like to thank Sheng Zhang and Wangsheng Yu for technical contributions, Betty Arceneaux and Dr. Karan Saluja with assistance in patient sample collection and processing, and Martha Thompson for assistance with regulatory approvals for research involving human subjects.
Funding
This work was supported by funding from the National Institutes of Health (NCI R01 CA226894) and Welch Foundation Endowment Fund Award (L-AU-0002-19940421) to KSC, funding from the Cancer Prevention and Research Institute of Texas (RP190542) to QJL and KSC, a fellowship of the Gulf Coast Consortia, on the Training Interdisciplinary Pharmacology Scientists Program (T32 GM139801) to JJ, and a Cancer Therapeutics Training Program Fellowship (RP210043) to LEF.
Author information
Authors and Affiliations
Contributions
Conceptualisation and design: KSC; methodology: KSC; investigation: KSC, LEF, JJ, TC, SS, ZL, QJL and JR; data curation: KSC, JJ, LEF, TC, ZL and SS; formal analysis: KSC, LEF, JJ, TC and SS; writing original draft: KSC and JJ; review and editing: KSC, JJ and QJL; resources: KSC, QJL and JR; funding acquisition: KSC and QJL; supervision: KSC.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki. All studies involving human subjects and tissues were approved by the Institutional Review Board at UTHealth Houston (HSC-MS-20-0327 and HSC-MS-21-0074). Written informed consent was obtained from all participants. All animal experiments were approved by the Animal Welfare Committee (AWC-20-0144) at UTHealth Houston.
Consent to publish
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jacob, J., Francisco, L.E., Chatterjee, T. et al. An antibody–drug conjugate targeting GPR56 demonstrates efficacy in preclinical models of colorectal cancer. Br J Cancer 128, 1592–1602 (2023). https://doi.org/10.1038/s41416-023-02192-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02192-3