Abstract
Background
Study 10, a four-part Phase 1/2 study, evaluated oral rucaparib monotherapy in patients with advanced solid tumours. Here we report the final efficacy and safety results in heavily pretreated patients with ovarian cancer who received rucaparib in Study 10 Parts 2A and 2B.
Methods
Parts 2A and 2B (Phase 2 portions) enrolled patients with relapsed, high-grade, platinum-sensitive or platinum-resistant, BRCA-mutated ovarian cancer who had received 2–4 (Part 2A) or 3–4 (Part 2B) prior chemotherapies. Patients received oral rucaparib 600 mg twice daily (starting dose). The primary endpoint was the investigator-assessed objective response rate (ORR) by RECIST v1.1.
Results
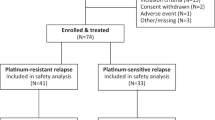
Fifty-four patients were enrolled: 42 in Part 2A (all had platinum-sensitive disease) and 12 in Part 2B (4 with platinum-sensitive disease; 8 with platinum-resistant disease). ORR was 59.3% (95% CI 45.0–72.4%). The median time to onset of the most common nonhaematological treatment-emergent adverse events (TEAEs) was typically early (<56 days) and was later for haematological TEAEs (53–84 days). The median duration of grade ≥3 TEAEs was ≤13 days.
Conclusions
In patients with relapsed, platinum-sensitive or platinum-resistant germline BRCA-mutant high-grade ovarian cancer who had received ≥2 prior chemotherapies, rucaparib had robust antitumour activity with a safety profile consistent with prior reports.
Clinical trial registration
NCT01482715.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Consent was not obtained from patients to allow the posting of the data to public repositories. Requests for de-identified datasets for the results reported in this publication will be made available to qualified researchers following the submission of a methodologically sound proposal to medinfo@clovisoncology.com. Data will be made available for such requests following the online publication of this article and for 1 year thereafter in compliance with applicable privacy laws, data protection, and requirements for consent and anonymization. Data will be provided by Clovis Oncology. The redacted protocol for the Study 10 clinical study is available on https://clinicaltrials.gov/ProvidedDocs/15/NCT01482715/Prot_000.pdf. Clovis Oncology does not share identified participant data or a data dictionary.
References
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al. Global cancer observatory: cancer today. Lyon, France: International Agency for Research on Cancer; 2020.
National Cancer Institute (NCI). SEER Cancer Statistics Factsheets: Ovarian cancer. 2021. http://seer.cancer.gov/statfacts/html/ovary.html. Accessed June 30, 2022.
Bouberhan S, Pujade-Lauraine E, Cannistra SA. Advances in the management of platinum-sensitive relapsed ovarian cancer. J Clin Oncol. 2019;37:2424–36.
Colombo N, Sessa C, du Bois A, Ledermann J, McCluggage WG, McNeish I, et al. ESMO–ESGO consensus conference recommendations on ovarian cancer: pathology and molecular biology, early and advanced stages, borderline tumours and recurrent disease. Ann Oncol. 2019;30:672–705.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidlines®). Ovarian cancer including fallopian tube cancer and primary peritoneal cancer (version 1.2022). 2022. https://www.nccn.org/professionals/physician_gls/pdf/ovarian.pdf. Accessed June 30, 2022.
Colombo N. Optimising the treatment of the partially platinum-sensitive relapsed ovarian cancer patient. Eur J Cancer Suppl. 2014;12:7–12.
Baert T, Ferrero A, Sehouli J, O’Donnell DM, González-Martín A, Joly F, et al. The systemic treatment of recurrent ovarian cancer revisited. Ann Oncol. 2021;32:710–25.
Herzog TJ, Monk BJ. Bringing new medicines to women with epithelial ovarian cancer: what is the unmet medical need. Gyneco l Oncol Res Pract. 2017;4:13.
Dal Molin GZ, Westin SN, Coleman RL. Rucaparib in ovarian cancer: extending the use of PARP inhibitors in the recurrent disease. Future Oncol. 2018;14:3101–10.
Gupta S, Nag S, Aggarwal S, Rauthan A, Warrier N. Maintenance therapy for recurrent epithelial ovarian cancer: current therapies and future perspectives - a review. J Ovarian Res. 2019;12:103.
Rubraca (rucaparib) tablets [prescribing information]. Boulder, CO: Clovis Oncology, Inc.; 2022.
Rubraca (rucaparib) tablets [summary of product characteristics]. Swords, Ireland: Clovis Oncology Ireland Ltd.; 2022).
Robillard L, Nguyen M, Harding TC, Simmons AD. In vitro and in vivo assessment of the mechanism of action of the PARP inhibitor rucaparib. Cancer Res. 2017;77:abst 2475.
Drew Y, Mulligan EA, Vong WT, Thomas HD, Kahn S, Kyle S, et al. Therapeutic potential of poly(ADP-ribose) polymerase inhibitor AG014699 in human cancers with mutated or methylated BRCA1 or BRCA2. J Natl Cancer Inst. 2011;103:334–46.
Murai J, Huang SY, Renaud A, Zhang Y, Ji J, Takeda S, et al. Stereospecific PARP trapping by BMN 673 and comparison with olaparib and rucaparib. Mol Cancer Ther. 2014;13:433–43.
Lin KK, Harrell MI, Oza AM, Oaknin A, Ray-Coquard I, Tinker AV, et al. BRCA reversion mutations in circulating tumor DNA predict primary and acquired resistance to the PARP inhibitor rucaparib in high-grade ovarian carcinoma. Cancer Discov. 2019;9:210–9.
Kristeleit R, Lisyanskaya A, Fedenko A, Dvorkin M, de Melo AC, Shparyk Y, et al. Rucaparib versus standard-of-care chemotherapy in patients with relapsed ovarian cancer and a deleterious BRCA1 or BRCA2 mutation (ARIEL4): an international, open-label, randomised, phase 3 trial. Lancet Oncol. 2022;23:465–78.
Kristeleit R, Shapiro GI, Burris HA, Oza AM, LoRusso P, Patel MR, et al. A phase I-II study of the oral PARP inhibitor rucaparib in patients with germline BRCA1/2-mutated ovarian carcinoma or other solid tumors. Clin Cancer Res. 2017;23:4095–106.
Shapiro GI, Kristeleit R, Burris HA, LoRusso P, Patel MR, Drew Y, et al. Pharmacokinetic study of rucaparib in patients with advanced solid tumors. Clin Pharmacol Drug Dev. 2019;8:107–18.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Rustin GJ, Vergote I, Eisenhauer E, Pujade-Lauraine E, Quinn M, Thigpen T, et al. Definitions for response and progression in ovarian cancer clinical trials incorporating RECIST 1.1 and CA 125 agreed by the Gynecological Cancer Intergroup (GCIG). Int J Gynecol Cancer. 2011;21:419–23.
Pujade-Lauraine E, Selle F, Scambia G, Asselain B, Marmé F, Lindemann K, et al. Maintenance olaparib rechallenge in patients (pts) with ovarian carcinoma (OC) previously treated with a PARP inhibitor (PARPi): phase IIIb OReO/ENGOT Ov-38 trial. Ann Oncol. 2021;32:abst LBA33.
Selle F, Asselain B, Montestruc F, Bazan F, Pardo B, Salutari V, et al. OReO/ENGOT Ov-38 trial: impact of maintenance olaparib rechallenge according to ovarian cancer patient prognosis—an exploratory joint analysis of the BRCA and non-BRCA cohorts. J Clin Oncol. 2022;40:abst 5558.
Oza AM, Lisyanskaya AS, Fedenko AA, Dvorkin M, Melo ACD, Shparyk YV, et al. Subgroup analysis of rucaparib versus chemotherapy as treatment for BRCA-mutated, advanced, relapsed ovarian carcinoma: effect of platinum sensitivity in the randomized, phase 3 study ARIEL4. J Clin Oncol. 2021;39:abst 5517.
Penson RT, Valencia RV, Cibula D, Colombo N, Leath CA 3rd, Bidzinski M, et al. Olaparib versus nonplatinum chemotherapy in patients with platinum-sensitive relapsed ovarian cancer and a germline BRCA1/2 mutation (SOLO3): a randomized phase III trial. J Clin Oncol. 2020;38:1164–74.
Moore KN, Secord AA, Geller MA, Miller DS, Cloven N, Fleming GF, et al. Niraparib monotherapy for late-line treatment of ovarian cancer (QUADRA): a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2019;20:636–48.
Oza AM, Tinker AV, Oaknin A, Shapira-Frommer R, McNeish IA, Swisher EM, et al. Antitumor activity and safety of the PARP inhibitor rucaparib in patients with high-grade ovarian carcinoma and a germline or somatic BRCA1 or BRCA2 mutation: integrated analysis of data from Study 10 and ARIEL2. Gynecol Oncol. 2017;147:267–75.
Kristeleit RS, Oaknin A, Ray-Coquard I, Leary A, Balmana J, Drew Y, et al. Antitumor activity of the poly(ADP-ribose) polymerase inhibitor rucaparib as monotherapy in patients with platinum-sensitive, relapsed, BRCA-mutated, high-grade ovarian cancer, and an update on safety. Int J Gynecol Cancer. 2019;29:1396–404.
Coleman RL, Oza AM, Lorusso D, Aghajanian C, Oaknin A, Dean A, et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390:1949–61.
Ledermann JA, Oza AM, Lorusso D, Aghajanian C, Oaknin A, Dean A, et al. Rucaparib for patients with platinum-sensitive, recurrent ovarian carcinoma (ARIEL3): postprogression outcomes and updated safety from a randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2020;21:710–22.
Swisher EM, Lin KK, Oza AM, Scott CL, Giordano H, Sun J, et al. Rucaparib in relapsed, platinum-sensitive high-grade ovarian carcinoma (ARIEL2 Part 1): an international, multicentre, open-label, phase 2 trial. Lancet Oncol. 2017;18:75–87.
Lorusso D, García-Donas J, Sehouli J, Joly F. Management of adverse events during rucaparib treatment for relapsed ovarian cancer: a review of published studies and practical guidance. Target Oncol. 2020;15:391–406.
Tookman L, Krell J, Nkolobe B, Burley L, McNeish IA. Practical guidance for the management of side effects during rucaparib therapy in a multidisciplinary UK setting. Ther Adv Med Oncol. 2020;12:1758835920921980.
Labadie BW, Morris DS, Bryce AH, Given R, Zhang J, Abida W, et al. Guidelines for management of treatment-emergent adverse events during rucaparib treatment of patients with metastatic castration-resistant prostate cancer. Cancer Manag Res. 2022;14:673–86.
Pujade-Lauraine E, Ledermann JA, Selle F, Gebski V, Penson RT, Oza AM, et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:1274–84.
Kikuchi R, Lao Y, Bow DAJ, Chiou WJ, Andracki ME, Carr RA, et al. Prediction of clinical drug-drug interactions of veliparib (ABT-888) with human renal transporters (OAT1, OAT3, OCT2, MATE1, and MATE2K). J Pharm Sci. 2013;102:4426–32.
McCormick A, Swaisland H. In vitro assessment of the roles of drug transporters in the disposition and drug-drug interaction potential of olaparib. Xenobiotica. 2017;47:903–15.
Zibetti Dal Molin G, Westin SN, Msaouel P, Gomes LM, Dickens A, Coleman RL. Discrepancy in calculated and measured glomerular filtration rates in patients treated with PARP inhibitors. Int J Gynecol Cancer. 2020;30:89–93.
Dean A, Oza AM, Lorusso D, Aghajanian C, Oaknin A, Colombo N, et al. Timing of adverse events during maintenance treatment with rucaparib for recurrent ovarian cancer in the phase III ARIEL3 study. Ann Oncol 2020;31:abst 821P.
Moore KN, Secord A, Geller MA, Miller DS, Cloven NG, Fleming GF, et al. QUADRA: A phase 2, open-label, single-arm study to evaluate niraparib in patients (pts) with relapsed ovarian cancer (ROC) who have received ≥3 prior chemotherapy regimens. J Clin Oncol. 2018;36:abst 5514.
Acknowledgements
Medical writing and editorial support were funded by Clovis Oncology, Inc., and were provided by Nathan Yardley and Stephen Bublitz of Ashfield MedComms, an Inizio company.
Funding
This study was funded by Clovis Oncology, Inc. (Boulder, USA).
Author information
Authors and Affiliations
Contributions
RSK, YD, TS, SG and LM designed the study. RSK, YD, AMO, SMD, SB, RMG, Judith Balmaña, LC, MRP, HAB, TS and RSF treated patients. RSK, YD, AMO, SMD, SB, RMG, Judith Balmaña, LC, MRP, HAB, TS, KKL and RSF acquired the data. RSK, KKL, SG and LM interpreted data. All authors wrote the manuscript and reviewed draft and final versions of it.
Corresponding author
Ethics declarations
Competing interests
RSK has received institutional funding from Clovis Oncology for this clinical trial; reports clinical trial grants from Merck Sharp & Dohme; has served as a consultant from Basilea Pharmaceutica and Shattuck Pharma; has received honoraria from Clovis Oncology, AstraZeneca, GlaxoSmithKline, and Incyte; received travelling support from AstraZeneca, GlaxoSmithKline, and Sierra Oncology; has served on data safety monitoring boards or advisory boards for Clovis Oncology, AstraZeneca, BeiGene, Eisai, GlaxoSmithKline, Incyte, iTeos Therapeutics, PharmaMar and Roche. YD has contributed to the development of rucaparib and has received royalty payments from Newcastle University for this work; has received research funding from Clovis Oncology, AstraZeneca, Merck KGaA, and Verastem; and has received honoraria for advisory boards/speakers fees from Clovis Oncology, AstraZeneca, Genmab, GlaxoSmithKline, Merck and Tesaro. AMO reports institutional research grants from AstraZeneca; served on an advisory board (uncompensated) for GlaxoSmithKline; served on advisory boards and steering committees (uncompensated) for Clovis Oncology and AstraZeneca; served as a principal investigator on investigator-initiated trials for Clovis Oncology, AstraZeneca, and GlaxoSmithKline. SMD has received research funding from Clovis Oncology and AstraZeneca; and has received honoraria from Clovis Oncology, AstraZeneca, and Bristol Myers Squibb. SB has served on advisory boards and received honoraria from Clovis Oncology, AstraZeneca, Genmab, GlaxoSmithKline, Immunogen, Merck Serono, Merck Sharp & Dohme, Mersana, Pfizer, Roche, Seattle Genetics, and Tesaro; received honoraria for lectures from AstraZeneca/Merck Sharp & Dohme, GlaxoSmithKline, Pfizer, Roche, and Tesaro; received support for travel or accommodation from NuCana and Tesaro; and reports institutional funding from AstraZeneca, GlaxoSmithKline and Tesaro. RMG reports grant funding for investigator-initiated studies from Clovis Oncology, Boehringer Ingelheim and Lilly/Ignyta; institutional fees from Novartis; institutional drug donation from GSK; personal fees from Clovis Oncology, AstraZeneca, and GlaxoSmithKline/Tesaro, Immunogen, Merck Sharp & Dohme and Sotio; and conference registration fees from GSK. Judith Balmaña has served on advisory boards for Clovis Oncology, AstraZeneca, and Bristol Myers Squibb; and has received support for travel from AstraZeneca. L-mC has received institutional funding from Clovis Oncology, AstraZeneca, Genentech, and GlaxoSmithKline/Tesaro for this clinical trial and others. MRP reports a leadership position with ION Pharma; has received honoraria from Adaptive Biotechnologies, Bayer, Genentech, Janssen Oncology, Pfizer, and Pharmacyclics; has served in a consulting or advisory role for Pharmacyclics/Janssen and Pfizer/EMD Serono; has served on speakers’ bureaus for Celgene, Exelixis, Genentech/Roche, and Taiho Pharmaceutical; his institution has received research funding from Clovis Oncology, Acerta Pharma, ADC Therapeutics, Agenus, Aileron Therapeutics, Artios, AstraZeneca, Bayer, Bicycle Therapeutics, BioNTech AG, BioTheryX, Black Diamond Therapeutics, Boehringer Ingelheim, Calithera Biosciences, Celgene, Checkpoint Therapeutics, CicloMed, Curis, Cyteir Therapeutics, Daiichi Sankyo, eFFECTOR Therapeutics, EMD Serono, Erasca, Evelo Biosciences, Forma Therapeutics, Genetec/Roche, Gilead Sciences, GlaxoSmithKline, H3 Biomedicine, Hengrui Therapeutics, Hutchison MediPharma, IgM Biosciences, Ignyta, Incyte, Jacobio Pharmaceuticals, Janssen, Jounce Therapeutics, Klus Pharma, Kymab, Lilly, Loxo Oncology, LSK BioPartners, Lycera, Mabspace, MacroGenics, Merck, Millennium, Mirati Therapeutics, Moderna Therapeutics, NGM Biopharmaceuticals, Novartis, Nurix, ORIC, Pfizer, Phoenix Molecular Designs, Placon, Portola Pharmaceuticals, Prelude Therapeutics, Puget Sound Biotherapeutics, PureTech, QiLu Pharmaceutical, Relay Therapeutics, Revolution Medicines, Ribon Therapeutics, Samumed, Seven and Eight Biopharmaceuticals, Silicon Therapeutics, Stemline Therapeutics, Syndax, Synthorx, Taiho Pharmaceutical, Takeda, TeneoBio, Tesaro, TopAlliance BioSciences, Treadwell Therapeutics, Vedanta Biosciences, Verastem Oncology, Vigeo, Xencor, and Zymeworks. HAB reports payment for consulting services from AstraZeneca, Celgene, Forma Therapeutics, and Incyte; has received payment for his expert testimony from Novartis; has performed noncompensated consulting services for Bayer, Daiichi Sankyo, GRAIL, Novartis, and Pfizer; and his institution has received grants for conduct of clinical trials from Clovis Oncology, Agios, Arch, Array BioPharma, Arvinas, AstraZeneca, Bayer, BIND Therapeutics, BioAtla, BioMed Valley Discoveries, Boehringer Ingelheim, Bristol Myers Squibb, CicloMed, CytomX Therapeutics, eFFECTOR Therapeutics, Foundation Medicine, Gilead Sciences, GlaxoSmithKline, Harpoon Therapeutics, Incyte, Janssen, Jounce Therapeutics, Kyocera, Lilly, Macrogenics, MedImmune, Merck, miRNA Therapeutics, Moderna Therapeutics, Novartis, Pfizer, Revolution Medicines, Roche/Genentech, Seattle Genetics, Takeda/Millennium, Tesaro, TG Therapeutics, Verastem, and Vertex. Dr. Burris is employed by and has a leadership position at HCA Healthcare/Sarah Cannon Research Institute and owns stock in that company. TS declares no conflict of interest. Jennifer Borrow, KKL, SG and LM are employees of Clovis Oncology and may own stock or have stock options in that company. RS-F has received research grants from Merck Sharp & Dohme; and has received speaker honoraria from AstraZeneca, Bristol Myers Squibb, Medison, Merck Sharp & Dohme, Neopharm and Novartis.
Ethics approval and consent to participate
The study was approved by an institutional review board at each study site and was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines of the International Council for Harmonisation.
Consent to publish
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kristeleit, R.S., Drew, Y., Oza, A.M. et al. Efficacy and safety of rucaparib treatment in patients with BRCA-mutated, relapsed ovarian cancer: final results from Study 10. Br J Cancer 128, 255–265 (2023). https://doi.org/10.1038/s41416-022-02022-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-02022-y