Abstract
Background
RSPO fusions that lead to WNT pathway activation are potential therapeutic targets in colorectal cancer (CRC), but their clinicopathological significance remains unclear.
Methods
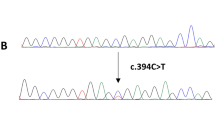
We screened 1019 CRCs for RSPO fusions using multiplex reverse transcription–PCR. The RSPO fusion-positive tumours were subjected to whole-exome sequencing (WES).
Results
Our analysis identified 29 CRCs with RSPO fusions (2.8%), consisting of five with an EIF3E-RSPO2 fusion and 24 with PTPRK-RSPO3 fusions. The patients were 17 women and 12 men. Thirteen tumours (45%) were right-sided. Histologically, approximately half of the tumours (13/29, 45%) had a focal or extensive mucinous component that was significantly more frequent than the RSPO fusion-negative tumours (13%; P = 8.1 × 10−7). Four tumours (14%) were mismatch repair-deficient. WES identified KRAS, BRAF, and NRAS mutations in a total of 27 tumours (93%). In contrast, pathogenic mutations in major WNT pathway genes, such as APC, CTNNB1 and RNF43, were absent. RSPO fusion status did not have a statistically significant influence on the overall or recurrence-free survival. These clinicopathological and genetic features were also confirmed in a pooled analysis of previous studies.
Conclusion
RSPO fusion-positive CRCs constitute a rare subgroup of CRCs with several characteristic clinicopathological and genetic features.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Nucleotide sequence data reported are available in the DDBJ database under the accession number JGAS000538.
References
Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–7.
Giannakis M, Hodis E, Jasmine Mu X, Yamauchi M, Rosenbluh J, Cibulskis K, et al. RNF43 is frequently mutated in colorectal and endometrial cancers. Nat Genet. 2014;46:1264–6.
Yaeger R, Chatila WK, Lipsyc MD, Hechtman JF, Cercek A, Sanchez-Vega F, et al. Clinical sequencing defines the genomic landscape of metastatic colorectal cancer. Cancer Cell. 2018;33:125–36.e3.
Kleeman SO, Leedham SJ. Not all Wnt activation is equal: ligand-dependent versus ligand-independent Wnt activation in colorectal cancer. Cancers. 2020;12:3355.
Seshagiri S, Stawiski EW, Durinck S, Modrusan Z, Storm EE, Conboy CB, et al. Recurrent R-spondin fusions in colon cancer. Nature. 2012;488:660–4.
de Lau W, Barker N, Low TY, Koo BK, Li VS, Teunissen H, et al. Lgr5 homologues associate with Wnt receptors and mediate R-spondin signalling. Nature. 2011;476:293–7.
Storm EE, Durinck S, de Sousa e Melo F, Tremayne J, Kljavin N, Tan C, et al. Targeting PTPRK-RSPO3 colon tumours promotes differentiation and loss of stem-cell function. Nature. 2016;529:97–100.
Fischer MM, Yeung VP, Cattaruzza F, Hussein R, Yen WC, Murriel C, et al. RSPO3 antagonism inhibits growth and tumorigenicity in colorectal tumors harboring common Wnt pathway mutations. Sci Rep. 2017;7:15270.
Madan B, Ke Z, Harmston N, Ho SY, Frois AO, Alam J, et al. Wnt addiction of genetically defined cancers reversed by PORCN inhibition. Oncogene. 2016;35:2197–207.
Li C, Cao J, Zhang N, Tu M, Xu F, Wei S, et al. Identification of RSPO2 fusion mutations and target therapy using a porcupine inhibitor. Sci Rep. 2018;8:14244.
Picco G, Petti C, Centonze A, Torchiaro E, Crisafulli G, Novara L, et al. Loss of AXIN1 drives acquired resistance to WNT pathway blockade in colorectal cancer cells carrying RSPO3 fusions. EMBO Mol Med. 2017;9:293–303.
Shinmura K, Kahyo T, Kato H, Igarashi H, Matsuura S, Nakamura S, et al. RSPO fusion transcripts in colorectal cancer in Japanese population. Mol Biol Rep. 2014;41:5375–84.
Kloosterman WP, Coebergh van den Braak RRJ, Pieterse M, van Roosmalen MJ, Sieuwerts AM, Stangl C, et al. A systematic analysis of oncogenic gene fusions in primary colon cancer. Cancer Res. 2017;77:3814–22.
Mizuguchi Y, Sakamoto T, Hashimoto T, Tsukamoto S, Iwasa S, Saito Y, et al. Identification of a novel PRR15L-RSPO2 fusion transcript in a sigmoid colon cancer derived from superficially serrated adenoma. Virchows Arch. 2019;475:659–63.
Kleeman SO, Koelzer VH, Jones HJ, Vazquez EG, Davis H, East JE, et al. Exploiting differential Wnt target gene expression to generate a molecular biomarker for colorectal cancer stratification. Gut. 2020;69:1092–103.
Yan HHN, Siu HC, Ho SL, Yue SSK, Gao Y, Tsui WY, et al. Organoid cultures of early-onset colorectal cancers reveal distinct and rare genetic profiles. Gut. 2020;69:2165–79.
Conboy CB, Velez-Reyes GL, Rathe SK, Abrahante JE, Temiz NA, Burns MB, et al. R-Spondins 2 and 3 are overexpressed in a subset of human colon and breast cancers. DNA Cell Biol. 2021;40:70–9.
Sekine S, Ogawa R, Hashimoto T, Motohiro K, Yoshida H, Taniguchi H, et al. Comprehensive characterization of RSPO fusions in colorectal traditional serrated adenomas. Histopathology. 2017;71:601–9.
Hashimoto T, Ogawa R, Yoshida H, Taniguchi H, Kojima M, Saito Y, et al. EIF3E-RSPO2 and PIEZO1-RSPO2 fusions in colorectal traditional serrated adenoma. Histopathology. 2019;75:266–73.
Nagtegaal IDAM, Salto-Tellez M. Colorectal adenocarcinoma. In: WHO Classification of Tumours Editorial Board (ed). WHO classification of tumours digestive system tumors, 5th edn. Lyon, France: IARC Press; 2019. pp. 181–7.
Rozek LS, Schmit SL, Greenson JK, Tomsho LP, Rennert HS, Rennert G, et al. Tumor-infiltrating lymphocytes, Crohn’s-like lymphoid reaction, and survival from colorectal cancer. J Natl Cancer Inst. 2016;108:djw027.
Cibulskis K, Lawrence MS, Carter SL, Sivachenko A, Jaffe D, Sougnez C, et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat Biotechnol. 2013;31:213–9.
Dietlein F, Weghorn D, Taylor-Weiner A, Richters A, Reardon B, Liu D, et al. Identification of cancer driver genes based on nucleotide context. Nat Genet. 2020;52:208–18.
Thorvaldsdottir H, Robinson JT, Mesirov JP. Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Brief Bioinform. 2013;14:178–92.
Yonemaru J, Hashimoto T, Takayanagi D, Naka T, Yatabe Y, Kanemitsu Y, et al. NTRK fusion-positive colorectal cancer in Japanese population. Pathol Int. 2021;71:355–9.
Yokota T, Saito Y, Takamaru H, Sekine S, Nakajima T, Yamada M, et al. Spontaneous regression of mismatch repair-deficient colon cancer: a case series. Clin Gastroenterol Hepatol. 2021;19:1720–2.e3.
Grasso CS, Giannakis M, Wells DK, Hamada T, Mu XJ, Quist M, et al. Genetic mechanisms of immune evasion in colorectal cancer. Cancer Discov. 2018;8:730–49.
Jass JR, Atkin WS, Cuzick J, Bussey HJ, Morson BC, Northover JM, et al. The grading of rectal cancer: historical perspectives and a multivariate analysis of 447 cases. Histopathology. 1986;10:437–59.
Greenson JK, Bonner JD, Ben-Yzhak O, Cohen HI, Miselevich I, Resnick MB, et al. Phenotype of microsatellite unstable colorectal carcinomas: Well-differentiated and focally mucinous tumors and the absence of dirty necrosis correlate with microsatellite instability. Am J Surg Pathol. 2003;27:563–70.
Gonzalez RS, Cates JMM, Washington K. Associations among histological characteristics and patient outcomes in colorectal carcinoma with a mucinous component. Histopathology. 2019;74:406–14.
Huang L, Luo S, Zhang X, Cai Y, Xue F, Hu H, et al. Distinct genomic landscape of colorectal mucinous carcinoma determined via comprehensive genomic profiling: steps to a new treatment strategy. Front Oncol. 2021;11:603564.
Shia J, Ellis NA, Paty PB, Nash GM, Qin J, Offit K, et al. Value of histopathology in predicting microsatellite instability in hereditary nonpolyposis colorectal cancer and sporadic colorectal cancer. Am J Surg Pathol. 2003;27:1407–17.
Alexander J, Watanabe T, Wu TT, Rashid A, Li S, Hamilton SR. Histopathological identification of colon cancer with microsatellite instability. Am J Pathol. 2001;158:527–35.
Rimbert J, Tachon G, Junca A, Villalva C, Karayan-Tapon L, Tougeron D. Association between clinicopathological characteristics and RAS mutation in colorectal cancer. Mod Pathol. 2018;31:517–26.
Shia J, Schultz N, Kuk D, Vakiani E, Middha S, Segal NH, et al. Morphological characterization of colorectal cancers in The Cancer Genome Atlas reveals distinct morphology-molecular associations: clinical and biological implications. Mod Pathol. 2017;30:599–609.
Stachler MD, Rinehart E, Lindeman N, Odze R, Srivastava A. Novel molecular insights from routine genotyping of colorectal carcinomas. Hum Pathol. 2015;46:507–13.
Pai RK, Jayachandran P, Koong AC, Chang DT, Kwok S, Ma L, et al. BRAF-mutated, microsatellite-stable adenocarcinoma of the proximal colon: an aggressive adenocarcinoma with poor survival, mucinous differentiation, and adverse morphologic features. Am J Surg Pathol. 2012;36:744–52.
Sekine S, Yamashita S, Tanabe T, Hashimoto T, Yoshida H, Taniguchi H, et al. Frequent PTPRK-RSPO3 fusions and RNF43 mutations in colorectal traditional serrated adenoma. J Pathol. 2016;239:133–8.
Sekine S, Yamashita S, Yamada M, Hashimoto T, Ogawa R, Yoshida H, et al. Clinicopathological and molecular correlations in traditional serrated adenoma. J Gastroenterol. 2020;55:418–27.
Jorissen RN, Christie M, Mouradov D, Sakthianandeswaren A, Li S, Love C, et al. Wild-type APC predicts poor prognosis in microsatellite-stable proximal colon cancer. Br J Cancer. 2015;113:979–88.
Wang C, Ouyang C, Cho M, Ji J, Sandhu J, Goel A, et al. Wild-type APC is associated with poor survival in metastatic microsatellite stable colorectal cancer. Oncologist. 2021;26:208–14.
Acknowledgements
We thank Ms. Reiko Ogawa, Ms. Sachiko Miura, Ms. Toshiko Sakaguchi and Ms. Chizu Kina for their skilful technical assistance. We also thank Dr. Andrew Blake for help in data preparation. Part of the data used in the preparation of this manuscript were obtained and analysed from the datasets available through the MRC and CRUK funded S:CORT consortium.
Funding
This study was supported by Kurozumi Medical Foundation and JSPS KAKENHI Grant number 20K07382.
Author information
Authors and Affiliations
Contributions
TH, DT, KS and SS carried out experiments and analysed data. TH, JY, TN, YY and SS performed histological analyses. KN conducted the statistical analysis. TH and SS wrote the manuscript. DS, SK, SL, TM and AT provided clinicopathological and mutation data. RH reviewed the paper. All authors provided critical revisions of the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the National Cancer Center Tokyo, Japan. The study was performed in accordance with the Declaration of Helsinki.
Consent to publish
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hashimoto, T., Takayanagi, D., Yonemaru, J. et al. Clinicopathological and molecular characteristics of RSPO fusion-positive colorectal cancer. Br J Cancer 127, 1043–1050 (2022). https://doi.org/10.1038/s41416-022-01880-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01880-w
This article is cited by
-
Incidence and clinical significance of 491 known fusion genes in a large cohort of Japanese patients with colorectal cancer
International Journal of Clinical Oncology (2023)