Abstract
Background
The causal pathway between high education and reduced risk of gastric cancer (GC) has not been explained. The study aimed at evaluating the mediating role of lifestyle factors on the relationship between education and GC
Methods
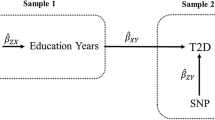
Ten studies with complete data on education and five lifestyle factors (smoking, alcohol drinking, fruit and vegetable intake, processed meat intake and salt consumption) were selected from a consortium of studies on GC including 4349 GC cases and 8441 controls. We created an a priori score based on the five lifestyle factors, and we carried out a counterfactual-based mediation analysis to decompose the total effect of education on GC into natural direct effect and natural indirect effect mediated by the combined lifestyle factors. Effects were expressed as odds ratios (ORs) with a low level of education as the reference category.
Results
The natural direct and indirect effects of high versus low education were 0.69 (95% CI: 0.62–0.77) and 0.96 (95% CI: 0.95–0.97), respectively, corresponding to a mediated percentage of 10.1% (95% CI: 7.1–15.4%). The mediation effect was limited to men.
Conclusions
The mediation effect of the combined lifestyle factors on the relationship between education and GC is modest. Other potential pathways explaining that relationship warrants further investigation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of our study are available from the Stomach cancer Pooling (StoP) Project but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however, available from the authors upon reasonable request and with permission of the Steering Committee of the StoP Project.
References
Santucci C, Carioli G, Bertuccio P, Malvezzi M, Pastorino U, Boffetta P, et al. Progress in cancer mortality, incidence, and survival: a global overview. Eur J Cancer Prev. 2020;29:367–81.
Ferlay J, Ervik M, Lam F, Comobet M, Mery L, Piñeros M, et al. Global Cancer Observatory: Cancer Today. International Agency for Research on Cancer, 2020. https://gco.iarc.fr/today/home. Accessed 15 April 2021.
Praud D, Rota M, Pelucchi C, Bertuccio P, Rosso T, Galeone C, et al. Cigarette smoking and gastric cancer in the Stomach Cancer Pooling (StoP) Project. Eur J Cancer Prev. 2018;27:124–33.
Rota M, Pelucchi C, Bertuccio P, Matsuo K, Zhang ZF, Ito H, et al. Alcohol consumption and gastric cancer risk-A pooled analysis within the StoP project consortium. Int J Cancer. 2017;141:1950–62.
Ferro A, Rosato V, Rota M, Costa AR, Morais S, Pelucchi C, et al. Meat intake and risk of gastric cancer in the Stomach cancer Pooling (StoP) project. Int J Cancer. 2020;147:45–55.
D’Elia L, Rossi G, Ippolito R, Cappuccio FP, Strazzullo P. Habitual salt intake and risk of gastric cancer: a meta-analysis of prospective studies. Clin Nutr. 2012;31:489–98.
Bertuccio P, Alicandro G, Rota M, Pelucchi C, Bonzi R, Galeone C, et al. Citrus fruit intake and gastric cancer: The stomach cancer pooling (StoP) project consortium. Int J Cancer. 2019;144:2936–44.
Ferro A, Costa AR, Morais S, Bertuccio P, Rota M, Pelucchi C, et al. Fruits and vegetables intake and gastric cancer risk: a pooled analysis within the Stomach cancer Pooling Project. Int J Cancer. 2020;147:3090–101.
Hausdorf K, Eakin E, Whiteman D, Rogers C, Aitken J, Newman B. Prevalence and correlates of multiple cancer risk behaviors in an Australian population-based survey: results from the Queensland Cancer Risk Study. Cancer Causes Control. 2008;19:1339–47.
Kvaavik E, Batty GD, Ursin G, Huxley R, Gale CR. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: the United Kingdom health and lifestyle survey. Arch Intern Med. 2010;170:711–8.
Schuit AJ, van Loon AJ, Tijhuis M, Ocke M. Clustering of lifestyle risk factors in a general adult population. Prev Med. 2002;35:219–24.
Buckland G, Travier N, Huerta JM, Bueno-de-Mesquita HB, Siersema PD, Skeie G, et al. Healthy lifestyle index and risk of gastric adenocarcinoma in the EPIC cohort study. Int J Cancer. 2015;137:598–606.
Jiao L, Mitrou PN, Reedy J, Graubard BI, Hollenbeck AR, Schatzkin A, et al. A combined healthy lifestyle score and risk of pancreatic cancer in a large cohort study. Arch Intern Med. 2009;169:764–70.
Lohse T, Faeh D, Bopp M, Rohrmann S, Swiss National Cohort Study G. Adherence to the cancer prevention recommendations of the World Cancer Research Fund/American Institute for Cancer Research and mortality: a census-linked cohort. Am J Clin Nutr. 2016;104:678–85.
Alicandro G, Frova L, Sebastiani G, El Sayed I, Boffetta P, La Vecchia C. Educational inequality in cancer mortality: a record linkage study of over 35 million Italians. Cancer Causes Control. 2017;28:997–1006.
Lagergren J, Andersson G, Talback M, Drefahl S, Bihagen E, Harkonen J, et al. Marital status, education, and income in relation to the risk of esophageal and gastric cancer by histological type and site. Cancer. 2016;122:207–12.
Rota M, Alicandro G, Pelucchi C, Bonzi R, Bertuccio P, Hu J, et al. Education and gastric cancer risk—an individual participant data meta-analysis in the StoP project consortium. Int J Cancer. 2020;146:671–81.
Zhang YB, Chen C, Pan XF, Guo J, Li Y, Franco OH, et al. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies. BMJ. 2021;373:n604.
Pelucchi C, Lunet N, Boccia S, Zhang ZF, Praud D, Boffetta P, et al. The stomach cancer pooling (StoP) project: study design and presentation. Eur J Cancer Prev. 2015;24:16–23.
La Vecchia C, D’Avanzo B, Negri E, Decarli A, Benichou J. Attributable risks for stomach cancer in northern Italy. Int J Cancer. 1995;60:748–52.
Pelucchi C, Tramacere I, Bertuccio P, Tavani A, Negri E, La Vecchia C. Dietary intake of selected micronutrients and gastric cancer risk: an Italian case-control study. Ann Oncol. 2009;20:160–5.
Zaridze D, Borisova E, Maximovitch D, Chkhikvadze V. Alcohol consumption, smoking and risk of gastric cancer: case-control study from Moscow, Russia. Cancer Causes Control. 2000;11:363–71.
Santibanez M, Alguacil J, de la Hera MG, Navarrete-Munoz EM, Llorca J, Aragones N, et al. Occupational exposures and risk of stomach cancer by histological type. Occup Environ Med. 2012;69:268–75.
Pourfarzi F, Whelan A, Kaldor J, Malekzadeh R. The role of diet and other environmental factors in the causation of gastric cancer in Iran-a population based study. Int J Cancer. 2009;125:1953–60.
Zhang ZF, Kurtz RC, Klimstra DS, Yu GP, Sun M, Harlap S, et al. Helicobacter pylori infection on the risk of stomach cancer and chronic atrophic gastritis. Cancer Detect Prev. 1999;23:357–67.
Schatzkin A, Subar AF, Thompson FE, Harlan LC, Tangrea J, Hollenbeck AR, et al. Design and serendipity in establishing a large cohort with wide dietary intake distributions: the National Institutes of Health-American Association of Retired Persons Diet and Health Study. Am J Epidemiol. 2001;154:1119–25.
Hernandez-Ramirez RU, Galvan-Portillo MV, Ward MH, Agudo A, Gonzalez CA, Onate-Ocana LF, et al. Dietary intake of polyphenols, nitrate and nitrite and gastric cancer risk in Mexico City. Int J Cancer. 2009;125:1424–30.
Nishimoto IN, Hamada GS, Kowalski LP, Rodrigues JG, Iriya K, Sasazuki S, et al. Risk factors for stomach cancer in Brazil (I): a case-control study among non-Japanese Brazilians in Sao Paulo. Jpn J Clin Oncol. 2002;32:277–83.
Hamada GS, Kowalski LP, Nishimoto IN, Rodrigues JJ, Iriya K, Sasazuki S, et al. Risk factors for stomach cancer in Brazil (II): a case-control study among Japanese Brazilians in Sao Paulo. Jpn J Clin Oncol. 2002;32:284–90.
Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 1). J Epidemiol Community Health. 2006;60:7–12.
Burke DL, Ensor J, Riley RD. Meta-analysis using individual participant data: one-stage and two-stage approaches, and why they may differ. Stat Med. 2017;36:855–75.
Vansteelandt S, Bekaert M, Lange T. Imputation strategies for the estimation of natural direct and indirect effects. Epidemiol Methods. 2012;1. https://doi.org/10.1515/2161-962X.1014.
Steen J, Loeys T, Moerkerke B, Vansteelandt S. medflex: an R package for flexible mediation analysis using natural effect models. J Stat Softw. 2017;76:1–46.
van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2017;45:1–67.
Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons Inc; 1987.
Uemura N, Okamoto S, Yamamoto S, Matsumura N, Yamaguchi S, Yamakido M, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 2001;345:784–9.
Collatuzzo G, Pelucchi C, Negri E, Lopez-Carrillo L, Tsugane S, Hidaka A, et al. Exploring the interactions between Helicobacter pylori (Hp) infection and other risk factors of gastric cancer: a pooled analysis in the Stomach cancer Pooling (StoP) Project. Int J Cancer. 2021;149:1228–38.
Boffetta P. Infection with Helicobacter pylori and parasites, social class and cancer. IARC Sci Publ. 1997;(138):325–9.
Laszewicz W, Iwanczak F, Iwanczak B. Seroprevalence of Helicobacter pylori infection in Polish children and adults depending on socioeconomic status and living conditions. Adv Med Sci. 2014;59:147–50.
Eusebi LH, Zagari RM, Bazzoli F. Epidemiology of Helicobacter pylori infection. Helicobacter. 2014;19(Suppl 1):1–5.
Niv Y, Hazazi R. Helicobacter pylori recurrence in developed and developing countries: meta-analysis of 13C-urea breath test follow-up after eradication. Helicobacter. 2008;13:56–61.
Ocana-Riola R, Sanchez-Cantalejo C, Rosell J, Sanchez-Cantalejo E, Daponte A. Socio-economic level, farming activities and risk of cancer in small areas of Southern Spain. Eur J Epidemiol. 2004;19:643–50.
Kogevinas M, Pearce N, Susser M, Boffetta P. Social Inequalities and Cancer. IARC Science Publications No 138 Lyon: International Agency for Research on Cancer; 1997.
Shah SC, Boffetta P, Johnson KC, Hu J, Palli D, Ferraroni M, et al. Occupational exposures and odds of gastric cancer: a StoP project consortium pooled analysis. Int J Epidemiol. 2020;49:422–34.
Doubeni CA, Major JM, Laiyemo AO, Schootman M, Zauber AG, Hollenbeck AR, et al. Contribution of behavioral risk factors and obesity to socioeconomic differences in colorectal cancer incidence. J Natl Cancer Inst. 2012;104:1353–62.
Wang Z, Koh WP, Jin A, Wang R, Yuan JM. Composite protective lifestyle factors and risk of developing gastric adenocarcinoma: the Singapore Chinese Health Study. Br J Cancer. 2017;116:679–87.
Vari R, Scazzocchio B, D’Amore A, Giovannini C, Gessani S, Masella R. Gender-related differences in lifestyle may affect health status. Ann Ist Super Sanita. 2016;52:158–66.
Garcia-Mayor J, Moreno-Llamas A, la Cruz-Sanchez E. High educational attainment redresses the effect of occupational social class on health-related lifestyle: findings from four Spanish national health surveys. Ann Epidemiol. 2021;58:29–37.
La Vecchia C, Negri E, D’Avanzo B, Franceschi S. Electric refrigerator use and gastric cancer risk. Br J Cancer. 1990;62:136–7.
Ferro A, Morais S, Pelucchi C, Aragones N, Kogevinas M, Lopez-Carrillo L, et al. Smoking and Helicobacter pylori infection: an individual participant pooled analysis (Stomach Cancer Pooling- StoP Project). Eur J Cancer Prev. 2019;28:390–6.
Acknowledgements
We thank the European Cancer Prevention (ECP) Organization for providing support for the project meetings.
Funding
This study was funded by the Associazione Italiana per la Ricerca sul Cancro (AIRC), Project no. 21378 (Investigator Grant).
Author information
Authors and Affiliations
Contributions
Conceptualisation: GA, PB, GC, PB; Methodology: GA, PB, GC, PB; Data collection: LML, CSR, EN, DZ, JV, ST, GSH, LL-C, RUH-R, RM, Z-FZ, CLV; Formal analysis and investigation: GA, PB; Writing—original draft preparation: GA, PB; Writing—review and editing: All authors; Funding acquisition: CLV; Resources: CLV; Supervision: CLV, CP.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. The StoP Project received ethical approval from the University of Milan Institutional Review Board (reference no. 19/15 of 01/04/2015). Informed consent was obtained for each subject included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Alicandro, G., Bertuccio, P., Collatuzzo, G. et al. The mediating role of combined lifestyle factors on the relationship between education and gastric cancer in the Stomach cancer Pooling (StoP) Project. Br J Cancer 127, 855–862 (2022). https://doi.org/10.1038/s41416-022-01857-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01857-9
This article is cited by
-
Dose–response association between cigarette smoking and gastric cancer risk: a systematic review and meta-analysis
Gastric Cancer (2024)
-
Global burden of gastric cancer: epidemiological trends, risk factors, screening and prevention
Nature Reviews Clinical Oncology (2023)