Abstract
Background
We investigated whether associations between prevalent diabetes and cancer risk are pertinent to older adults and whether associations differ across subgroups of age, body weight status or levels of physical activity.
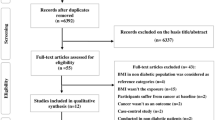
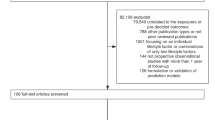
Methods
We harmonised data from seven prospective cohort studies of older individuals in Europe and the United States participating in the CHANCES consortium. Cox proportional hazard regression was used to estimate the associations of prevalent diabetes with cancer risk (all cancers combined, and for colorectum, prostate and breast). We calculated summary risk estimates across cohorts using pooled analysis and random-effects meta-analysis.
Results
A total of 667,916 individuals were included with an overall median (P25–P75) age at recruitment of 62.3 (57–67) years. During a median follow-up time of 10.5 years, 114,404 total cancer cases were ascertained. Diabetes was not associated with the risk of all cancers combined (hazard ratio (HR) = 0.94; 95% confidence interval (CI): 0.86–1.04; I2 = 63.3%). Diabetes was positively associated with colorectal cancer risk in men (HR = 1.17; 95% CI: 1.08–1.26; I2 = 0%) and a similar HR in women (1.13; 95% CI: 0.82–1.56; I2 = 46%), but with a confidence interval including the null. Diabetes was inversely associated with prostate cancer risk (HR = 0.81; 95% CI: 0.77–0.85; I2 = 0%), but not with postmenopausal breast cancer (HR = 0.96; 95% CI: 0.89–1.03; I2 = 0%). In exploratory subgroup analyses, diabetes was inversely associated with prostate cancer risk only in men with overweight or obesity.
Conclusions
Prevalent diabetes was positively associated with colorectal cancer risk and inversely associated with prostate cancer risk in older Europeans and Americans.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Chatterjee, S., Khunti, K. & Davies, M. J. Type 2 diabetes. Lancet 389, 2239–2251 (2017).
Zheng, Y., Ley, S. H. & Hu, F. B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 14, 88–98 (2018).
Ohkuma, T., Peters, S. A. E. & Woodward, M. Sex differences in the association between diabetes and cancer: a systematic review and meta-analysis of 121 cohorts including 20 million individuals and one million events. Diabetologia 61, 2140–2154 (2018).
Gouveri, E., Papanas, N. & Maltezos, E. The female breast and diabetes. Breast 20, 205–211 (2011).
Tsilidis, K. K., Kasimis, J. C., Lopez, D. S., Ntzani, E. E. & Ioannidis, J. P. A. Type 2 diabetes and cancer: umbrella review of meta-analyses of observational studies. BMJ 350, g7607 (2015).
Bansal, D., Bhansali, A., Kapil, G., Undela, K. & Tiwari, P. Type 2 diabetes and risk of prostate cancer: a meta-analysis of observational studies. Prostate Cancer Prostatic Dis. 16, 151–158 (2013). S1.
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A. & Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J. Clinicians. 68, 394–424 (2018).
Giovannucci, E., Harlan, D. M., Archer, M. C., Bergenstal, R. M., Gapstur, S. M., Habel, L. A. et al. Diabetes and cancer: a consensus report. CA Cancer J. Clin. 60, 207–221 (2010).
Lynch, B. M., Neilson, H. K. & Friedenreich, C. M. Physical activity and breast cancer prevention. Recent Results Cancer Res. 186, 13–42 (2011).
Steindorf, K., Ritte, R., Eomois, P.-P., Lukanova, A., Tjonneland, A., Johnsen, N. F. et al. Physical activity and risk of breast cancer overall and by hormone receptor status: the European prospective investigation into cancer and nutrition. Int. J. Cancer 132, 1667–1678 (2013).
Amadou, A., Hainaut, P. & Romieu, I. Role of obesity in the risk of breast cancer: lessons from anthropometry. J. Oncol. 2013, 906495 (2013).
Renehan, A. G., Tyson, M., Egger, M., Heller, R. F. & Zwahlen, M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371, 569–578 (2008).
Zhang, P., Li, H., Tan, X., Chen, L. & Wang, S. Association of metformin use with cancer incidence and mortality: a meta-analysis. Cancer Epidemiol. 37, 207–218 (2013).
Boffetta, P., Bobak, M., Borsch-Supan, A., Brenner, H., Eriksson, S., Grodstein, F. et al. The Consortium on Health and Ageing: Network of Cohorts in Europe and the United States (CHANCES) project–design, population and data harmonization of a large-scale, international study. Eur. J. Epidemiol. 29, 929–936 (2014).
Lai, G. Y., Park, Y., Hartge, P., Hollenbeck, A. R. & Freedman, N. D. The association between self-reported diabetes and cancer incidence in the. J. Clin. Endocrinol. Metab. 98, E497–E502 (2013).
Diagnostic Criteria and Classification of Hyperglycaemia First Detected in Pregnancy [Internet]. (WHO Guidelines Approved by the Guidelines Review Committee). http://www.ncbi.nlm.nih.gov/books/NBK169024/ (WHO, 2013).
FIN-EAS and FIN-WES: FINRISK Study [Internet]. https://www.thl.fi/publications/morgam/cohorts/full/finland/fin-fina.htm#dprocedure (2020).
Tsilidis, K. K., Papadimitriou, N., Capothanassi, D., Bamia, C., Benetou, V., Jenab, M. et al. Burden of Cancer In A Large Consortium Of Prospective Cohorts in Europe. J. Natl Cancer Inst. 108, https://academic.oup.com/jnci/article/108/10/djw127/2412485 (2016).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 7, 177–188 (1986).
Higgins, J. P. T. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
Dankner, R., Boffetta, P., Balicer, R. D., Boker, L. K., Sadeh, M., Berlin, A. et al. Time-dependent risk of cancer after a diabetes diagnosis in a cohort of 2.3 million adults. Am. J. Epidemiol. 183, 1098–1106 (2016).
Peila, R. & Rohan, T. E. Diabetes, glycated hemoglobin, and risk of cancer in the UK biobank study. Cancer Epidemiol. Biomark. Prev. 29, 1107–1119 (2020).
Ling, S., Brown, K., Miksza, J. K., Howells, L., Morrison, A., Issa, E. et al. Association of type 2 diabetes with cancer: a meta-analysis with bias analysis for unmeasured confounding in 151 cohorts comprising 32 million people. Diabetes Care. 43, 2313–2322 (2020).
Xu, H., Jiang, H., Ding, G., Zhang, H., Zhang, L., Mao, S. et al. Diabetes mellitus and prostate cancer risk of different grade or stage: a systematic review and meta-analysis. Diabetes Res. Clin. Pract. 99, 241–249 (2013).
Jayedi, A., Djafarian, K., Rezagholizadeh, F., Mirzababaei, A., Hajimohammadi, M. & Shab-Bidar, S. Fasting blood glucose and risk of prostate cancer: a systematic review and meta-analysis of dose-response. Diabetes Metab. 44, 320–327 (2018).
Au Yeung, S. L. & Schooling, C. M. Impact of glycemic traits, type 2 diabetes and metformin use on breast and prostate cancer risk: a Mendelian randomization study. BMJ Open Diabetes Res. Care 7, e000872 (2019).
Dankner, R., Boffetta, P., Keinan-Boker, L., Balicer, R. D., Berlin, A., Olmer, L. et al. Diabetes, prostate cancer screening and risk of low- and high-grade prostate cancer: an 11 year historical population follow-up study of more than 1 million men. Diabetologia 59, 1683–1691 (2016).
Larsson, S. C., Mantzoros, C. S. & Wolk, A. Diabetes mellitus and risk of breast cancer: a meta-analysis. Int. J. Cancer 121, 856–862 (2007).
Aune, D., Norat, T., Leitzmann, M., Tonstad, S. & Vatten, L. J. Physical activity and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis. Eur. J. Epidemiol. 30, 529–542 (2015).
Lee, J., Meyerhardt, J. A., Giovannucci, E. & Jeon, J. Y. Association between body mass index and prognosis of colorectal cancer: a meta-analysis of prospective cohort studies. PLoS ONE 10, e0120706 (2015).
Freisling, H., Arnold, M., Soerjomataram, I., O’Doherty, M. G., Ordonez-Mena, J. M., Bamia, C. et al. Comparison of general obesity and measures of body fat distribution in older adults in relation to cancer risk: meta-analysis of individual participant data of seven prospective cohorts in Europe. Br. J. Cancer 116, 1486–1497 (2017).
PJHL, Peeters, Bazelier, M. T., Leufkens, H. G. M., de Vries, F. & De Bruin, M. L. The risk of colorectal cancer in patients with type 2 diabetes: associations with treatment stage and obesity. Diabetes Care 38, 495–502 (2015).
Moe, B. & Nilsen, T. I. L. Cancer risk in people with diabetes: Does physical activity and adiposity modify the association? Prospective data from the HUNT Study, Norway. J. Diabetes Complicat. 29, 176–179 (2015).
Fall, K., Garmo, H., Gudbjornsdottir, S., Stattin, P. & Zethelius, B. Diabetes mellitus and prostate cancer risk; a nationwide case-control study within PCBaSe Sweden. Cancer Epidemiol. Biomark. Prev. 22, 1102–1109 (2013).
Vigneri, P., Frasca, F., Sciacca, L., Pandini, G. & Vigneri, R. Diabetes and cancer. Endocr. Relat. Cancer 16, 1103–1123 (2009).
Novosyadlyy, R., Lann, D. E., Vijayakumar, A., Rowzee, A., Lazzarino, D. A., Fierz, Y. et al. Insulin-mediated acceleration of breast cancer development and progression in a nonobese model of type 2 diabetes. Cancer Res. 70, 741–751 (2010).
Ward, P. S. & Thompson, C. B. Metabolic reprogramming: a cancer hallmark even Warburg did not anticipate. Cancer Cell. 21, 297–308 (2012).
Ryu, T. Y., Park, J. & Scherer, P. E. Hyperglycemia as a risk factor for cancer progression. Diabetes Metab. J. 38, 330–336 (2014).
Xu, C.-X., Zhu, H.-H. & Zhu, Y.-M. Diabetes and cancer: associations, mechanisms, and implications for medical practice. World J. Diabetes 5, 372–380 (2014).
Rastmanesh, R., Hejazi, J., Marotta, F. & Hara, N. Type 2 diabetes: a protective factor for prostate cancer? An overview of proposed mechanisms. Clin. Genitourin. Cancer 12, 143–148 (2014).
Lau, B., Cole, S. R. & Gange, S. J. Competing risk regression models for epidemiologic data. Am. J. Epidemiol. 170, 244–256 (2009).
Kowall, B., Stang, A., Rathmann, W. & Kostev, K. No reduced risk of overall, colorectal, lung, breast, and prostate cancer with metformin therapy in diabetic patients: database analyses from Germany and the UK. Pharmacoepidemiol. Drug Saf. 24, 865–874 (2015).
Feng, Z., Zhou, X., Liu, N., Wang, J., Chen, X. & Xu, X. Metformin use and prostate cancer risk: a meta-analysis of cohort studies. Medicine 98, e14955 (2019).
Qiu, S., Cai, X., Wu, T., Sun, Z., Guo, H., Kirsten, J. et al. Objectively-measured light-intensity physical activity and risk of cancer mortality: a meta-analysis of prospective cohort studies. Cancer Epidemiol. Biomark. Prev. 29, 1067–1073 (2020).
Dallal, C. M., Brinton, L. A., Matthews, C. E., Lissowska, J., Peplonska, B., Hartman, T. J. et al. Accelerometer-based measures of active and sedentary behavior in relation to breast cancer risk. Breast Cancer Res. Treat. 134, 1279–1290 (2012).
Dohrn, I.-M., Welmer, A.-K. & Hagströmer, M. Accelerometry-assessed physical activity and sedentary time and associations with chronic disease and hospital visits—a prospective cohort study with 15 years follow-up. Int. J. Behav. Nutr. Phys. Act. 16, 125 (2019).
Acknowledgements
Where authors are identified as personnel of the International Agency for Research on Cancer/World Health Organization, the authors alone are responsible for the views expressed in this paper and they do not necessarily represent the decisions, policy or views of the International Agency for Research on Cancer/World Health Organization.
Author information
Authors and Affiliations
Contributions
A.A., H.F., M.J. and I.R. conceived and designed the work. A.A. performed data analysis. I.R. and H.F. contributed to data analysis. K.K.T., A.T., P.B., B.V.G., O.M., T.W., F.K., B.S., J.M.O.M., S.M., S.S., R.C.H.V., J.R.Q., L.M.M., R.S., K.K. and H.B. acquired the data, and all authors played an important role in interpreting the results. A.A., H.F., M.J. and I.R. drafted the paper. K.K.T., A.T., P.B., B.V.G., O.M., T.W., F.K., B.S., J.M.O.M., S.M., S.S., R.C.H.V., J.R.Q., L.M.M., R.S., K.K. and H.B. revised the paper. All authors approved the final version of the paper and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. H.F. had full access to the data in the study and final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All studies participating in CHANCES were conducted in accordance with the Declaration of Helsinki. For each study, investigators satisfied the local requirements for ethical research, including obtaining informed consent from participants.
Consent to publish
Not applicable.
Data availability
The CHANCES participating cohorts’ data are available only to the collaborating scientists from the respective CHANCES participating centres. The data may be available upon request for some of the participating centres but not for all due to relevant data protection laws.
Competing interests
The authors declare no competing interests.
Funding information
Data used throughout the present study are derived from the CHANCES project. The project is coordinated by the Hellenic Health Foundation, Greece. The project received funding by the FP7 framework programme of DG-RESEARCH in the European Commission (grant agreement no. HEALTH-F3-2010-242244). EPIC Greece: funded by the Hellenic Health Foundation. EPIC Netherlands: funded by European Commission (DG SANCO), Dutch Ministry of Public Health, Welfare and Sports (VWS), The National Institute for Public Health and the Environment, the Dutch Cancer Society, the Netherlands Organisation for Health Research and Development (ZONMW) and World Cancer Research Fund (WCRF). EPIC Spain: supported by Health Research Fund (FIS) of the Spanish Ministry of Health RTICC ‘Red Temática de Investigación Cooperativa en Cáncer (grant numbers: Rd06/0020/0091 and Rd12/0036/0018), Regional Governments of Andalucía, Asturias, Basque Country, Murcia (project 6236) and Navarra, Instituto de Salud Carlos III, Redes de Investigacion Cooperativa (RD06/0020). EPIC Umea: funded by Region Västerbotten and the Swedish Research Council. ESTHER: funded by the Baden-Württemberg State Ministry of Science, Research and Arts (Stuttgart, Germany), the Federal Ministry of Education and Research (Berlin, Germany) and the Federal Ministry of Family Affairs, Senior Citizens, Women and Youth (Berlin, Germany). Data from FINRISK, Belfast and Northern Sweden were harmonised for this analysis in the MOnica Risk, Genetics, Archiving and Monograph (MORGAM) Project. The activities of the MORGAM Data Centre have been sustained also by recent funding from European Union FP7 project BiomarCaRE (HEALTH-F2-2011-278913). PRIME Belfast: supported by grants from the Institut National de la Santé et de la Recherche Médicale (INSERM), the Merck, Sharp & Dohme-Chibret Laboratory and the Northern Ireland Health & Social Care Research and Development Office. Northern Sweden MONICA Study: funded by Umeå University and the county councils of Norr and Västertbotten. Tromsø: funded by UiT The Arctic University of Norway, the National Screening Service and the Research Council of Norway. This study was in part funded by the World Cancer Research Fund (WCRF UK) as part of the World Cancer Research Fund International grant programme (IIG_2019_1978, Principal Investigator, Heinz Freisling).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Amadou, A., Freisling, H., Jenab, M. et al. Prevalent diabetes and risk of total, colorectal, prostate and breast cancers in an ageing population: meta-analysis of individual participant data from cohorts of the CHANCES consortium. Br J Cancer 124, 1882–1890 (2021). https://doi.org/10.1038/s41416-021-01347-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-021-01347-4
This article is cited by
-
Prevalence of diabetes mellitus among 80,193 gastrointestinal cancer patients in five European and three Asian countries
Journal of Cancer Research and Clinical Oncology (2022)