Abstract
Background
Trastuzumab–emtansine (T-DM1), one of the most potent HER2-targeted drugs, shows impressive efficacy in patients with HER2-positive breast cancers. However, resistance inevitably occurs and becomes a critical clinical problem.
Methods
We modelled the development of acquired resistance by exposing HER2-positive cells to escalating concentrations of T-DM1. Signalling pathways activation was detected by western blotting, gene expression was analysed by qRT-PCR and gene copy numbers were determined by qPCR. The role of Yes on resistance was confirmed by siRNA-mediated knockdown and stable transfection-mediated overexpression. The in vivo effects were tested in xenograft model.
Results
We found that Yes is overexpressed in T-DM1–resistant cells owing to amplification of chromosome region 18p11.32, where the YES1 gene resides. Yes activated multiple proliferation-related signalling pathways, including EGFR, PI3K and MAPK, and led to cross-resistance to all types of HER2-targeted drugs, including antibody-drug conjugate, antibody and small molecule inhibitor. The outcome of this cross-resistance may be a clinically incurable condition. Importantly, we found that inhibiting Yes with dasatinib sensitised resistant cells in vitro and in vivo.
Conclusions
Our study revealed that YES1 amplification conferred resistance to HER2-targeted drugs and suggested the potential application of the strategy of combining HER2 and Yes inhibition in the clinic.
Similar content being viewed by others
Background
HER2 is amplified in up to 20% of primary breast cancers and is associated with poor patient prognosis.1 Monoclonal antibodies that target HER2, such as trastuzumab and pertuzumab, as well as small molecule kinase inhibitors, such as lapatinib and neratinib, which target both HER2 and EGFR, have been approved by the Food and Drug Administration (FDA) for the treatment of HER2-positive cancer.2 However, despite initial responses to these agents, acquired resistance almost universally develops.3
The development of trastuzumab–emtansine (T-DM1), an antibody-drug conjugate (ADC) comprising trastuzumab and the antimicrotubule maytansinoid drug emtansine (DM1), brought new hope for HER2-positive patients. T-DM1 possesses the biological properties of trastuzumab, namely HER2-signaling inhibition and antibody-dependent cell-mediated cytotoxicity, as well as the antimicrotubule activity of DM1.4 T-DM1 has been reported to overcome resistance to trastuzumab5 and lapatinib6 in HER2-amplified cancer cells, and was approved for HER2-positive metastatic breast cancer by the FDA based on the phase III EMILIA trial (NCT00829166).7,8
However, although T-DM1 produces enormous clinical benefits, some patients do not respond to the drug or ultimately develop acquired resistance.9 Identified mechanisms of T-DM1 resistance include defects in T-DM1 binding,10 trafficking11,12 and microtubule dynamics.13,14 These resistance factors play a critical role in the effects of T-DM1, but not those of non-ADC anti-HER2 drugs, and thus may be overcome by other HER2-targeted drugs. Indeed, we have reported that lapatinib overcomes T-DM1 resistance in a cell line with impaired lysosomal proteolytic degradation of T-DM1.11 However, beyond that, cross-resistance mechanisms of T-DM1 with other HER2-targeted drugs, which may lead to an incurable clinical condition, are poorly characterised. Therefore, a better understanding of T-DM1-resistance mechanisms, especially of cross-resistance mechanisms, is particularly important.
In this study, which is part of our continuing effort to address the problem of resistance to HER2-targeted drugs,11,15,16 we found that the non-receptor tyrosine kinase Yes is overexpressed in a cell line with acquired resistance to T-DM1 owing to amplification of chromosome region 18p11.32, where YES1 gene resides. Notably, this overexpression of Yes conferred cross-resistance to all types of HER2-targeted drugs. We further suggest the possible therapeutic strategy of combining HER2 with Yes inhibition for overcoming resistance to HER2-targeted drugs.
Methods
Reagents and antibodies
T-DM1 and trastuzumab were purchased from F. Hoffmann-La Roche (Basel, Switzerland). Gefitinib, AZD4547, crizotinib, sunitinib, imatinib, dasatinib, PD 0325901 and GDC-0941 were purchased from Selleck Chemicals (Houston, TX, USA). DM1 was purchased from Meilunbio Inc. (Dalian, China). T-DM1 and trastuzumab were dissolved in saline, and small molecule compounds were dissolved in dimethyl sulfoxide. Lyso-Tracker Deep Red and DyLight 488 NHS ester were purchased from Thermo-Fisher Scientific (Waltham, MA, USA). Sulforhodamine B and the antibody against β-tubulin were purchased from Sigma–Aldrich (St. Louis, MO, USA). Antibodies against phospho-HER2 (Tyr1221/1222), HER2, phospho-EGFR (Tyr845), EGFR, phospho-HER3 (Tyr1289), HER3, phospho-Met (Tyr1234/1235), phospho-IGF-IR (Tyr1135/1136)/IR (Tyr1150/1151), phospho-Akt (Ser473), phospho-Erk1/2 (Thr202/Tyr204), phospho-PTEN (Ser380/Thr382/383), PTEN, phospho-Src family kinase (Tyr416), c-Src, Yes, Fyn, Lyn, Lck, Csk and PARP were purchased from Cell Signaling Technology (Beverly, MA, USA). Antibodies against Erk1/2, p27, TYMS, and THOC1 were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA).
Cell culture and treatment
The human BT-474 and SK-OV-3 cell lines were obtained from the American Type Culture Collection (Manassas, VA, USA) and were cultured according to the instructions provided. Acquired T-DM1-resistant cells (BT-474/R1-7) were established by exposing parental BT-474 cells to increasing concentrations of T-DM1 (from 10 ng/mL to 1 μg/mL) for 12 months and selecting clones using the limiting dilution method. BT-474 and SK-OV-3 cells expressing YES1 Y537F and YES1 WT were generated by transfecting cells with the YES1 Y537F (Addgene plasmid #51299)17 and YES1 WT (generated by point mutation from YES1 Y537F plasmid) plasmids, respectively.
Lentiviral overexpression
YES1 Y537F or YES1 WT together with psPAX2 and pMD2G plasmids were transfected into HEK293FT cells in a 4:3:1 ratio using Lipofectamine 2000 (Thermo-Fisher Scientific, Waltham, MA, USA). Lentiviral supernatants were harvested after 48 and 72 h. BT-474 and SK-OV-3 cells were transfected with lentiviral supernatants at 37 °C. 24 h later, the viral supernatants were removed and cells were cultured in the presence of blasticidin (BT-474: 20 μg/ml; SK-OV-3: 10 μg/ml) for 7 days.
Cell proliferation assay
Cells were treated with different concentrations of drugs, alone or in combination, as indicated, inhibition rates were determined using sulforhodamine B assays and 50% growth-inhibition concentration (IC50) was calculated using GraphPad Prism software, as described previously.18
Western blotting
Western blotting was performed using standard procedures, as described previously.19 Briefly after drug treatment, cells were harvested and cell lysates were separated by SDS–PAGE and transferred to polyvinylidene difluoride membranes. After blocking in 5% nonfat milk in TBST (Tris-buffered saline containing 0.1% Tween-20, pH 7.6), membranes were incubated with primary and secondary antibodies. Immunoreactive proteins were visualised using the enhanced chemiluminescence system from Thermo-Fisher Scientific (Waltham, MA, USA). Results were quantified by densitometry and normalised to corresponding total protein (for phosphorylated protein) or β-tubulin control.
Binding and endocytosis assay
Binding and endocytosis assays were performed as described previously.15 For binding assay, cells were incubated with DyLight 488 NHS-ester-linked T-DM1 on ice for 1 h. For endocytosis assay, cells were incubated with DyLight 488 NHS-ester-linked T-DM1 at 37 °C for different indicated time and subsequently stripped using a stripping buffer (0.05 mol/L glycine, 0.1 mol/L NaCl, pH 2.45). Fluorescence was finally analysed by flow cytometry.
Fluorescence microscopy
Cells were incubated with DyLight 488 NHS-ester-linked T-DM1 for 23 h at 37 °C and the lysosome fluorescent probe Lyso-Tracker Red was added for another 1 h. Alternatively, cells were incubated with Lyso-Tracker Red for 1 h at 37 °C, then incubated with DyLight 488 NHS-ester-linked T-DM1 for 10 min at 4 °C. Cells were fixed with 4% paraformaldehyde for 15 min and imaged with an Olympus FV1000 confocal microscope.
Polymeric tubulin fraction assay
Cells was lysed with a buffer consisting of 80 mmol/L MES-KOH (pH 6.8), 1 mmol/L MgC12, 1 mmol/L EGTA, 0.1% Triton X-100 and 10% glycerol for 3 min at 30 °C, and detergent-insoluble polymerised cytoskeleton was analysed by western blotting.
In vivo study
BT-474/R1-7 tumour models were established by subcutaneous inoculation of BT-474/R1-7 cells into female Balb/cA-nude mice (5–6 weeks old, purchased from Shanghai SLAC Laboratory Animal Co. Ltd), and SK-OV-3/YES1 Y537F tumour models were established by subcutaneous inoculation of SK-OV-3/YES1 Y537F cells into female NCG mice (5–6 weeks old, purchased from Jiangsu GemPharmatech Co. Ltd). Animals were bred in specific-pathogen-free environment under standard conditions (temperature: 22 ± 1 °C; dark/light cycle: 12/12 h; humidity: 60 ± 10%; cage: plastic, sterile, with filter; cage companions: max 6 animals/cage; bedding material: high-adsorbing bedding material without dust). Tumour diameter was measured by vernier calliper. When tumours reached a volume of 100–300 mm3, mice were randomised into control (n = 10) or treatment (n = 6) groups and treated with drugs. Control group: saline, 10 mL/kg, intravenous (i.v.), day 0, 7, 14, 29 (BT-474/R1-7) or day 0, 7, 20 (SK-OV-3/YES1 Y537F). T-DM1 group: 3 mg/kg, i.v., day 0, 7, 14, 29 (BT-474/R1-7) or day 0, 7, 20 (SK-OV-3/YES1 Y537F). Dasatinib group: 3 mg/kg, intragastric (i.g.), once a day. Combination group: T-DM1 (described above) plus dasatinib (described above). T-DM1 was diluted in saline and dasatinib was diluted in citric acid buffer (0.1% Tween 80, pH4.6). Tumour volume was calculated as (length × width2)/2, and body weight was monitored as an indicator of general health twice a week. Mice were euthanised by cervical dislocation at the end of the experiments (24 h after the last dose of T-DM1 and 4 h after the last dose of dasatinib), and the tumours were resected and frozen in liquid nitrogen. Tumour growth inhibition (%) was calculated as 100 − (Tt − T0)/(Ct − C0) × 100, where Tt is the mean volume of treated tumour at time t, T0 is the mean tumour volume immediately prior to treatment (time 0), Ct is the mean tumour volume of controls at time t, and C0 is the mean tumour volume in controls at time 0. Animal experiments were carried out in accordance with guidelines of the Institutional Animal Care and Use Committee at the Shanghai Institute of Materia Medica, Chinese Academy of Sciences.
Statistical analysis
Data were analysed using GraphPad Prism software. Two-tailed Student’s t-tests were used to determine the statistical significance of differences between two groups. A p-value < 0.05 was considered statistically significant.
Additional methods
Methods for siRNA transfection, RNA isolation, quantitative reverse transcription-PCR (qRT-PCR) and qPCR are provided in Supplementary Material.
Results
BT-474/R1-7 cells are resistant to HER2-targeted drugs
To investigate the molecular mechanism of T-DM1 resistance, we established T-DM1–resistant clone BT-474/R1-7 from the HER2-positive breast cancer cell line BT-474 following repeated treatment with T-DM1. The degree of T-DM1 resistance in BT-474/R1-7 cells was evaluated using cell-growth assays. As shown in Fig. 1a, the IC50 value of T-DM1 in BT-474/R1-7 cells was ~22-fold higher than that in BT-474 cells, indicating significant resistance to T-DM1. We also investigated the sensitivity of BT-474/R1-7 cells to other HER2-targeted drugs, including the antibody drugs trastuzumab and pertuzumab, and the small molecule inhibitors lapatinib and neratinib, and found that BT-474/R1-7 cells were significantly resistant to either drug alone or the combination of trastuzumab and pertuzumab (Fig. 1a). These data suggest that BT-474/R1-7 cells are resistant to different types of HER2-targeted drugs, including antibodies, ADCs and small molecule inhibitors.
a Cells were treated with different concentrations of T-DM1, trastuzumab, pertuzumab, lapatinib, neratinib or the combination of trastuzumab and pertuzumab for 120 h, after which cell survival was measured using sulforhodamine B assays. IC50 was exhibited close to the corresponding dose-response curve. Data shown represent means ± SD of three independent experiments. b HER2 levels were determined by western blotting. c, d Cells were incubated with DyLight 488 NHS-ester–labelled T-DM1 (1 μg/mL) on ice for 1 h (c), or at 37 °C for the indicated times, followed by quenching of surface fluorescence with stripping buffer (d). Mean fluorescence intensity (MFI) was determined by flow cytometry. e Cells were incubated with DyLight 488 NHS-ester–labelled T-DM1 (1 μg/mL, green), and lysosomes were labelled with Lyso-Tracker (100 nM, Red). Samples were visualised by confocal microscopy. Colour figures were shown in html full text version. f Cells were treated with T-DM1 for 48 h, after which polymeric tubulin was examined by western blotting.
HER2 expression, T-DM1 trafficking and microtubule dynamics are not changed in BT-474/R1-7 cells
Normally, T-DM1 binds to HER2, is endocytosed into cells and releases DM1 through proteolytic degradation, ultimately leading to inhibition of microtubule assembly.20 Because factors that affect these processes may play a role in T-DM1 resistance,20 we first investigated HER2 expression and T-DM1 drug-release processes in BT-474/R1-7 cells. We found that HER2 levels (Fig. 1b, Supplementary Fig. 1a), as well as T-DM1 binding (Fig. 1c), endocytosis (Fig. 1d) and location (Fig. 1e), were not changed in BT-474/R1-7 cells. We then assessed inhibition of microtubule polymerisation, a critical outcome elicited by DM1-containing catabolites. As shown in Fig. 1f and Supplementary Fig. 1b, T-DM1 caused a concentration-dependent inhibition of tubulin polymerisation in BT-474/R1-7 cells, indicating that microtubule dynamics and the release of DM1-containing catabolites through proteolytic degradation were also not defective in BT-474/R1-7 cells. Taken together, these results suggest that HER2 expression, T-DM1 trafficking and microtubule dynamics are not changed, and are thus not the cause of T-DM1 resistance in BT-474/R1-7 cells.
Src family kinases play a critical role in drug resistance in BT-474/R1-7 cells
HER2-targeted drugs inhibit several proliferation-related signalling pathways in HER2-positive cells, and compensatory activation of such signalling pathways may lead to resistance. Accordingly, we next examined the status of signalling proteins in BT-474/R1-7 cells. As shown in Fig. 2a and Supplementary Fig. 1c, phosphorylation of HER2, HER3, c-Met, IGF-IR, IR and PTEN were not changed, but phosphorylation of EGFR, Akt, Erk1/2 and Src family kinases (SFKs) were significantly increased in BT-474/R1-7 cells. Moreover, the inhibitory effects of HER2-targeted drugs on the phosphorylation of signalling proteins in BT-474 cells were almost lost in BT-474/R1-7 cells (Fig. 2b and Supplementary Fig. 1d), suggesting that reprogramming of these signalling pathways may be a mechanism of acquired resistance. To determine the identity of the aberrantly activated signalling protein that lies upstream in this mechanism, we tested various inhibitors for their ability to suppress activation of all signalling proteins. As shown in Fig. 2c and Supplementary Fig. 1e, dasatinib, which mainly targets SFKs and Abl, and also inhibits Arg, c-Kit and PDGFR,21 inhibited all activated signalling proteins (SFK, EGFR, Akt and Erk1/2) in BT-474/R1-7 cells, an effect that was concentration dependent (Fig. 2d and Supplementary Fig. 1f). However, imatinib, an inhibitor of Abl, Arg, c-Kit and PDGFR, but not SFKs,22 had no inhibitory effects on these proteins. Besides, gefitinib (EGFR inhibitor) inhibited phosphorylation of EGFR, and its downstream signalling proteins (Akt and Erk1/2), but not phosphorylation of SFKs; GDC-0941 (PI3K inhibitor) and PD 0325901 (MEK inhibitor) only inhibited their respective signalling without affecting other signalling tested. These results suggested that SFK is the most upstream signalling element in the cascade of aberrantly activated signalling proteins in BT-474/R1-7 cells. We then investigated the role of SFK in the unresponsiveness of BT-474/R1-7 cells to the effects of HER2-targeted drugs. As shown in Fig. 2e and Supplementary Fig. 1g, dasatinib decreased aberrant activation of all signalling proteins in this cascade, and restored the inhibitory effects of HER2-targeted drugs. We further explored the role of SFKs in drug resistance using proliferation assays. In contrast to their resistance to HER2-targeted drugs, BT-474/R1-7 cells were significantly more sensitive to dasatinib than BT-474 cells (Fig. 2f). Moreover, a low concentration of dasatinib (30 nM) considerably sensitised BT-474/R1-7 cells to HER2-targeted drugs (Fig. 2g). To further explore the mechanism of cell death, we then tested p27, a marker of cell-cycle arrest, and cleaved PARP, a marker of apoptosis, in BT-474/R1-7 cells. As shown in Fig. 2h and Supplementary Fig. 1h, when combined with dasatinib, T-DM1 induced a more obvious increase of p27 and cleaved PARP, indicating that a stronger cell-cycle arrest and subsequent apoptosis was induced by this combination. Collectively, these results suggest that SFKs, primary targets of dasatinib, play a critical role in drug resistance in BT-474/R1-7 cells.
a Signalling proteins in BT-474 and BT-474/R1-7 cells were determined by western blotting. b–e BT-474/R1-7 cells were treated with the indicated inhibitors (T-DM1 and trastuzumab: 1 μg/mL; DM1: 30 nM; lapatinib: 300 nM; other inhibitors: 1 μM or used as indicated) for 2 h, after which the phosphorylation status of signalling proteins was determined by western blotting. f, g BT-474 and BT-474/R1-7 cells were treated with different concentrations of inhibitors alone or combined with dasatinib (30 nM) for 120 h, after which cell survival was measured using sulforhodamine B assays. Data shown represent means ± SD of three independent experiments. h BT-474/R1-7 cells were treated with the indicated inhibitors for 36 or 72 h, after which proteins were determined by western blotting.
Yes, but not c-Src, is responsible for activation of signalling pathways in BT-474/R1-7 cells
The SFK family comprises nine members—c-Src, Yes, Fyn, Lyn, Lck, Fgr, Blk, Hck and Yrk—that share similar structure and function.23 c-Src, Yes and Fyn are expressed ubiquitously, whereas the other SFKs are more or less tissue specific.24 To identify the specific SFK involved in the resistance to T-DM1, we determined the levels of individual SFK members in BT-474/R1-7 cells. As shown in Fig. 3a and Supplementary Fig. 2a, Yes expression was significantly increased in BT-474/R1-7 cells (P < 0.001), but the expression of other SFK members (c-Src, Fyn, Lyn and Lck) and Csk, a kinase that negatively regulates SFKs, were largely unchanged. To explore the role of Yes in resistance, we transfected BT-474/R1-7 cells with three independent small interfering RNAs (siRNAs) targeting Yes and assessed aberrant activation of SFK, EGFR, Akt and Erk1/2 signalling pathways. As shown in Fig. 3b and Supplementary Fig. 2b, Yes knockdown selectively inhibited Yes expression (p < 0.01) and significantly inhibited all activated signalling proteins (SFK, EGFR, Akt and Erk1/2), suggesting that Yes overexpression is the upstream event in the aberrant activation of these signalling pathways. Because c-Src is the predominant member of SFKs, and has been considered the common node of trastuzumab resistance,25 we also knocked down c-Src using siRNAs. As shown in Fig. 3b, c-Src knockdown decreased c-Src expression to a low level, but had no discernible effects on activation of SFK, EGFR, Akt or Erk1/2, suggesting that c-Src is not involved in aberrant signalling pathway activation in BT-474/R1-7 cells. Collectively, these results highlight a critical role for Yes in mediating drug resistance.
Chromosome region 18p11.32 is amplified in BT-474/R1-7 cells
To understand the mechanism underlying Yes overexpression, we further examined Yes expression at the mRNA level. As shown in Fig. 4a, YES1 mRNA was dramatically increased (~46-fold, p < 0.0001) in BT-474/R1-7 cells, whereas mRNAs of other SFK members (SRC, FYN, LYN, BLK, HCK and FGR) were largely unchanged. A further examination of DNA copy number showed that the YES1 gene was significantly amplified (~22-fold, p < 0.0001) in BT-474/R1-7 cells (Fig. 4b), suggesting that Yes overexpression is attributable to changes at the genomic level. Because gene amplification usually occurs in the form of an increase in the copy number of a chromosome region,26 we further analysed whether other genes located near YES1 were amplified in BT-474/R1-7 cells. This analysis showed that the copy numbers of seven genes—THOC1, COLEC12, CETN1, CLUL1, TYMS, ENOSF1 and ADCYAP1—in the 18p11.32 region of chromosome 18 were significantly amplified (Fig. 4b). A further examination of the expression of these genes at mRNA and protein levels showed that CLUL1, TYMS and ENOSF1 mRNA levels were also significantly increased (Fig. 4c), and confirmed TYMS overexpression at the protein level (Fig. 4d and Supplementary Fig. 2, c). We then asked whether overexpression of these genes was associated with drug resistance. To this end, we knocked down CLUL1, TYMS, ENOSF1 or YES1 using two independent siRNAs for each, and determined whether the resulting knockdown sensitised BT-474/R1-7 cells to T-DM1 treatment. Because TYMS is the target for the chemotherapeutic agent 5-fluorouracil (5-FU), we also assessed the effects of 5-FU on resistance to T-DM1. These analyses showed that only YES1 knockdown reversed T-DM1 resistance in BT-474/R1-7 cells (Fig. 4e); siRNA-mediated knockdown of TYMS or inhibition with 5-FU exerted inhibitory effects on cell growth as broad cytotoxic drugs did, but these treatments did not reverse T-DM1 resistance (Fig. 4e, f and Supplementary Fig. 3). Thus, among the amplified genes in the 18p11.32 region, YES1 is the critical gene for T-DM1 resistance.
mRNA levels of SFK members (a) and other genes in the 18p11.32 region (c) were analysed by qRT-PCR. b Copy numbers of genes on chromosome 18 were analysed by qPCR. d Protein levels of TYMS and THOC1 were determined by western blotting. e BT-474/R1-7 cells were transfected with siRNAs for 24 h, and then treated with T-DM1 for an additional 120 h. f BT-474/R1-7 cells were treated with different concentrations of 5-FU, with or without T-DM1 (300 ng/mL), for 120 h. Cell survival in e, f was measured using sulforhodamine B assays. Data shown represent means ± SD (error bars) from triplicates (**p < 0.01).
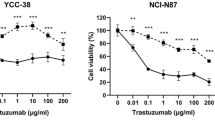
Ectopic expression of Yes confers resistance to HER2-targeted drugs
To determine whether Yes activation is sufficient to confer resistance to HER2-targeted drugs, we stably transfected BT-474 breast cancer cells (parental cells of BT-474/R1-7) and SK-OV-3 ovarian cancer cells (to assess cell specificity) with wild-type YES1 (WT) or constitutively active YES1 (Y537F), and analysed resistance to the HER2-targeted drugs. Transfection of YES1 WT and YES1 Y537F led to similar protein levels of Yes in both BT-474 and SK-OV-3 cell models, but YES1 Y537F led to a stronger activation of signalling proteins (Fig. 5a and Supplementary Fig. 2d). Although ectopic expression of Yes in BT-474 cells did not achieve equivalent level as that in BT-474/R1-7 cells, activation of signalling proteins in BT-474/YES1 Y537F cells was comparable to that in BT-474/R1-7 cells. YES1 WT and YES1 Y537F conferred cell resistance to all HER2-targeted drugs tested (T-DM1, trastuzumab and lapatinib), and the resistance caused by YES1 Y537F was stronger (Fig. 5b, c). We further examined whether dasatinib was capable of reversing resistance to these HER2-targeted drugs in these cell models as it did in BT-474/R1-7 cells. As shown in Fig. 5d and e, dasatinib treatment sensitised resistant cells to HER2-targeted drugs in both cell models. Collectively, these observations indicate that Yes amplification confers resistance to HER2-targeted drugs, and the resistance level mainly depends on the activation degree of Yes.
a Signalling proteins in indicated cells were determined by western blotting. BT-474, BT-474/YES1 WT and BT-474/YES1 Y537F cells (b), and SK-OV-3, SK-OV-3/YES1 WT and SK-OV-3/YES1 Y537F cells (c), were treated with different concentrations of T-DM1, trastuzumab or lapatinib for 120 h, after which cell survival was measured using sulforhodamine B assays. BT-474/YES1 Y537F (d) and SK-OV-3/YES1 Y537F (e) cells were treated with different concentrations of the HER2-targeted inhibitors, T-DM1 or lapatinib, for 120 h, with or without dasatinib (30 nM), after which cell survival was measured using sulforhodamine B assays. Data shown represent means ± SD of three independent experiments.
Yes inhibition overcomes T-DM1 resistance in vivo
Finally, to extend these in vitro findings to an in vivo setting, we performed xenograft studies. As shown in Fig. 6a, mono-treatment with either T-DM1 (3 mg/kg, n = 6) or dasatinib (3 mg/kg, n = 6) led to only modest inhibition of tumour growth (45.4 ± 15.7% and 27.6 ± 22.6%, respectively) in nude mice bearing BT-474/R1-7 xenografts, whereas combined treatment with both agents (n = 6) significantly improved tumour growth inhibition (89.2 ± 6.1%). In SK-OV-3/YES1 Y537F model, T-DM1 plus dasatinib led to a significant shrinkage of tumours (69.3 ± 1.7%, n = 6), whereas T-DM1 (3 mg/kg, n = 6) or dasatinib (3 mg/kg, n = 6) alone was not so effective (47.4 ± 5.5% and 30.1 ± 4.3%, respectively) (Fig. 6b). Moreover, no apparent toxicity was observed in either model (Fig. 6a, b). We further found that activation (phosphorylation) of the signalling proteins SFK, EGFR, Akt and Erk1/2 was significantly decreased and p27 was significantly increased by combinatorial treatment in BT-474/R1-7 xenografts, as shown in Fig. 6c and Supplementary Fig. 2e. Collectively, these results suggest that Yes inhibition by dasatinib sensitises BT-474/R1-7 and SK-OV-3/YES1 Y537F tumours to T-DM1 in vivo.
Mice bearing BT-474/R1-7 (a) or SK-OV-3/YES1 Y537F (b) xenograft tumours were treated with T-DM1, dasatinib, or a combination of T-DM1 and dasatinib. Tumour volumes (top) and body weights (bottom) were measured on the indicated days. Data shown represent means ± SD (error bars; control group, n = 10 or treatment groups, n = 6; *p < 0.05, **p < 0.01, ****p < 0.0001). c BT-474/R1-7 xenograft tumours were isolated, then signalling proteins were determined by western blotting. d Proposed model of T-DM1 resistance in BT-474/R1-7 cells.
Discussion
T-DM1 is a powerful HER2-targeted ADC that demonstrates remarkable efficacy in the clinic. However, after long-term treatment with this highly specific, targeted agent, tumour cells inevitably become reprogrammed so as to sustain cell survival.25 Here, we discovered that in a cell line incubated long term with T-DM1, Yes was overexpressed owing to amplification of chromosome region 18p11.32. Increased activated Yes subsequently activated multiple proliferation-related signalling pathways, and thereby conferred cross-resistance to HER2-targeted drugs (Fig. 6d). Notably, we demonstrated that inhibition of Yes with dasatinib reversed this resistance both in vitro and in vivo (Fig. 6d). These findings uncover a novel mechanism of T-DM1 resistance and provide a valuable reference for the development of rational strategies for overcoming resistance to HER2-targeted drugs in the clinic.
The tyrosine kinase Yes, encoded by the YES1 gene, is a member of the SFK family. In addition to Yes, there are eight other highly homologous members of the SFK family, namely c-Src, Fyn, Lyn, Lck, Fgr, Blk, Hck and Yrk.23 SFKs activate multiple signalling proteins, including EGFR,27 PI3K/Akt, Ras/MAPK, FAK, RhoA, cortactin, p130CAS, paxillin, tensin-3, p27 and Bcl-2,28 and modulate a number of biological functions, such as cell proliferation, survival, differentiation, migration, invasion, adhesion, angiogenesis and immune cell function.29 Although the transforming ability of Yes has not been fully studied, some miRNAs were shown to regulate tumour progression via YES1 regulation.30,31 Recently, a novel Yes inhibitor CH6953755 (more specific for Yes than other SFKs) was generated and showed potent antitumour activity against YES1-amplified cancers in vitro and in vivo.32 In this study, we found that phosphorylation of SFK, EGFR, Akt and Erk1/2 were significantly increased in YES1-amplified BT-474/R1-7 cells, and could be inhibited by dasatinib or siRNAs targeting Yes. Moreover, ectopic expression of Yes in different cancer cells led to resistance to HER2-targeted drugs. These results add evidences to YES1 as an independent oncogene among SFK family members.
c-Src, the most studied SFK, has been implicated in conferring resistance to many targeted therapies, such as anti-EGFR therapies in lung cancer,33 antiandrogen therapies in prostate cancer,34 as well as anti-HER2 therapies (trastuzumab)25 and antioestrogen therapies35 in breast cancer. c-Src also modulates sensitivity to chemotherapeutic drugs, such as the antimicrotubule agent paclitaxel.36,37 Whereas c-Src has been extensively studied in the context of acquired drug resistance, comparatively less is known about Yes-induced drug resistance. It has been reported that YES1 is amplified in clinical cases of acquired resistance to EGFR inhibitors38 and in osimertinib-induced resistant cell lines,39 but this conclusion was not directly confirmed by ectopically overexpressing Yes. We report here for the first time that Yes is overexpressed in breast cancer cells with acquired resistance to T-DM1 owing to amplification of chromosome region 18p11.32, and showed that this increase in Yes expression conferred resistance to different types of HER2-targeted drugs. In this study, we used comprehensive research strategies, including establishment of various cell lines stably transfected with wild-type or activated mutant version of YES1, to establish that activated Yes leads to resistance. This work provides novel insights into the role of Yes in the drug-resistance process, supported by solid evidence.
The YES1 gene maps to chromosome region 18p11.32, which is reported to be frequently and extensively amplified in different cancers.40,41,42,43 In particular, TYMS, another gene that is closely linked to cancer, is located very near YES1 in the 18p11.32 region. TYMS catalyses the methylation of dUMP to dTMP, and is a target for the chemotherapy drug 5-FU, one of the most commonly used drugs to treat cancer, including breast cancer.44 Notably, it has been found that YES1 and TYMS are usually co-amplified and consequently co-overexpressed in cancer,43,45 findings similar to those of this study. Because patients treated with 5-FU are reported to exhibit a significantly greater frequency of TYMS amplification,46 YES1 copy numbers should be determined in patients pretreated with 5-FU before initiating HER2-targeted therapy, given the current study’s finding that YES1 amplification confers resistance to HER2-targeted drugs. Moreover, several regimens of HER2-targeted drugs (including T-DM1) in combination with 5-FU or capecitabine (5-FU pro-drug) have been studied in clinical trials.47,48 Specifically, trastuzumab + 5-FU/capecitabine + cisplatin has been approved as a first-line standard of care for HER2-positive metastatic gastric/gastroesophageal junction adenocarcinoma, and lapatinib + capecitabine has been approved for HER2-positive advanced or metastatic breast cancer with certain prior therapies, including an anthracycline, a taxane, or trastuzumab.49 Although these combinations exhibit enhanced antitumour activity, it is worth noting that under the dual selective pressure of HER2-targeted drugs and fluorouracil/capecitabine, there is a higher probability that amplification of chromosome region 18p11.32, where YES1 and TYMS genes reside, will occur in these patients. Thus, monitoring copy numbers of these genes in the clinic is essential for obtaining additional statistical information and to avoid possible resistance in these patients. Interestingly, chemotherapies, such as adriamycin and taxol, displayed different sensitivity in YES1 amplification (BT-474/R1-7) cells (Supplementary Fig. 4), and further investigation is warranted.
Dasatinib, which mainly targets SFKs and Abl, has been approved by the FDA for the treatment of chronic myeloid leukaemia and Philadelphia chromosome-positive acute lymphoblastic leukaemia. Despite being used clinically for many years, dasatinib has not yet been approved for the treatment of solid tumours; notable in this context, results from several clinical trials of dasatinib on different types of solid tumours have not been encouraging.50,51,52 However, it should be noted that most of these clinical trials were performed in unselected patients.50,51,52 In the current study, we demonstrated that cells with YES1 amplification were remarkably more sensitive to dasatinib, which considerably reversed resistance to HER2-targeted drugs, even at low concentrations. Thus, YES1 may potentially serve as a biomarker for the efficacy of dasatinib; moreover, dasatinib may be beneficial as monotherapy or mechanism-based combination therapy in solid tumours with YES1 amplification. Further exploration of the therapeutic opportunities of dasatinib in solid tumours may prove promising.
In summary, we report a novel mechanism in which amplification of chromosome region 18p11.32, where the YES1 gene resides, leads to overexpression of the SFK member Yes in cells incubated long term with T-DM1, and confers cross-resistance to HER2-targeted drugs. We further suggest that combined inhibition of HER2 and SFK could be a promising treatment strategy for overcoming resistance to HER2-targeted drugs. These findings provide novel insights into the treatment of resistance to HER2-targeted drugs, but still need clinical verification.
References
Moasser, M. M. Targeting the function of the HER2 oncogene in human cancer therapeutics. Oncogene 26, 6577–6592 (2007).
Escriva-de-Romani, S., Arumi, M., Bellet, M. & Saura, C. HER2-positive breast cancer: current and new therapeutic strategies. Breast 39, 80–88 (2018).
Rexer, B. N. & Arteaga, C. L. Intrinsic and acquired resistance to HER2-targeted therapies in HER2 gene-amplified breast cancer: mechanisms and clinical implications. Crit. Rev. Oncog. 17, 1–16 (2012).
Doroshow, D. B. & LoRusso, P. M. Trastuzumab emtansine: determining its role in management of HER2 + breast cancer. Future Oncol. 14, 589–602 (2018).
Lewis Phillips, G. D., Li, G., Dugger, D. L., Crocker, L. M., Parsons, K. L., Mai, E. et al. Targeting HER2-positive breast cancer with trastuzumab-DM1, an antibody-cytotoxic drug conjugate. Cancer Res. 68, 9280–9290 (2008).
Junttila, T. T., Li, G., Parsons, K., Phillips, G. L. & Sliwkowski, M. X. Trastuzumab-DM1 (T-DM1) retains all the mechanisms of action of trastuzumab and efficiently inhibits growth of lapatinib insensitive breast cancer. Breast Cancer Res. Treat. 128, 347–356 (2011).
Welslau, M., Dieras, V., Sohn, J. H., Hurvitz, S. A., Lalla, D., Fang, L. et al. Patient-reported outcomes from EMILIA, a randomised phase 3 study of trastuzumab emtansine (T-DM1) versus capecitabine and lapatinib in human epidermal growth factor receptor 2-positive locally advanced or metastatic breast cancer. Cancer 120, 642–651 (2014).
Dieras, V., Miles, D., Verma, S., Pegram, M., Welslau, M., Baselga, J. et al. Trastuzumab emtansine versus capecitabine plus lapatinib in patients with previously treated HER2-positive advanced breast cancer (EMILIA): a descriptive analysis of final overall survival results from a randomised, open-label, phase 3 trial. Lancet Oncol. 18, 732–742 (2017).
Collins, D. M., Bossenmaier, B., Kollmorgen, G., Niederfellner, G. Acquired resistance to antibody-drug conjugates. Cancers 11, 394 (2019).
Mercogliano, M. F., De Martino, M., Venturutti, L., Rivas, M. A., Proietti, C. J., Inurrigarro, G. et al. TNFalpha-induced mucin 4 expression elicits trastuzumab resistance in HER2-positive breast cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 23, 636–648 (2017).
Wang, H., Wang, W., Xu, Y., Yang, Y., Chen, X., Quan, H. et al. Aberrant intracellular metabolism of T-DM1 confers T-DM1 resistance in human epidermal growth factor receptor 2-positive gastric cancer cells. Cancer Sci. 108, 1458–1468 (2017).
Rios-Luci, C., Garcia-Alonso, S., Diaz-Rodriguez, E., Nadal-Serrano, M., Arribas, J., Ocana, A. et al. Resistance to the antibody-drug conjugate T-DM1 is based in a reduction in lysosomal proteolytic activity. Cancer Res. 77, 4639–4651 (2017).
Loganzo, F., Tan, X., Sung, M., Jin, G., Myers, J. S., Melamud, E. et al. Tumor cells chronically treated with a trastuzumab-maytansinoid antibody-drug conjugate develop varied resistance mechanisms but respond to alternate treatments. Mol. Cancer Ther. 14, 952–963 (2015).
Saatci, O., Borgoni, S., Akbulut, O., Durmus, S., Raza, U., Eyupoglu, E. et al. Targeting PLK1 overcomes T-DM1 resistance via CDK1-dependent phosphorylation and inactivation of Bcl-2/xL in HER2-positive breast cancer. Oncogene 37, 2251–2269 (2018).
Wang, L., Wang, Q., Gao, M., Fu, L., Li, Y., Quan, H. et al. STAT3 activation confers trastuzumab-emtansine (T-DM1) resistance in HER2-positive breast cancer. Cancer Sci. 109, 3305–3315 (2018).
Wang, Q., Quan, H., Zhao, J., Xie, C., Wang, L. & Lou, L. RON confers lapatinib resistance in HER2-positive breast cancer cells. Cancer Lett. 340, 43–50 (2013).
Rosenbluh, J., Nijhawan, D., Cox, A. G., Li, X., Neal, J. T., Schafer, E. J. et al. beta-Catenin-driven cancers require a YAP1 transcriptional complex for survival and tumorigenesis. Cell 151, 1457–1473 (2012).
Wang, L., Yang, C., Xie, C., Jiang, J., Gao, M., Fu, L. et al. Pharmacologic characterization of fluzoparib, a novel poly(ADP-ribose) polymerase inhibitor undergoing clinical trials. Cancer Sci. 110, 1064–1075 (2019).
Wang, L., Xu, Y., Fu, L., Li, Y. & Lou, L. (5R)-5-hydroxytriptolide (LLDT-8), a novel immunosuppressant in clinical trials, exhibits potent antitumor activity via transcription inhibition. Cancer Lett. 324, 75–82 (2012).
Barok, M., Joensuu, H. & Isola, J. Trastuzumab emtansine: mechanisms of action and drug resistance. Breast Cancer Res. 16, 209 (2014).
Montero, J. C., Seoane, S., Ocana, A. & Pandiella, A. Inhibition of SRC family kinases and receptor tyrosine kinases by dasatinib: possible combinations in solid tumors. Clin. Cancer Res. 17, 5546–5552 (2011).
Hantschel, O., Rix, U. & Superti-Furga, G. Target spectrum of the BCR-ABL inhibitors imatinib, nilotinib and dasatinib. Leuk. Lymphoma 49, 615–619 (2008).
Kim, L. C., Song, L. & Haura, E. B. Src kinases as therapeutic targets for cancer. Nat. Rev. Clin. Oncol. 6, 587–595 (2009).
Thomas, S. M. & Brugge, J. S. Cellular functions regulated by Src family kinases. Annu. Rev. Cell Dev. Biol. 13, 513–609 (1997).
Zhang, S., Huang, W. C., Li, P., Guo, H., Poh, S. B., Brady, S. W. et al. Combating trastuzumab resistance by targeting SRC, a common node downstream of multiple resistance pathways. Nat. Med. 17, 461–469 (2011).
Albertson, D. G. Gene amplification in cancer. Trends Genet. 22, 447–455 (2006).
El-Hashim, A. Z., Khajah, M. A., Renno, W. M., Babyson, R. S., Uddin, M., Benter, I. F. et al. Src-dependent EGFR transactivation regulates lung inflammation via downstream signaling involving ERK1/2, PI3Kdelta/Akt and NFkappaB induction in a murine asthma model. Sci. Rep. 7, 9919 (2017).
Le, X. F. & Bast, R. C. Jr. Src family kinases and paclitaxel sensitivity. Cancer Biol. Ther. 12, 260–269 (2011).
Johnson, F. M. & Gallick, G. E. SRC family nonreceptor tyrosine kinases as molecular targets for cancer therapy. Anticancer Agents Med. Chem. 7, 651–659 (2007).
Fang, Z., Yin, S., Sun, R., Zhang, S., Fu, M., Wu, Y. et al. miR-140-5p suppresses the proliferation, migration and invasion of gastric cancer by regulating YES1. Mol. Cancer 16, 139 (2017).
Shen, Y., Chen, F. & Liang, Y. MicroRNA-133a inhibits the proliferation of non-small cell lung cancer by targeting YES1. Oncol. Lett. 18, 6759–6765 (2019).
Hamanaka, N., Nakanishi, Y., Mizuno, T., Horiguchi-Takei, K., Akiyama, N., Tanimura, H. et al. YES1 is a targetable oncogene in cancers harboring YES1 gene amplification. Cancer Res. 79, 5734–5745 (2019).
Wheeler, D. L., Iida, M., Kruser, T. J., Nechrebecki, M. M., Dunn, E. F., Armstrong, E. A. et al. Epidermal growth factor receptor cooperates with Src family kinases in acquired resistance to cetuximab. Cancer Biol. Ther. 8, 696–703 (2009).
Lee, L. F., Louie, M. C., Desai, S. J., Yang, J., Chen, H. W., Evans, C. P. et al. Interleukin-8 confers androgen-independent growth and migration of LNCaP: differential effects of tyrosine kinases Src and FAK. Oncogene 23, 2197–2205 (2004).
Riggins, R. B., Thomas, K. S., Ta, H. Q., Wen, J., Davis, R. J., Schuh, N. R. et al. Physical and functional interactions between Cas and c-Src induce tamoxifen resistance of breast cancer cells through pathways involving epidermal growth factor receptor and signal transducer and activator of transcription 5b. Cancer Res. 66, 7007–7015 (2006).
Chen, T., Pengetnze, Y. & Taylor, C. C. Src inhibition enhances paclitaxel cytotoxicity in ovarian cancer cells by caspase-9-independent activation of caspase-3. Mol. Cancer Ther. 4, 217–224 (2005).
George, J. A., Chen, T. & Taylor, C. C. SRC tyrosine kinase and multidrug resistance protein-1 inhibitions act independently but cooperatively to restore paclitaxel sensitivity to paclitaxel-resistant ovarian cancer cells. Cancer Res. 65, 10381–10388 (2005).
Fan, P. D., Narzisi, G., Jayaprakash, A. D., Venturini, E., Robine, N., Smibert, P. et al. YES1 amplification is a mechanism of acquired resistance to EGFR inhibitors identified by transposon mutagenesis and clinical genomics. Proc. Natl Acad. Sci. USA 115, E6030–E6038 (2018).
Ichihara, E., Westover, D., Meador, C. B., Yan, Y., Bauer, J. A., Lu, P. et al. SFK/FAK Signaling Attenuates Osimertinib Efficacy in Both Drug-Sensitive and Drug-Resistant Models of EGFR-Mutant Lung Cancer. Cancer Res. 77, 2990–3000 (2017).
Hermsen, M., Guervos, M. A., Meijer, G., Baak, J., van Diest, P., Marcos, C. A. et al. New chromosomal regions with high-level amplifications in squamous cell carcinomas of the larynx and pharynx, identified by comparative genomic hybridization. J. Pathol. 194, 177–182 (2001).
Hinze, R., Schagdarsurengin, U., Taubert, H., Meye, A., Wurl, P., Holzhausen, H. J. et al. Assessment of genomic imbalances in malignant fibrous histiocytomas by comparative genomic hybridization. Int J. Mol. Med. 3, 75–79 (1999).
Sonoda, G., Palazzo, J., du Manoir, S., Godwin, A. K., Feder, M., Yakushiji, M. et al. Comparative genomic hybridization detects frequent overrepresentation of chromosomal material from 3q26, 8q24, and 20q13 in human ovarian carcinomas. Genes Chromosomes Cancer 20, 320–328 (1997).
Nakakuki, K., Imoto, I., Pimkhaokham, A., Fukuda, Y., Shimada, Y., Imamura, M. et al. Novel targets for the 18p11.3 amplification frequently observed in esophageal squamous cell carcinomas. Carcinogenesis 23, 19–24 (2002).
Marsh, S. Thymidylate synthase pharmacogenetics. Invest. N. Drugs 23, 533–537 (2005).
Wang, W., Marsh, S., Cassidy, J. & McLeod, H. L. Pharmacogenomic dissection of resistance to thymidylate synthase inhibitors. Cancer Res. 61, 5505–5510 (2001).
Watson, R. G., Muhale, F., Thorne, L. B., Yu, J., O’Neil, B. H., Hoskins, J. M. et al. Amplification of thymidylate synthetase in metastatic colorectal cancer patients pretreated with 5-fluorouracil-based chemotherapy. Eur. J. Cancer 46, 3358–3364 (2010).
Krop, I. E., Lin, N. U., Blackwell, K., Guardino, E., Huober, J., Lu, M. et al. Trastuzumab emtansine (T-DM1) versus lapatinib plus capecitabine in patients with HER2-positive metastatic breast cancer and central nervous system metastases: a retrospective, exploratory analysis in EMILIA. Ann. Oncol. 26, 113–119 (2015).
Bang, Y. J., Van Cutsem, E., Feyereislova, A., Chung, H. C., Shen, L., Sawaki, A. et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 376, 687–697 (2010).
Moy, B., Kirkpatrick, P., Kar, S. & Goss, P. Lapatinib. Nat. Rev. Drug Discov. 6, 431–432 (2007).
Mayer, E. L. & Krop, I. E. Advances in targeting SRC in the treatment of breast cancer and other solid malignancies. Clin. Cancer Res. 16, 3526–3532 (2010).
Miller, A. A., Pang, H., Hodgson, L., Ramnath, N., Otterson, G. A., Kelley, M. J. et al. A phase II study of dasatinib in patients with chemosensitive relapsed small cell lung cancer (Cancer and Leukemia Group B 30602). J. Thorac. Oncol. 5, 380–384 (2010).
Sharma, M. R., Wroblewski, K., Polite, B. N., Knost, J. A., Wallace, J. A., Modi, S. et al. Dasatinib in previously treated metastatic colorectal cancer: a phase II trial of the University of Chicago Phase II Consortium. Invest. N. Drugs 30, 1211–1215 (2012).
Acknowledgements
Not applicable.
Author information
Authors and Affiliations
Contributions
L.W., H.Q. and L.L. conceived and designed the study; L.W., Q.W. and P.X. developed the methodologies and acquired the data; L.F., Y.L. and H.F. performed in vivo experiments; L.W. and L.L. wrote and revised the paper. All authors read and approved the final paper.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Animal studies were carried out in accordance with guidelines of the Institutional Animal Care and Use Committee at the Shanghai Institute of Materia Medica, Chinese Academy of Sciences. The human BT-474 and SK-OV-3 cell lines were obtained from the American Type Culture Collection (Manassas, VA, USA).
Consent to publish
N/A
Data availability
The data generated during the current study are available from the corresponding author upon reasonable request.
Competing interests
The authors declare no competing interests.
Funding information
This work was supported by National Natural Science Foundation of China (№ 81502636); the Shanghai Science and Technology Committee (№ 18DZ2293200); and the Yunnan Provincial Science and Technology Department (№ 2017ZF010).
Additional information
Note This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution 4.0 International (CC BY 4.0).
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, L., Wang, Q., Xu, P. et al. YES1 amplification confers trastuzumab–emtansine (T-DM1) resistance in HER2-positive cancer. Br J Cancer 123, 1000–1011 (2020). https://doi.org/10.1038/s41416-020-0952-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-020-0952-1
This article is cited by
-
A renaissance for YES in cancer
Oncogene (2023)